December 2012, Volume 34, No. 4 |
Original Article
|
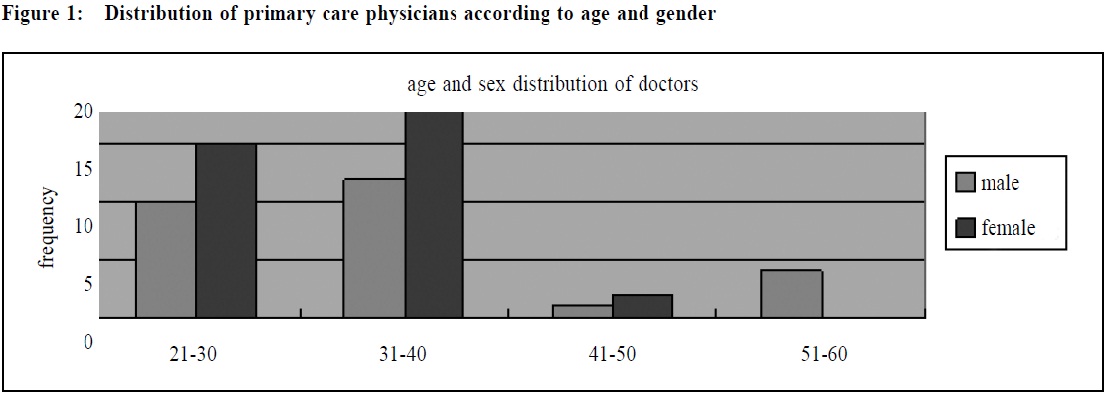
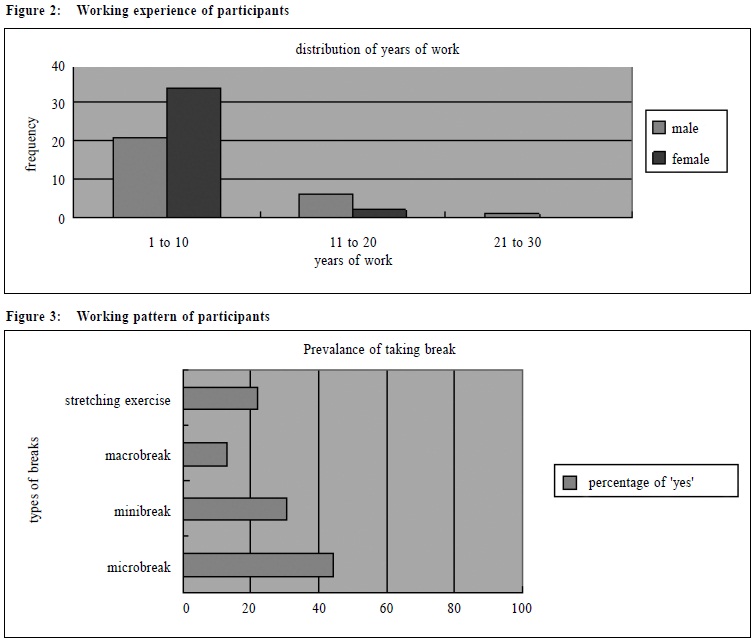
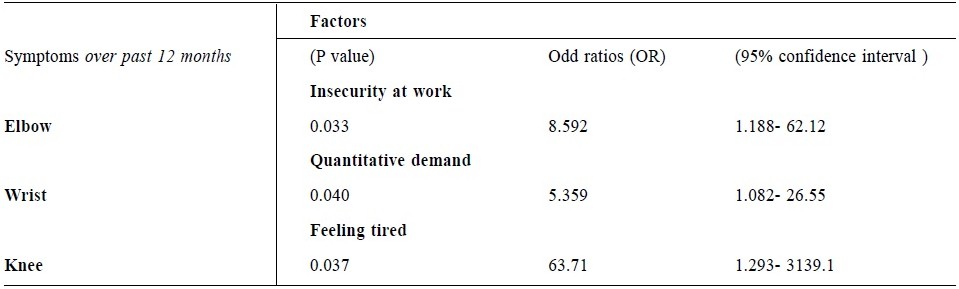
The prevalence and the work related predictors of musculoskeletal symptoms of doctors working in a general out-patient clinic settingCatherine TM Lam 林德敏, Chun-fat Lo 羅春發, Yuk-kwan Yiu 姚玉筠 HK Pract 2010;32:160-171 Summary Objective: The aim of this study is to determine the prevalence and the work related predictors of musculoskeletal (MSK) symptoms of doctors working in a general out-patient clinic setting. Design: Cross sectional survey Subjects: Primary care out-patient clinics in Kowloon West Cluster (KWC), Hospital Authority, Hong Kong. All 127 full-time doctors working in our general out-patient clinics of the Department of Family Medicine, KWC were included during the study period from 23rd March to 31st March, 2009. The exclusion criteria excluded one administrative staff and a part-time doctor in the Department. Sixty eight doctors completed standardized questionnaires. There were 28 (41.2%) male doctors and 36 (52.9%) female doctors. Four (5.9%) questionnaires had missing data on gender. Main outcome measures: The display screen equipment (DSE) conditions of consultation rooms were recorded by a standardized checklist issued by the Labour Department of Hong Kong. Short version of Copenhagen Questionnaire measured psychosocial predictors. The primary outcome measure is the presence of MSK problems as measured by the Standardized Nordic Questionnaire. Results: Using the Nordic Questionnaire, the 12 months prevalence of symptoms of neck, shoulder, wrist, upper and lower back were 69.1%, 53.1%, 44.1%, 48.5% and 48.5% respectively. Job insecurity (OR=8.592, 95% CI 1.188-62.12, p=0.033), quantitative demand (OR=5.359, 95% CI 1.082- 26.55, p=0.040) and feeling tired (OR=63.71, 95% CI 1.293- 3139.1, p=0.037) were significantly associated with the prevalence of elbow, wrist and knee symptoms respectively. Conclusion: With regard to a young working population of doctors, the high prevalence of musculoskeletal problems may pose significant health problems in the future. More resource input for health care programmes that aim at improving staff’s health may be needed, and further research that investigates the relationship between musculoskeletal problems and psychological factors is needed. Keywords: musculoskeletal symptoms, doctors, display screen equipments, general out-patient clinic 摘要 目的:本文評估在普通科門診工作的醫生的肌肉骨骼病徵的患病率及其對這些病症與工作相關的預測指標。 設計:橫切面調查。 對象:2009年3月23至31日期間,香港醫院管理局九龍西聯網家庭醫學部門轄下普通科門診除1位行政人員和1位兼職醫生以外的127位全職醫生。共收回68份完成的問卷,28位男醫生(41.2%)和36位女醫生(52.9%),4份問卷的性別資料缺失。 主要測量內容:以香港勞工處的標準清單記錄診症室內的顯示屏幕設備, 用哥本哈根問卷的簡化版本來量度社會心理條件, 並以標準挪威問卷量度肌肉骨骼病徵作為主要測量內容。 結果:挪威問卷顯示,頸痛、肩痛、手腕痛,上背痛和下背痛的12個月患病率分別是69.1%、53.1%、44.1%、48.5%和48.5%。工作不穩定(OR=8.592,95% CI 1.188 - 62.12,p = 0.033,工作量多(OR= 5.359,95% CI 1.082 - 26.55,p = 0.040)和疲倦感(OR= 63.71,95% CI 1.293 - 3139.1,p = 0.37)與手肘、手腕和膝部病徵有明顯關係。 結論:在年青醫生組群的肌肉骨骼病症高患病率,可引致未來的健康問題。因此,必須增加資源以促進員工健康, 此外還需要就肌肉骨骼病症與社會心理因素之間的關係作進一步的探討。 主要詞彙:肌肉骨骼病徵、醫生、顯示屏幕設備,普通科門診。 Background In Hong Kong, primary care delivered under the government funded Hospital Authority is divided into seven geographical clusters which include a number of districts in Hong Kong. The Kowloon West Cluster (KWC) is one of the largest with 19 out-patient clinics and has a total of 500 staff. There are 127 full-time doctors working as primary care physicians. With rapid blooming of different services and an increasing work load, health issues of staff become an important factor affecting the future development of the Department. The first occupational medicine programme for doctors of the Department was a pilot study using Nordic questionnaire in 2007. It showed a high prevalence of MSK problems among staff of the general outpatient clinics (GOPC). Computerization of consultation record in 2003 and increasing service demand had brought significant changes to working conditions of doctors. Each doctor needed to use DSE for at least seven hours per day. This raised a question on whether there is a high prevalence of MSK problems among doctors and if the change in working conditions is associated with MSK problems of doctors. When performing a literature search on Medline Mesh on musculoskeletal problem, DSE or visual display unit (VDU), literature indicated that employees may suffer from an impairment of general well-being, with symptoms or disorders of the upper extremities due to working conditions.1-4 However, the extent and the factors associated with these problems, its work related causes and the risks leading to symptoms related to the work using DSE have been controversial and thus far somewhat inconclusive results were reported.5,6 As local data on the prevalence of MSK problems is scarce among primary care physicians in Hong Kong, it is unknown whether previous studies1-4 could be generalized to our locality. This study was the first cross sectional study to investigate MSK problems among doctors in the primary care setting in KWC. The primary objective was to study the proportion of primary care physicians suffering from MSK problems. We also evaluated the factors associated with occurrence of these problems in relation to the working conditions. We tested the hypothesis that ergonomic design of DSE and psychosocial factors among physicians are significantly associated with musculoskeletal disorders. Methods This was a cross sectional study using validated and standardized questionnaire to evaluate the proportion of MSK problems among doctors working in the Hospital Authority in Kowloon West Cluster. The surveys were self-administered during the study period from 23rd March, 2009 to 31st March, 2009. Instruments The questionnaire contained items including socio demographic factors (age, gender, years on the job, sports activities, smoking habits), questions on musculoskeletal symptoms, questions about vision (e.g. symptoms at eyes, use of corrective lens or glasses), setup of DSE, general working posture (e.g. reaching out, inclining head and turning trunk) and evaluations of psychosocial factors (e.g. job satisfaction, mental demand, health). The questions on DSE set up were based on the checklist issued by the Labour Department of Hong Kong. This checklist include items regarding display screen, keyboard, desk and arrangement of the DSE and accessories, chair and environmental conditions.7 Questions on musculoskeletal problems were based on the standardized Nordic Questionnaire8 and the questions on psychosocial items were adopted from the short version of Copenhagen Psychosocial Questionnaire.9 The English version of all these surveys were used in this study. Sampling There were 127 full-time doctors working in KWC, as of March, 2009 and questionnaires were sent to all doctors by email. Administrative staff and part time doctors were excluded. The completed questionnaire was mailed back to the author’s office by sealed envelop. We received a total of 68 completed surveys, giving a response rate of 53.5%. Outcome measures and statistical analyses According to current published literature, MSK symptoms related to DSE work may be caused by many factors, including socio demographic, work-related and psychosocial variables.10,11 We erected a priori hypothesis that these factors remained significantly associated with MSK problems in our locality. The major outcome variables were MSK symptoms in different body parts. These included the neck, shoulder, elbow, wrist, upper and lower back, hip, knee and ankle. The predictor variables included the influence of doctor’s factors, DSE conditions, and psychosocial factors on the musculoskeletal symptoms. We performed univariate analysis between each predictor variable with the outcome variables consecutively. All factors with p<0.20 were included in a binary logistic regression model. The choice of predictor variables was hypothesis-driven according to previous studies.10,11 We also checked for the presence of multicolineraity (r>0.80) to ensure robustness of the regression equations. As a result we conducted a total of seven separate regression analyses with each MSK symptom as an outcome variable respectively. The results were presented as odds ratios and 95% confidence intervals. All p values <0.05 were regarded as statistically significant. The Statistical Package for Social Sciences version 11.5 (SPSS Incorporation, Chicago, Illinois) was used to analyze the data. Ethical considerations The study was performed in compliance with the Helsinki Declaration. The aims and methods of the study were agreed by the management committee and the doctors of the Family Medicine Department of KWC. The procedures were coordinated by our nurses and clerical staff. Each survey was anonymous and study participants were assured of survey confidentiality. This study was waived by the Kowloon West Cluster Clinical Research Ethic Committee for ethic approval because it did not include any patient. Results Characteristics of participants There were 74 questionnaires returned, out of 127, with 68 completed, giving a response rate of 53.5%. Of these primary care physicians, there were 28 (41.2%) male doctors and 36 (52.9%) female doctors. Ten (35.7%) male doctors were in the age group of 21 to 30 years old and twelve (42.9%) male doctors were in the age group of 31 to 40 years old. Fifteen (41.7%) female doctors were of 21-30 years old and nineteen (52.8%) were of 31-40 years old (Figure 1). Seventy five percent of male doctors and 94.4% of female doctors had worked for less than 10 years, and 46.4% of male doctors and 50% of female doctors had been working at display screen equipment for more than 4 years (Figure 2).
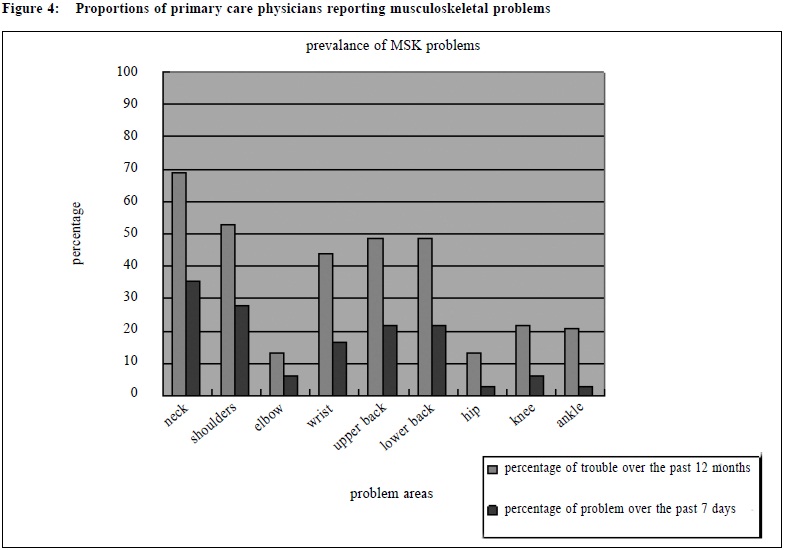
Regarding body mass index (BMI), there were 60.7% male doctors and 77.8% female doctors having BMI less than 23. All the doctors were non-smokers. There were 71.4% male and 66.7% female doctors wearing corrective lenses. 52.9% of them had their visual acuity check done more than 2 years ago. Work pattern characteristics The proportion of participants regularly performed stretching exercise was 22.1%. Only 13.9% of participants had macro breaks (break of several minutes or more). 30.9% of doctors reported that they had mini breaks (breaks of 1 to 2 minutes). 44.1% of doctors reported that they only had micro breaks (breaks of 10 to 15 seconds). The majority of male doctors (85.7%) and female doctors (77.8%) were having more than 2 evening clinic sessions per month. (Figure 3).
Prevalence of musculoskeletal symptoms By means of the standardized Nordic Questionnaire, the prevalence of neck, shoulder, elbow, wrist, upper and lower back, hip, knees and ankles symptoms were determined. With regard to the 12-month prevalence of symptoms, the highest values were reported in the neck (69.1%), shoulder (53.1%), upper back (48.5%), lower back (48.5%) and the wrist (44.1%). The least pronounced occurrences were seen in the elbow (13.2%), hip (13.2%), knee (22.1%) and ankle (20.6%).
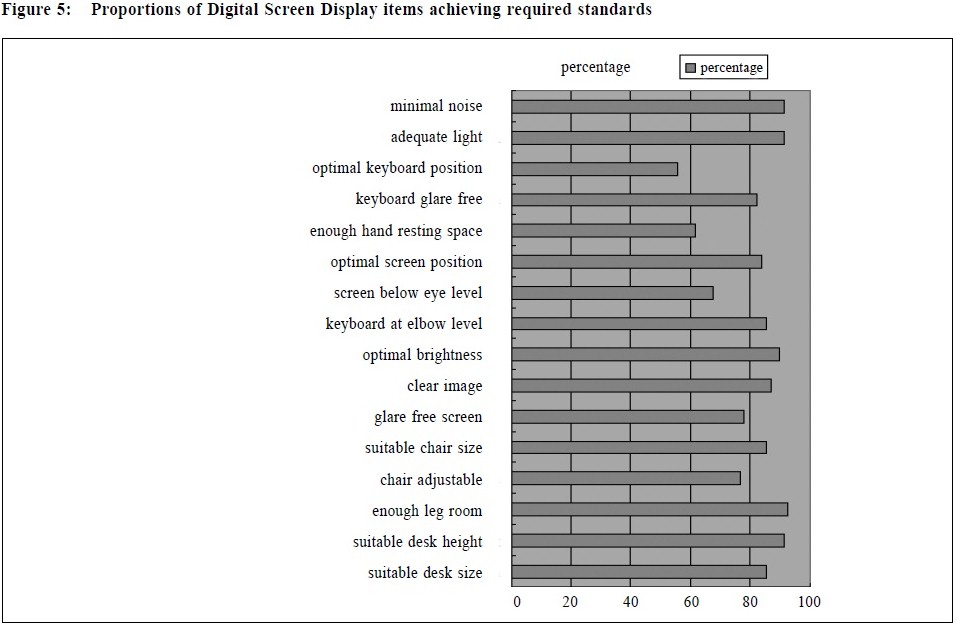
Workstation characteristic By means of the DSE checklist from the Labour Department, the prevalence of DSE arrangement reaching requirement was determined. There were 60% or above of items reaching the requirement of Labour Department of Hong Kong. The items where the highest proportions of physicians achieving standards included noise level (91.2%), light intensity (91.2%), desk height (91.2%) and leg room (92.6%). The lowest proportions achieving standards included keyboard position (55.9%), enough hand resting space (61.8%) and screen positioned below eye level (67.7%) (Figure 5).
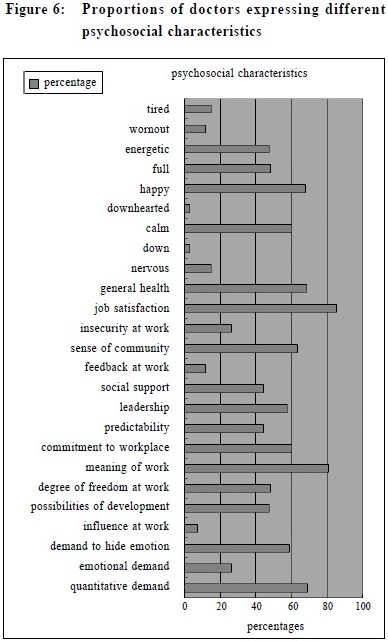
Eyes conditions Regarding eye symptoms, the most commonly reported problems were eyestrain (76.4%), heaviness (64.7%) and dryness (61.8%).There were 67.7% of staff wearing corrective lens. Psychosocial characteristic The short version of Copenhagen Psychosocial Questionnaire (CPQ) was used to determine the psychosocial working conditions, health and well being of doctors. The points of individual questions were added up according to standardized procedures to provide information on each scale.9 The highest percentage scales included were job satisfaction (85.3%), meaning of work (80.9%), quantitative demand (69.1%), general health (68.7%) and being happy (67.6%). The lowest percentage items included receiving feedback (11.8%), influence at work (7.4%), feeling down (2.9%) and downhearted (2.9%) (Figure 6).
Identification of symptoms predicting factors The potential predictive factors of each MSK symptom over 12 months were identified using binary logistic regression analysis with each symptom as a dichotomous variable. All factors with p<0.20 were included in a binary logistic regression model. Only job insecurity (OR= 8.592 , 95% CI 1.188-62.12, p=0.033) was positively associated with the presence of elbow symptoms over the past 12 months. The presence of “Quantitative demand” was associated with the occurrence of wrist symptoms in the past 12 months (OR=5.359, 95% CI, 1.082-26.55, p=0.040). Participants reporting “feeling tired” were more likely to present with knee symptoms (OR=63.71, 95% CI 1.293- 3139.1, p=0.037). All the other predictors did not show a statistically significant association. Discussion Aim and design of the study The aim of the study was to determine the prevalence of MSK problems in doctors working in the KWC Department of Family Medicine. In addition, the relationship between MSK problems and factors of the working conditions was studied. With the help of standardized questionnaires and checklist, the main features of DSE were described. Doctors were asked to fill in the questionnaire by themselves. The response rate was 53.5%. There were six questionnaires that missed out in the completion of Nordic questionnaire and they were not analyzed because the musculoskeletal problems were not determined. The low response rate could be related to the length of questionnaire which included the Nordic Questionnaire, short version of Copenhagen Psychosocial Questionnaire and DSE station assessment checklist. There were in total 213 items. We used standardized questionnaire in the assessment of musculoskeletal symptoms and psychosocial factors. However there was no physical examination part to determine the severity of the medical symptoms and this allowed record bias. DSE condition assessment The majority of DSE conditions met the checklist criteria. The checklist was filled in by DSE users and there was no measurement made on site. Some items were having more pronounced deficiency. These included keyboard position, hand resting space and screen position. These items could be related to adequacy of working surface area and the ergonomic design of work desk. There was a need on site assessment at individual clinics by trained assessors to measure the DSE dimensions and the usage of individual doctors in order to see if doctors used DSE in correct ways during work. Symptoms prevalence Bergqvist et al described that combinations of specific DSE work situations (e.g. typing work, work with DSE for more than 20 hours/ week) together with moderating factors were associated with an excess risk of suffering from muscular problems.10,11 Doctors at out patient clinics were characterized by long working hours with DSE and this study shows a high prevalence of MSK symptoms in doctors mainly over upper part of the body. As with the 12-month symptom prevalence, the 1 week prevalence results revealed that the neck and shoulder symptoms were more prevalent than the other parts of the body. With regard to the 12-month prevalence of the whole sample, the highest values were found in the neck (69.1%), shoulder (53.1%), upper back (48.5), lower back (48.5%) and the wrist (44.1%). The least pronounced occurrences were seen in the elbow (13.2%), hip (13.2%), knee (22.1%) and ankle (20.6%). These results are similar to the findings of other studies of workers with DSE.12,13 Predictors Based on the generated data, multivariable analyses were conducted for the occurrence of symptoms in the various parts of the body. A few factors were found to be correlated with the symptoms. Analyzing these factors with logistic regressions, there were only a few factors identified to be independent predictors of symptoms of elbow, wrist and knees. There is consensus that poor ergonomic conditions at DSE were the causes of MSK problems.16 In this study, the DSE conditions showed no significant impact on MSK symptoms. Silanpaa et al also showed similar findings in demonstrating no strong association between the duration of computer work and pain or between the duration of mouse use and pain.13 One of the reasons is that an audit was done in 2007 to standardize the DSE setting according to the Labour Department Guideline and all DSE settings met more than 90% of the standard. The high ergonomic standard and the small variance in the DSE setting contributed is the reason for no effect of DSE setting on MSK problems. The other reasons include the lack of on site measurement of DSE when being used during work and a small sample size. Psychosocial factors have been discussed as predictors in many previous studies.4,14,15 A number of psychosocial factors including insecurity at work, quantitative demand and feeling tired are independent predictors of elbow, wrist and knee problems respectively. These findings agree with many previous studies which showed high job demands, low decision latitude, time pressure, mental stress, lack of social support from colleagues and superior are suggested risk factors of MSK disorders in computer workers.16 Significance of the results The study is the first one to look into the demographic characteristics of the working doctor population in the cluster. It agrees with the main findings of literature that MSK problems were common in DSE users of long hours.4-6,10-12,15-22 Neck and shoulders symptoms occurred more often than symptoms of the distal part of the body. The study showed the prevalence of other related factors e.g. the prevalence of wearing corrective lens, and the psychosocial status of doctors. The study also identified independent work related predictors of MSK symptoms which included job insecurity, quantitative demand and feeling tired. This confirms with the study of Aries et al 4 who described psychosocial factors as independent risk factors for neck pain. Juul Kristensen et al demonstrated the speed of work was a prognostic factor for symptoms of low back.6 In this study, quantitative demand which was assessed by the questions of the need to work very fast, unevenly distributed workload and no time to complete work task, was associated with wrist symptoms. Although the MSK symptoms did not match completely among different studies, the association of psychosocial factors and MSK problems were repeatedly shown among studies. Although the doctor population is young, there is a high prevalence of musculoskeletal problems. This alerts us on the importance of starting health welfare programme early. Psychosocial predictors raised the issue of improving staff working morale through a better planning of work organization and management. For example, consider running stress management workshop for staff to decrease tiredness, organizing career prospect workshop to decrease the sense of job insecurity and the better managerial and organization change to decrease quantitative demand. Other outcomes like mental and sleep related disorders are demonstrated by Nakazawa et al to be increased among DSE users for more than 5 hours per day. This study did not assess mental disorder but feeling tired under the part of vitality assessment also demonstrated its association with knee symptoms. This sheds light into the need of screening for early mental disorders in DSE users. Limitations of the study Information about musculoskeletal symptoms, psychosocial factors and DSE conditions were selfreported. There was no standardized ergonomic assessment and physical examination to assess the level of over or underestimation of the factors. This also allowed recall bias. Although the instrument of Nordic Questionnaire and Copenhagen Psychosocial Questionnaire used are standardized questionnaire in the English version, their cross-culture validation are not checked when used in Hong Kong Chinese. The DSE set up questionnaires was adopted from the questionnaire of the Labour Department of Hong Kong on checking for occupational safety. This had not been assessed for reliability. When completed by different doctors, there is inter observer variation. This study cannot prove if the MSK problems of doctors are work related, we can only show association with some factors related to the working conditions. Non occupational factors e.g. household work, family conditions and personal medical data were not assessed. The cross sectional design of the study implies that only association between musculoskeletal symptoms and the predictor variables could be evaluated. Future longitudinal studies are warranted to assess cause-and-effect relationships. The response rate of the study was 53.5%. There is no further analysis on the demographic data and the reasons for not responding to the questionnaire. This can cause a selection bias in choosing out doctors with MSK problems because participants with more MSK symptoms may be more active in completion of the questionnaire and therefore will over-estimate the problems among all the doctors in the KWC. Reminder questionnaire to non-respondents can be given in the future and ways to encourage return of questionnaires can also be considered if resources allow. Preventive measures to be done The prevalence of MSK symptoms in this study was high especially when the majority of staff were young. Association between eye symptoms and MSK symptoms was found. With regard to more than 60% of doctors wearing corrective lens and only 50% of them had visual acuity check up done within 2 years, regular visual acuity checking can be arranged to help staff correct their visual problems. Although an audit was done two years ago based on the DSE checklist of the Labour Department of Hong Kong, there are also deficiencies shown in this study. DSE conditions need to be followed up in the future by trained assessors as well as by users. There is a need for better communication between users and assessors to check out details of the problems and adjustment will be made more flexibly and to fit better to individual situations. Feeling tired, quantitative demand and insecurity at work are associated with MSK problems. Organization workshop for doctors to help in stress management may help to alleviate these factors. Conclusion The prevalence of MSK problems is high among doctors working with DSE under the out patient clinic setting of HA. There may be a need for employer of HA KWC to provide further support to look into staff health issues more closely. When trying to improve working conditions, the association of psychosocial factors in MSK problems emphasizes the need of looking after psychosocial factors when planning future staff welfare programme. Although this study cannot clear the controversies reported by other studies on the extent of work related factors contributing to MSK problems of employees,5,6 it raises employers’ attention to staff health issue and sheds light into future studies when looking into the importance of psychosocial factors in improving staff health. Acknowledgement The study was funded by the Department of Family Medicine and Primary Care of Kowloon West Cluster of Hospital Authority. The authors thank Dr Sau Ngan Fu, Dr Martin Wong and Dr Kwok Leung Cheung on behalf of the research subcommittee of Kowloon West Cluster for their peer review and advices. All authors had full access to all of the data (including statistical reports and tables) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Data Sharing: technical appendix, statistical code and dataset are available from the corresponding author at drlam@graduate.hku.hk Key messages
Catherine TM Lam, MBBS, FHKCFP, FRACGP, FHKAM(Family Medicine) Chun-fat Lo, MBBS, DFM (CUHK), DOM (CUHK) Yuk-kwan Yiu, MBChB, FHKCFP, FRACGP, FHKAM(Family Medicine) Correspondence to: Dr Catherine TM Lam, Occupational Safety and Health Subcommittee, Department of Family Medicine and Primary Health Care, Kowloon West Cluster, Hospital Authority of Hong Kong, 1/FL GOPC Block, Our Lady of Maryknoll Hospital, Shatin Pass Road, Kowloon, Hong Kong SAR. References
|
|