|
December 2002, Volume 24, No. 12
|
Case Report
|
|||
Overbundling as a cause of fever in a 6-day old boyY M Fu 符儒明,D K K Ng 吳國強,C K L Kwok 郭嘉莉 HK Pract 2002;24:606-607 Summary Fever is a common symptom in paediatric practice. Particular attention is given to infants less than 3-month old because of higher risk of bacteraemia and meningitis at this age. Overbundling is one of the causes of high temperature in infants. Careful history and observation lead to prompt diagnosis, avoidance of unnecessary investigations and treatment. This case report shows an example of management of overbundling in a 6-day-old neonate. 摘要 發燒是兒童常見的病徵。對三個月以下的嬰兒要格外注意,因為在這個年齡,患菌血症和腦膜炎的機會較高。過度包裹也是嬰兒體溫過高的原因之一。仔細的詢問病史和觀察,可以迅速做出診斷並避免不必要的檢查和治療。本文報告一例出生後六天包裹過度 的新生兒的處理。 Introduction A neonate with fever is a challenging problem to a paediatrician. Paradoxically, a sick-looking neonate is more straightforward to manage than a febrile neonate who looks well. Hence, febrile neonates usually receive a full sepsis work-up, including lumbar puncture. They are often given empirical treatment with antibiotics.1 Overbundling, a cause of fever in infants, is not often included in the differential diagnoses of neonate with fever.2 This report serves to highlight the management of a febrile neonate as a result of overbundling. Case report
A 6-day old Indian boy was admitted to the paediatric ward for management of fever
within 24 hours of discharge from the postnatal ward. His temperature was not recorded
at home. Rectal temperature was 38.9
On admission, the baby was wrapped with 3 layers of thick clothing (Figure 1).
His parents were brought up in the Northern part of India where the temperature
in October was about 15-20 Discussion
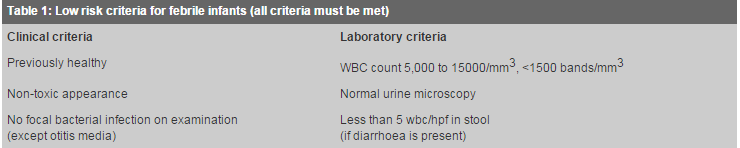
Environmental causes of neonatal fever, i.e. rectal temperature over 38 The current practice adopted for fever in infants of less than 28 days of life is hospitalisation for evaluation of sepsis by performing lumbar puncture, urine and blood culture, and complete blood count.1,2 However, for an infant of less than 3 months old who met the low risk clinical and laboratory criteria, the probability of having serious bacterial infection is only 0.2%4 (Table 1). With the evidence of overbundling and absence of fever after removal of excess clothing, lumbar puncture and blood culture are probably not necessary. In a study of a large number of full-term infants, a raised body temperature was found in 1% in the early neonatal period. Of these, 10% had bacterial infections and 90% were due to environmental causes.5
Conclusion This case illustrates the importance of careful observation and detailed history in evaluating an infant with fever. This helps to avoid unnecessary investigations and treatment in case of overbundling.
Y M Fu, MBBS(HK)
D K K Ng, M Med Sc, FHKAM(Paed), FHKCPaed Senior Medical Officer, Department of Paediatrics, Kwong Wah Hospital. Correspondence to: Dr D K K Ng, , Department of Paediatrics, Kwong Wah Hospital, Waterloo Road, Kowloon, Hong Kong. References
|
||||