|
July 2007, Volume 29, No. 7
|
Case Report
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Two asymptomatic patients with hyponatraemiaCarroll K L Chan 陳家樂, Kin-sang Ho 何健生, Wai-man Chan 陳慧敏 HK Pract 2007;29:278-281 Summary Hyponatraemia is not uncommonly found in routine blood investigation in asymptomatic patients. In this article, we report two cases of patients with asymptomatic hyponatraemia in general practice. The general approach by family physician to patients with hyponatraemia is also discussed. 摘要 無症狀病人的血常規檢查發現低鈉血症並不罕見。本文報告2例基層醫療中無症狀低鈉血症的病例,並討論家庭醫生一般的處理方法。 Introduction Elderly health centres of Elderly Health Service provide comprehensive health assessment for our elderly members aged above 65. Routine blood investigation is one part of our health assessment. Hyponatraemia is not uncommonly found in routine blood investigation. In this article, we would like to use two elderly patients of our centre to illustrate the general approach to manage patients with asymptomatic hyponatraemia. Case 1 M/76 Past Health
Thyroidectomy for benign thyroid nodule 20+ years ago He attended our elderly health centre for health assessment in 2005. He was asymptomatic. We found the following on routine blood investigation:
So, we rechecked the sodium and potassium levels and found the following:
Patient was not on diuretic or any medication. He was clinically not dehydrated and no ankle oedema was found. Further investigation revealed:
The low serum osmolality indicated that the patient had relative water excess. Further
detailed history found that he did not have any history of psychiatric disorder
and did not have features of compulsive drinking. However, he had started drinking
more than 2 L of water per day after his TURP operation because he was told by his
Urologist to drink more water after the operation. Ever since then, he had been
drinking this amount of water until this health assessment. As such, over-compliance
to doctor's advice appeared to be the only reason for his drinking of excessive
amount of water and hyponatraemia! We then advised him to drink an appropriate amount
of water and the subsequent plasma sodium level returned to normal.
Case 2 F/75 Past Health
Right ear drum perforation with right conductive hearing loss followed up by ENT
specialist She attended our elderly health centre for health assessment and was also asymptomatic. We found the following on routine blood investigation:
We rechecked the sodium and potassium levels and found the following:
She was clinically not dehydrated and no ankle oedema was found. Further investigation revealed:
Serum osmolality 268 mOsmol/kg (275-295) In this case, urine sodium concentration was inappropriately high as compared with low serum osmolality. So the clinical diagnosis of syndrome of inappropriate antidiuretic hormone ( SIADH) was made. Further detailed history found that she was prescribed with escitalopram by her family physician and there was no other medication. CXR was done to rule out possible chest pathology known to be associated with SIADH and the result was found to be unremarkable. Her mood was stable and the Geriatric Depression Score (GDS) done in our centre was 3. A letter was issued to inform her family physician of our finding. Escitalopram was subsequently withdrawn and her plasma sodium level resumed to normal later. Diagnosis: SSRI-related SIADH Discussion During health assessment or body check, family physicians usually arrange routine blood investigations for their patients; and incidental findings of hyponatraemia are not uncommon. Common causes of hyponatraemia include laboratory error and due to diuretic effect. Therefore the initial management of hyponatraemia should include rechecking the serum sodium to confirm hyponatraemia as well as reviewing the drug history. Common diuretics include Lasix, Dyazide, Moduretic, Natrilix, Spironolactone. Less common "diuretics" include carbonic anhydrase inhibitor e.g. acetazolamide (Diamox). After confirming hyponatraemia and excluding the use of diuretic, we should assess the hydration status of the patient to look out for any accountable causes.1-5
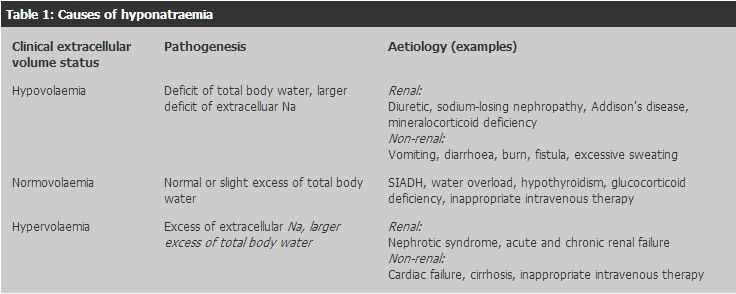
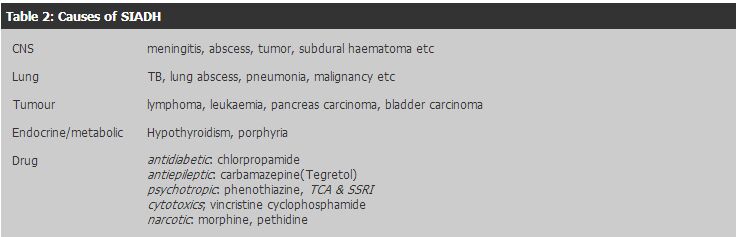
If the patient is dehydrated i.e. sodium depleted, we should consider extra-renal causes like vomiting, diarrhoea, fistula, or low sodium intake. In these cases the urine sodium should be low (<20 mmol/L) indicating that there is no excessive renal loss of sodium as a cause. If the patient's urine sodium is high (>20 mmol/L), we should consider excessive renal sodium loss such as use of diuretic, sodium-losing nephropathy, Addison's disease. If patient is oedematous, we should consider nephrotic syndrome, cirrhosis, and heart failure as cause of hyponatraemia. If patient is not dehydrated, we should also think of compulsive drinking or overdrinking of water when urine sodium is low as in Case 1 and we have to document this from the history. When urine sodium or urine osmolality is high and yet serum osmolality is inappropriately low, we should then think of the syndrome of inappropriate antidiuretic hormone (SIADH). SIADH is characterized1,3,4 by:
t should be noted that hyponatraemia related to SIADH has been associated with all types of antidepressants. However, it has been reported more frequently with SSRI than with other antidepressants and is also more common in elderly patients6 as seen in our Case 2 patient. Uncommonly, the combination of hyponatremia and normal plasma osmolality can be caused by pseudohyponatraemia.1,4 Severe hypertriglyceridemia and hyperproteinemia are two causes of this condition in patients with pseudohyponatraemia. These patients are usually euvolemic. Conclusion The general approach to asymptomatic hyponatraemia include rechecking blood to confirm hyponatraemia, reviewing medication and past health as well as assessing hydration status to look out for common reversible causes. Besides, checking plasma and urine osmolality is also important to ascertain causes so that family physician can manage the underlying cause accordingly. Last but not the least, in general practice, family physicians should always beware of iatrogenic cause. Key messages
Carroll K L Chan, MBBS (HK), FHKCFP, FRACGP, FHKAM (Family Medicine)
Medical Officer Elderly Health Service, Department of Health. Kin-sang Ho, MBBS (HK), FHKAM (Medicine), FHKAM (Family Medicine) Consultant (Family Medicine), Elderly Health Service, Department of Health. Wai-man Chan, MBBS (HK), MPH (USA), FHKAM (Community Medicine) Assistant Director of Health Family and Elderly Health Services, Department of Health. Correspondence to : Dr Carroll Ka-lok Chan, Shaukeiwan Elderly Health Centre, 8 Chai Wan Road, Shaukeiwan, Hong Kong.
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||