|
September 2011, Volume 33, No. 3
|
Case Report
|
Two cases of Vitamin B12 deficiency – presenting as two different common manifestations in a primary care setting for the elderlyCarroll KL Chan 陳家樂, Linda YF Hui 許燕芬, Wai-man Chan 陳慧敏 HK Pract 2011;33:115-120 Summary Elders are prone to multiple medical diseases, of which atypical presentations are not uncommon. Some common presenting symptoms might also be due to relatively uncommon but significant diseases in the primary care setting especially in elderly practice. In this article, we use two cases of Vitamin B12 deficiency with different clinical manifestations to illustrate this point in the care of elderly patients. By means of careful clinical assessment by primary care doctors and appropriate simple laboratory tests to make early diagnosis and hence prompt treatment, we can prevent serious irreversible complications and improve the quality of life of our elderly patients in the community. 摘要 長者容易患上多種疾病,其中非典型病徵並不罕見。某些常見的症狀可能是由一些基層醫療中比較少見但重要的疾病引致。本文我們報道兩個有臨床表現不同的維生素B12缺乏的案例,以說明這上述觀點。家庭醫生通過仔細臨床評估,進行適當簡單的實驗室測試,可以早期診斷和及時治療,進而避免嚴重而不可逆轉的併發症,並且提高社區年老患者的生活質素。 Introduction Elderly Health Centres (EHCs) of the Department of Health's Elderly Health Service provide comprehensive health assessments for our Hong Kong residents aged above 65 years in our community. EHCs also provide curative care for elders in accordance with Family Medicine practice. It is very common for our elderly patients to complain of multiple symptoms, some of which might sound trivial or too common so as to be taken for granted. However, as older people are susceptible to multiple medical illnesses and atypical presentations of diseases, even trivial presenting symptoms or bread-and-butter cases in the elderly may indicate significant medical diseases. Professor Richard J. Ham, Professor in Family Medicine and Professor in Medicine, has remarked that the changes which usually occur with increasing age, together with the way our society treats the old, combine to modify the ways in which illnesses present. Certain characteristics unique to the elderly and requiring special consideration are frequently overlooked.1 So it is advisable for us to pay special attention to consider a wider range of possible differential diagnoses before drawing a conclusive diagnosis for our elderly patients. In this article, we would like to share two cases of Vitamin B12 deficiency seen in two Elderly Health Centres to illustrate this point. Case 1 Madam Lee, a 76 years old widow, living with her daughter and grandson, had known history of hypertension which was well controlled with perindopril 8mg daily and prasozin 0.5mg BD. She also suffered from lumbar spondylosis, which was followed up by the orthopaedic unit in a public hospital, and discharged since April 2009. After her discharge by her orthopaedic doctors, she had episodic complaints of low back pain associated with lower limb numbness, which was relieved by Dologesic and Vitamin B6 prescribed by different primary care doctors. Otherwise, her past health was good. Her symptoms were stable until August 2010 when she attended our Shau Kei Wan Elderly Health Centre. She complained that the numbness in her lower limbs was slowly getting worse in the recent few months, involving both feet and more severe on the left side, ascending from the tip of her toes to the level of her ankle, and her complaints were not responding to treatments given by various doctors. The numbness appeared different from before, and was persistent day and night, even when her low back pain was not so bad. There was neither burning sensation nor pain over the feet. She had no claudication symptom or muscle cramp. Except for feeling a bit clumsy when she walked, she did not experience any limb weakness. There was also no upper limb symptom or sphincter disturbance. She did not have symptoms of diabetes and her latest fasting blood sugar level was 5.4mmol/L. Physical examination revealed decreased sensation over her left foot at the L5 dermatome compared with the right foot. The power of all her four limbs was full. The provisional diagnosis at that moment was "lumbar spondylosis with associated neuropathy". Referral for a trial of physiotherapy was suggested but she declined because physiotherapy had not been effective for her symptoms in the past. In view of the change in the characteristics of her numbness as well as the insidious and progressive nature of the disease course, blood investigation was ordered to rule out metabolic causes of her neuropathy.
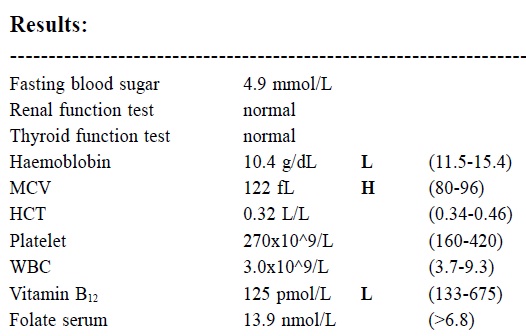
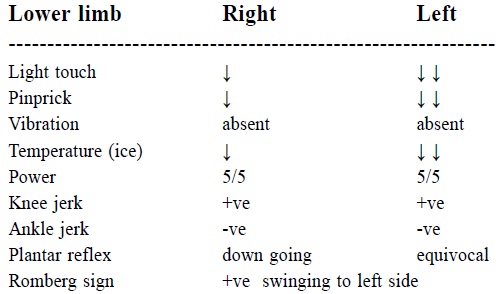
Taking the abnormal laboratory results into consideration, the provisional diagnosis had to be reviewed. On further physical examination, we found:
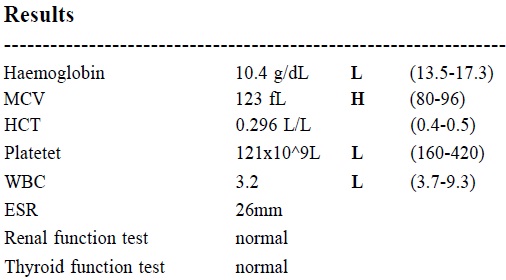
Further enquiry revealed that her recent clumsiness on walking caused her to nearly fall on several occasions and she had a fall just one week before. Fortunately she did not sustain any major injury from this recent fall. That was why she had started to use a walking stick lately. In view of the macrocytosis, low Vitamin B12 level and the presence of neurological signs like positive Romberg, the patient was clinically suspected to be suffering from subacute combined degeneration of the spinal cord and megaloblastic anaemia due to Vitamin B12 deficiency. It was noted that the patient was not a vegetarian and her diet pattern was normal. After six loading doses of Vitamin B12 intramuscular injections, her symptoms improved dramatically with almost complete resolution of her feet numbness. She also described that she walked much more steadily than before. Physical examination revealed sensation and Romberg test had returned normal. With her excellent treatment response, the clinical diagnosis of subacute combined degeneration of the spinal cord due to Vitamin B12 deficiency was confirmed. The Vitamin B12 level returned to normal at 324 pmol/L two months later, and the Vitamin B12 at a dosage of 1mg by IMI injections would continue every 3 months. Case 2 Mr Lau, a 75 year-old retired manual worker, lived with his wife and daughter in a public housing estate flat. In January 2010, he attended the Lam Tin Elderly Health Centre for a health assessment and complained that he had lost his mood and interest for about half a year. His sleep was fragmented with intermittent waking up. He lost interest to go out and preferred to stay at home most of the time. His taste for food turned strange and unpleasant which affected his appetite and eating, causing him to lose weight. Another reason for his weight loss was because of his poor denture. However, he had delayed seeing a dentist because of cost concern. Financially, he and his wife had to rely on his savings and the support from daughter since retirement. Despite the financial constraint, he denied any other recent significant stressful family event. He did not harbour any self-harm or suicidal idea. He enjoyed good relationship with his family members all along. His score in the 15-items Chinese version of Geriatric Depression Scale (GDS) was 12 out of 15 (with cut-off at 8).2 Taking into account the typical clinical features of depression and the GDS score, the clinical diagnosis of depression was made at that time. However, he had worries about possible side effects of medication, so he opted for psychotherapy by our clinical psychologist (CP ) . Additionally he looked pale and blood investigation for complete blood count was ordered. When Mr. Lau was first seen by our CP, he was observed to have low mood and low self-esteem but no suicidal idea. His sleep was poor with intermittent waking up. On the whole, he was able to maintain normal functioning. Our CP diagnosed him as suffering from depression and possibly in reaction to social stresses of financial constraint. Sleep hygiene was discussed with Mr. Lau by our CP at that session. After getting his agreement, our CP planned to have cognitive therapy for him and to review the client with his daughter at a next session. The results of blood investigation was as follow:
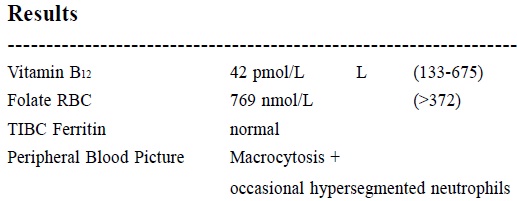
In view of the finding of macrocytic anaemia and the relative pancytopenia from the blood tests, further investigations were arranged and the result was as below:
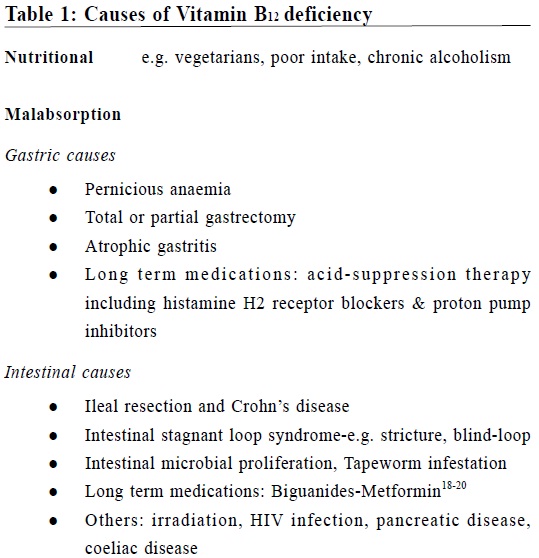
Serum B12 was low while his folate level was normal. The patient was not a vegetarian and his diet pattern was normal. Mr. Lau was diagnosed as suffering from depression and Vitamin B12 deficiency and loading doses of Vitamin B12 injections were given to patient. When the patient was reviewed with his daughter by our CP at the follow-up session, just around one month after Vitamin B12 injection, he was found to have much improvement of his mood even though cognitive therapy had not begun and his social problem of financial constraint had not yet settled. Besides regaining interest to go out, the somatic symptoms related to his "depression" including strange taste, loss of appetite, lethargy, and the poor sleep were all subsided. Since neither the CP nor the attending doctor had started any psychotherapy and his social stressors yet to be solved and the only active intervention during this period was Vitamin B12 injections, the doctor concluded the clinical response was due to Vitamin B12 replacement. Diagnosis of depression secondary to Vitamin B12 deficiency was made. Discussion In this article, we report two cases of Vitamin B12 deficiency in two elderly patients with different clinical manifestations. Since the two cases were from selected populations, our report cannot be generalized to all cases. However, because of the potential reversibility of Vitamin B12 deficiency, it is worthwhile to have a general discussion on the topic. The prevalence of Vitamin B12 (also known as cobalamin) deficiency in the general population is unknown but the incidence is noticed to increase with age. In overseas studies, although different figures were found depending on defining criteria, a more common prevalence figure was in the range of 12% to 15% of the elderly over 65 years of age, were found to have laboratory evidence of Vitamin B12 deficiency.3-5 Local data is still lacking for the time being. Hence our Elderly Health Service is now conducting a study on the prevalence of Vitamin B12 deficiency among the members of our Elderly Health Centres. Vitamin B12 is found in meat, eggs and milk, fish, but not in plants. The absorption of Vitamin B12 from food is a complicated process. In the acid environment of the stomach, pepsin releases cobalamin from animal protein, and cobalamin then binds itself to a salivary protein called haptocorrin. In the alkaline environment of the small intestine, haptocorrin is broken down by pancreatic enzymes to release the cobalamin which then binds itself with a intrinsic factor secreted by gastric parietal cells. This new complex then binds itself to receptors at the terminal ileum and is here actively absorbed. A small proportion (1%) of Vitamin B12 intake is absorbed by passive diffusion. The recommended daily allowance of Vitamin B12 is small (2μg per day) compared with body stores (2-5mg).6 Vitamin B12 plays an important role in DNA synthesis and neurologic functions. Recently, studies are being conducted to explore the role of Vitamin B12 deficiency in hyperhomocysteinaemia, atherosclerosis and increased cardiovascular risk.7-8 Vitamin B12 deficiency may take many years to develop, and patients may be asymptomatic or may present with a wide variety of neurological, psychiatric and haematological manifestations,9-10 which can often be reversed by early diagnosis and prompt treatment. Onset of neurological symptoms is usually subacute or gradual. Neurological symptoms of Vitamin B12 deficiency include numbness or paresthesias and peripheral neuropathy.11 Numbness usually starts at the tips of toes and then in the fingertips. Paresthesias are ascending in its course. Simultaneous involvement of the arms and legs are uncommon and onset in the arm is rare. In the early course of the disease, loss of vibration sense predominates. As the disease progresses, ascending loss of pinprick, light touch, and temperature sensation occur. Since Vitamin B12 is intergral to the myelination process, its lack or deficiency results in abnormal myelin formation or even frank demyelination, typically involving the dorsal columns of the spinal cord, at times the lateral spinothalamic tracts, i.e. subacute combined degeneration of spinal cord.12 So in our first case, the impaired sensation and the positive Romberg sign probably accounted for the pathological involvement of peripheral nerve and spinal cord. However, one typical sign of subacute combined degeneration of cord, i.e. hyperreflexia of knee jerk was not elicited in the first case, probably because the patient was not able to relax completely. In general, half of patients may have absent ankle reflexes with relative hyperreflexia at the knees. Plantar reflexes are initially down-going and later up-going. Gait may be wide-based. Vitamin B12 may involve the central nervous resulting in psychiatric disorders such as memory loss, irritability, depression as demonstrated in Case 2, dementia and rarely psychosis, and the olfactory nerve resulting in anosmia. Very rarely (0.5%) the optic nerve may also be involved. Constitutinal symptoms including anorexia, fatigue and malaise may occur in about half of patients. Other features including oropharyngeal ulceration, glossitis with sore tongue, impairement of taste (as seen in our Case 2) are not uncommon.6,10 Autonomic features like impotence, bladder or bowel incontinence are rare. Macrocytic anaemia, which may be severe, mild or absent occurs in the later stages of the deficiency. Typical Vitamin B12 is characterized by MCV>95fl and sometimes 120-140fl in severe cases. On blood film, hypersegmented polymorphonuclear leukocytes are found.6,10 In the advanced stage, leucopenia and thrombocytopaenia may also be present.9,10 It should be noted that early treatment with Vitamin B12 in subacute combined degeneration stops disease progression and improves neurological deficit in many patients.13-14 However, if neurological damage by Vitamin B12 deficiency is left untreated, further pathological damage on the cortical spinal tract may lead to irreversible complications including limb weakness, ataxia and spasticity. Causes of Vitamin B12 deficiency include insufficient nutritional intake and malabsorption, which can be summarized in Table 1. In the elderly population, the possible cause tends to be multifactorial, 15-17 e.g. food preference and poor denture often lead to decreased intake of meat while atrophic gastritis and long-term medications such as acid suppression therapy etc are also common in the elderly. Such causes can be identified by careful history taking. The traditional Schilling test for detection of pernicious anemia has been replaced by serologic tests for parietal cell and intrinsic factor antibodies. The value of testing in the elderly patients with clear Vitamin B12 deficiency is debated as treatment is the same regardless of the underlying cause.6
Interpretation of Vitamin B12 level may sometimes be misleading as concentration of Vitamin B12 may vary a lot between different individuals. This is compounded by the lack of consensus among different commercial assays. In patients with neurological or haematological abnormality and low or borderline-low Vitamin B12, a therapeutic trial of Vitamin B12 treatment should be given, followed by monitoring full blood count and clinical response.6 If the Vitamin B12 level is normal but the clinical suspicion is high, family doctors may consider to refer the patient to specialist clinic for consideration of a more sensitive method of screening by measurement of serum methylmalonic acid and homocysteine, which are increased early in vitamin B12 deficiency.9,21 Conclusion We report two cases of vitamin B12 deficiency in two elderly patients with different clinical manifestations. In our first case, an elderly lady presented with a common symptom of numbness, caused by subacute combined degeneration of cord, which if left untreated, would develop irreversible devastating complications including ataxia and spastic paraplegia. In our second case, the diagnosis of depression in an elderly gentleman was subsequently found to be secondary to a metabolic cause. Because of the potential reversibility of this condition, it is worthwhile to consider Vitamin B12 deficiency as a differential diagnosis for neuro-psychiatric symptoms in elderly and in the high risk groups. Acknowledgement We would like to thank Dr Mok Kin Fai, medical officer in charge of Lam Tin Elderly Health Centre, for providing the clinical information of the second case.
Carroll K L Chan, MBBS (HK), FRACGP, PDip Community Geriatrics (HK), FHKAM
(Fam Med)
Ag Senior Medical Officer Elderly Health Service, Department of Health. Linda Y F Hui, MBBS (HK), FHKCFP, FRACGP, FHKAM (Fam Med) Consultant (Family Medicine) Elderly Health Service, Department of Health. Wai-Man Chan, MBBS (HK), MPH (USA), FHKAM (Com Med) Assistant Director of Health Family and Elderly Health Services, Department of Health. Correspondence to : Dr Carroll Ka-lok Chan, Shau Kei Wan Elderly Health Centre, 8 Chai Wan Road, Shau Kei Wan, Hong Kong SAR.
References
|
|