December 2010, Volume 32, No. 4 |
Case Report
|
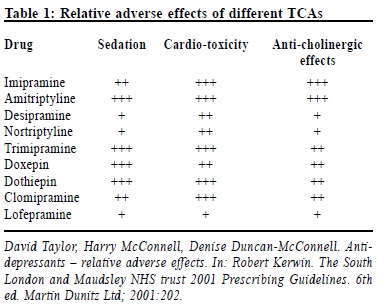
A young man with asymptomatic sinus tachycardiaTammy KW Tam 譚嘉渭, Luke C Y Tsang 曾昭義 HK Pract 2010;32:179-182 Summary Tricyclic antidepressants (TCA) are commonly prescribed in general practice for treating affective and anxiety disorders. Imipramine is the prototypical drug of the class. We report a suspected case of cardiotoxicity with chronic use of imipramine in a young man, which resulted in sinus tachycardia and persistent elevation of blood pressure. The abnormal blood pres sure and electrocardiogram tracings resolved gradually after stopping imipramine. We also discuss the clinical features and management of acute and chronic TCA overdoses, and highlight the precautions in prescribing TCAs, particularly in concomitant use with other medications. 摘要 三環抗抑鬱藥(TCA)是全科醫學醫生經常處方的治療情感障礙和焦慮症藥物丙咪嗪是此類的原型藥。本文報告了一例年輕男士因長期服用丙咪嗪而導致毒性影響心臟的可疑病例,表現為竇性心動過速和持續血壓升高。停服丙咪嗪後,血壓和心電圖參數逐漸恢復正常。本文還討論了急、慢性三環抗抑鬱藥過量的臨床表現及處理方法,並強調了處方三環抗抑鬱藥,尤其是與其他藥物同時使用的注意事項。 Introduction Depressive disorder is commonly encountered in general practice. The World Health Report published in 2004 had estimated that unipolar depression was the third leading cause of burden of disease.1 Primary care doctors are often the first point of contact with patients. And by having a continuous relationship with patients, primary care physicians have played an important role in promoting both physical and psychological health status of the general population. It is imperative for them to be vigilant and competent in diagnosing and managing depression in daily practice. Physicians should be alert to the side effect profiles of antidepressant medications, particularly for patients with multiple co-morbidities and polypharmacy, so that the risk of drug toxicity or disastrous drug-drug interactions can be minimized. A case report A 35-year old man was incidentally found to have sinus tachycardia of 140 per minute during his pre-employment health check in early April 2009. He did not notice any palpitation, shortness of breath, chest pain, facial flushing, headache or dizziness. And there was no neck swelling, hand tremor, heat intolerance or weight loss. In 2001, the patient was diagnosed to have major depression and put on imipramine, a tricyclic anti-depressant. After the initial period of drug titration, his condition was stabilized by using the dosage of 50 mg daily. He was unable to wean off the drug. In January 2009, his depression illness was exacerbated due to unemployment and, not having informed his doctor, he stepped up the dosage of imipramine to 100 mg daily. His mood and sleep improved apparently after increasing the drug dosage, and this had not resulted in any noticeable adverse effects. Apart from depression, the patient did not have other significant medical illnesses. He was a nonsmoker and non-drinker. He was not taking any concomitant medications, herbal preparations, or caffeine-containing beverages. On examination, his general condition was good. His blood pressure was elevated in the range of 145-156/80-85 mmHg, with a regular pulse rate of 120 beats per minute. Physical examination was otherwise unremarkable. An electrocardiogram was performed that showed sinus tachycardia of 118 per min. Laboratory-test results including complete blood picture, renal, liver and thyroid functions, as well as urinalysis were all normal. Drug-induced sinus tachycardia and hypertension was suspected. Imipramine was gradually tailed off, and substituted with fluoxetine in late April 2009. In July 2009, his blood pressure was normalized to 116/72 mmHg and heart rate returned to 75 per minute. His mood condition remained stable while on fluoxetine 20mg daily. Discussion Tricyclic antidepressant (TCA) is commonly prescribed in general practice for treating mood and anxiety disorders. TCA is so named because of the characteristic 3-ring nucleus. Imipramine is the prototypical drug of the class, and is used in treatment of depression, as well as attention deficit disorder and nocturnal enuresis in children. Complications arising from acute intoxication of TCA include neurological symptoms such as agitation, restlessness, seizure, respiratory depression and coma. Cardiovascular effects of acute intoxication include orthostatic hypotension, hypertension, myocardial depression, tachycardia, intractable ventricular tachycardia or fibrillation, and sudden death.2 The mechanism of action of TCAs involves the noradrenergic properties of catecholamines. Some authors speculated that they could be due to drug’s ability to bind directly to the cardiac sodium channels.3 The mortality rate of TCA poisoning is 2% - 3%,2 with cardiotoxicity being the major cause of mortality. Chronic use of TCA is associated with orthostatic hypotension, tremors, tachycardia, dry mouth, urinary retention and other symptoms of anti-cholinergic effect. Table 1 illustrates the relative adverse effects of different TCAs.
We report a suspected case of adverse drug reaction with chronic use of imipramine. The patient had been constantly taking imipramine at dosage from 25 mg daily to 100 mg daily over 8 years for major depression. He presented with persistent elevation of blood pressure and increase in heart rate, with electrocardiogram showing sinus tachycardia of around 120 beats per minute. All these abnormalities resolved gradually after a few months of stopping imipramine. Electrocardiographic changes observed with TCA overdosage include all degrees of conduction block, sinus tachycardia, ST depression, non-specific T-wave changes, and widened QRS intervals. Some studies suggested that QRS duration is an indicator of the clinical severity of TCA poisoning, and seems to correlate well with the clinical manifestations.4 But the relationship between TCA plasma levels and clinical toxicity is unclear. Despite the fact that a previous study had monitored the serial plasma TCA levels in 40 overdosed patients and found that levels of 1000ng/ml or more are associated with seizure toxicity, serious cardiac arrhythmias and seizures may still occur with normal serum level.4 Management of acute TCA poisoning depends on the neurological signs and ECG characteristics.5 It generally involves the use of gastric lavage, and installation of activated charcoal to minimize further drug absorption.6-8 Alkalinization of blood by sodium bicarbonate will help in narrowing the QRS complex, improving conduction and decreasing arrhythmias.5,6,8 Seizures are best managed by diazepam or phenytoin, rather than barbiturates, as they are less likely to aggravate respiratory depression.7 Metabolism of imipramine is primarily in the liver. The plasma half-life is about 9-24 hours. With prompt management, ECG abnormalities are expected to revert to normal after 2-3 days. In general practice, the initiation of TCAs requires careful patient assessment, including a thorough medical history, in particular any history of cardiac arrhythmia, heart disease or syncope, or family history of heart disease or sudden cardiac death. Baseline blood pressure and pulse rate should be recorded, and a baseline 12-lead electrocardiogram should be obtained, with any significant arrhythmia, conduction disturbances or prolonged QTc interval noted. In chronic administration of tricyclic antidepressants, it is important for patients to be aware of the potential cardiac side effects, and have their blood pressure, pulse rate and electrocardiogram regularly monitored. Clinicians should be alert to the danger of adding other medications that can lengthen the QTc intervals, to avoid drug interactions with devastating consequences. Examples of agents which can affect the CYP IA1/2 cytochrome (the major site for demethylation of tricyclics) include inhibitors (ciprofloxacin, theophylline, and grapefruit) and inducers (carbamazepine, caffeine, omeprazole, and cigarette smoking).9 Some other medications with possible drug interactions with TCAs are alcohol, anti-cholinergics (including neuroleptics, etc.), MAOIs, and sympathomimetics. In managing suspected cardiotoxicity associated with chronic use of TCAs, as in this case, the culprit drug should be withdrawn, preferably gradually, to prevent discontinuation symptoms. Nevertheless, the drug should be withdrawn more abruptly if there are serious adverse effect e.g. cardiac arrhythmia.10 When swapping from one antidepressant to another, cross-tapering is preferred, where the dose of the poorly tolerated drug is slowly reduced while the new drug is slowly introduced.10 Potential dangers of simultaneously administering two antidepressants include pharmacodynamic interactions (serotonin syndrome, hypotension, drowsiness) and pharmacokinetic interactions (e.g. elevation of TCA plasma levels by some SSRIs).10 Moreover, in daily practice, patients are commonly seen by multiple doctors for the same or different diseases. Effective communication across different healthcare settings, by good medical record keeping and shared medical record system, is pivotal to enable early diagnosis and management of diseases, and to enhance patient safety and improve treatment outcomes. Conclusion TCAs are commonly prescribed in general practice. It requires careful evaluation of patients before and after their initiation and careful monitoring by history, physical examination (blood pressure and pulse rate), and electrocardiogram, once their use is implemented. Caution should be exercised in concomitant use of other medications to avoid disastrous drug-drug interactions. Early recognition and prompt management of adverse effects is important to improve patient outcomes. Key messages
Tammy K W Tam, MBChB (CUHK), MMedSc (HKU), FRACGP, FHKAM (Fam Med) Luke C Y Tsang, MBBS (NSW), DFM (CUHK), FRACGP, FHKAM (Fam Med) Correspondence to: Dr Tammy K W Tam, Kowloon Families Clinic, 6/F Yaumatei Polyclinic, 145 Battery Street, Yaumatei, Kowloon, Hong Kong SAR. References
|
|