|
September 2011, Volume 33, No. 3
|
Original Articles
|
Family Medicine training in Hong Kong's public health care system : A focus group studyKenny Kung 龔敬樂 Samuel YS Wong 黃仰山, Carmen Wong 黃嘉雯, Martin CS Wong 黃至生, Ting Gao 高汀, Sian Griffiths 葛菲雪 HK Pract 2011;33:97-106 Summary
Objective: General Outpatient Clinics (GOPCs) now provide the main
bulk of basic community training for Family Medicine (FM) trainees. Although it
is obvious that there is a rising number of FM trained doctors, there still remains
a significant proportion of the GOPC workforce who have not been through any formal
vocational training. With the increasing role of FM in Hong Kong's healthcare, the
Chinese University of Hong Kong (CUHK) and the Hospital Authority conducted a joint
project to review and define the role of GOPCs and FM training that can facilitate
primary care development for the whole of Hong Kong and provide a robust community
based medical service affordable to all. Thus, focus groups were formed to study
and form part of the whole project which looked at FM training provision within
the GOPC setting.
Keywords: Family Medicine training, General Outpatient Clinics 摘要
目的: 普通科門診是提供家庭醫生訓練主要的地方。雖然家庭醫生練習生的比例愈來愈高,仍有相當一部份在普通科門診工作的醫生未接受任何正式家庭醫學的訓練。鑒於家庭醫生在香港的醫療體系的角色日趨重要,香港中文大學和醫院管理局進行了一個聯合計劃,以界定普通科門診和家庭醫生訓練的作用,藉此促進香港整體基層醫療的發展,供給一個全民負擔可負擔的以社區為本的健全醫療服務。焦點小組是此計劃的一部份,主要是去考察在普通科中家庭醫學訓練的運作。
主要詞彙: 家庭醫學訓練,普通科門診。 Introduction The government's latest healthcare reform document clearly emphasized the need to enhance primary care in Hong Kong.1 As a matter of fact, since 2000 there had been a rapid increase in the number of Family Medicine (FM) trainees intake per year, from around 10 in the 1990s to over 90 in 2004.2 While higher training can take place in any community setting that allows the trainee to practise Family Medicine, basic training must take place in a recognized vocational training centre. Since their transfer from the Department of Health to the Hospital Authority (HA) in 2003, General Outpatient Clinics (GOPCs) now provide the main bulk of basic community training for FM trainees. GOPCs serve as the venue for clinical practice and provide facilities for training. Many FM specialists are employed in the GOPCs and serve as trainers for trainees working in these GOPCs. Although it is obvious that there is a rising number of FM trained doctors, there still remains a significant proportion of the GOPC workforce who is without any formal vocational FM training. There is an obvious need to address this area in view of the government's directive regarding primary care. With the increasing role of FM in Hong Kong's healthcare, the Chinese University of Hong Kong (CUHK) and the HA conducted a joint project to review and define the role of GOPCs and FM training that can facilitate primary care development for the whole of Hong Kong and provide a robust community based medical service affordable for all. This paper forms part of a project which looks at FM training provision within the GOPC setting. There have been very few studies that looked into local FM training. One previous study showed that the learning needs of primary care doctors closely related to their perceived needs in their daily works.3 Another study reported that FM trainers were unsure on what and how to teach. More varied training methods, more resources at training centres and more coordination among training stakeholders should be made available.4 Focus groups were therefore conducted to review the current training methods and arrangements in GOPCs. The objective is to seek views towards FM training in a GOPC setting from both trainees and trainers as well as from servicing doctors with the intention of providing authorities in identifying gaps and means of improving future training in the GOPCs. Method Focus groups were conducted separately for each of the following groups of doctors:
1. Basic trainees (BT), defined as community trainees (FM) receiving basic training
from the Hong Kong College of Family Physicians' (HKCFP) vocational training programme
and working in the general outpatient clinics (GOPCs). Doctors were selected through randomization and were then invited to take part. At least one doctor from each of the seven clusters of the Hospital Authority was expected. The target was to have at least six doctors from each focus group in order to make the sampling representative although over sampling of 30% was conducted to compensate for "no shows". No financial incentive was given for participants. Written consent from each participant was obtained before the focus groups were conducted. Proceedings were recorded with an MP3 recorder and transcribed "in verbatim". One author from among us and one research assistant with experience in qualitative analysis served as facilitators of the discussions. The focus group discussions were semi-structured, with the following areas covered (minor variations were allowed depending on the subgroup of participants):
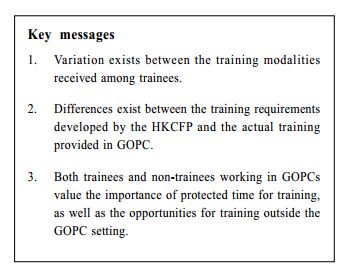
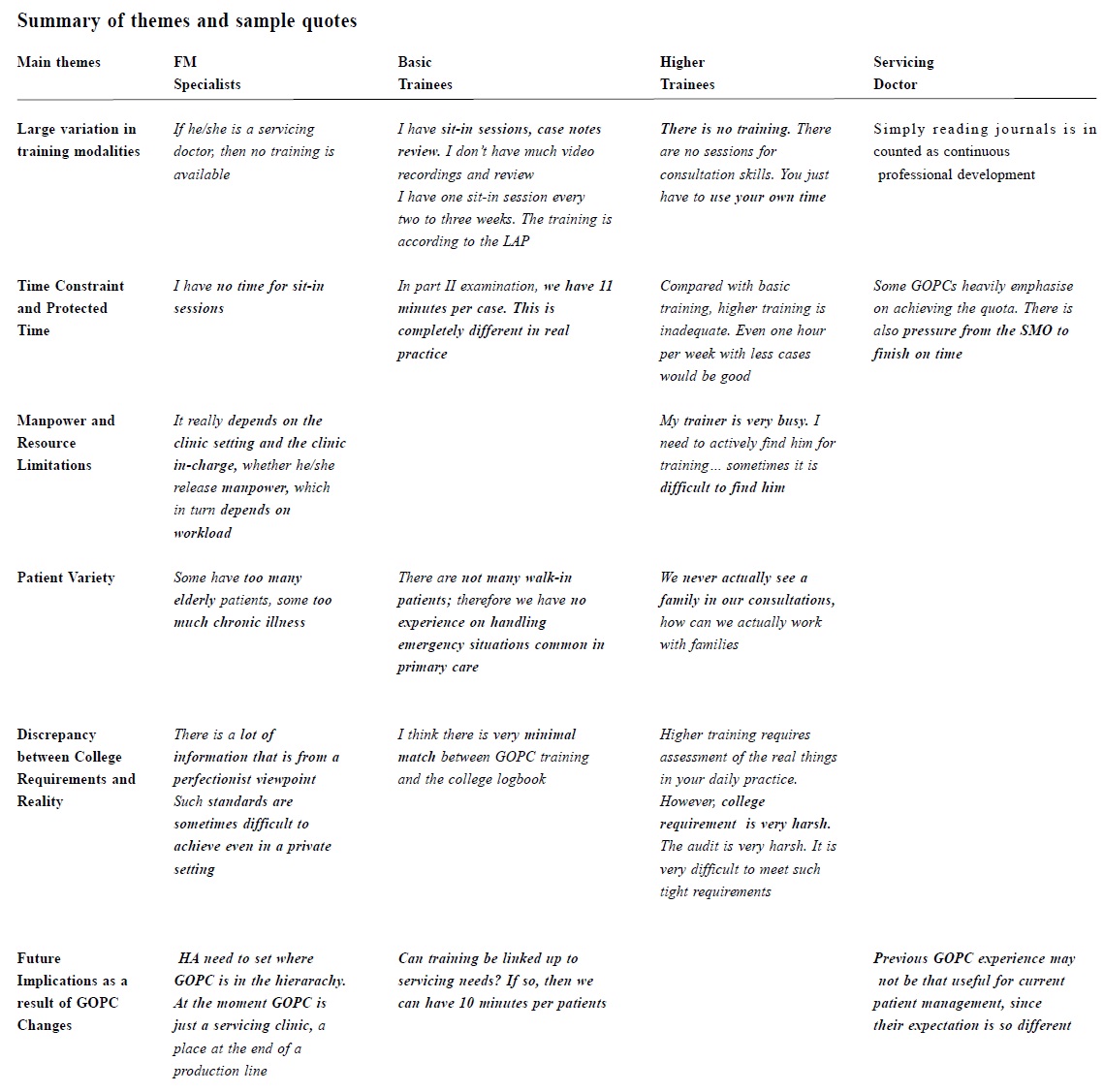
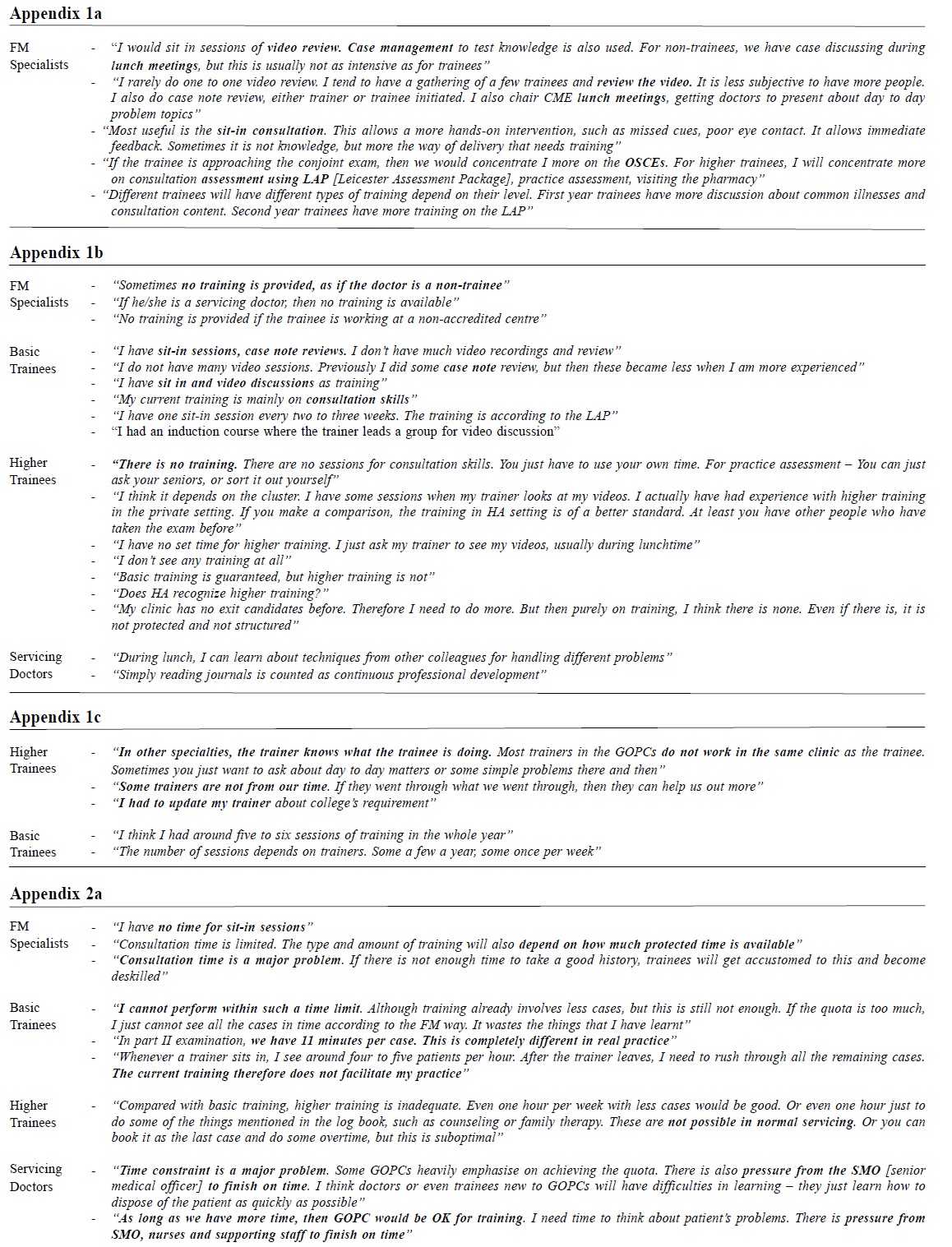
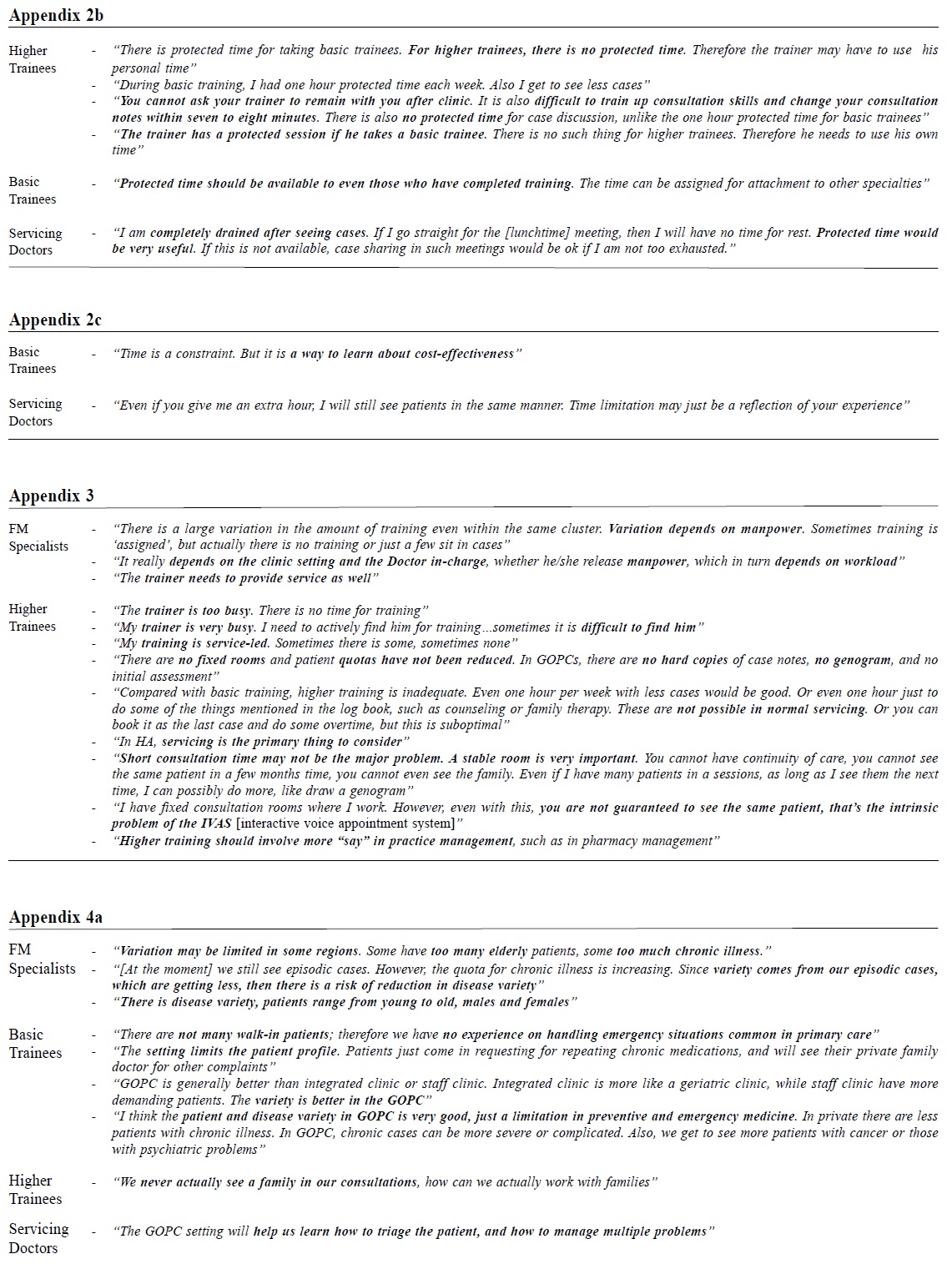
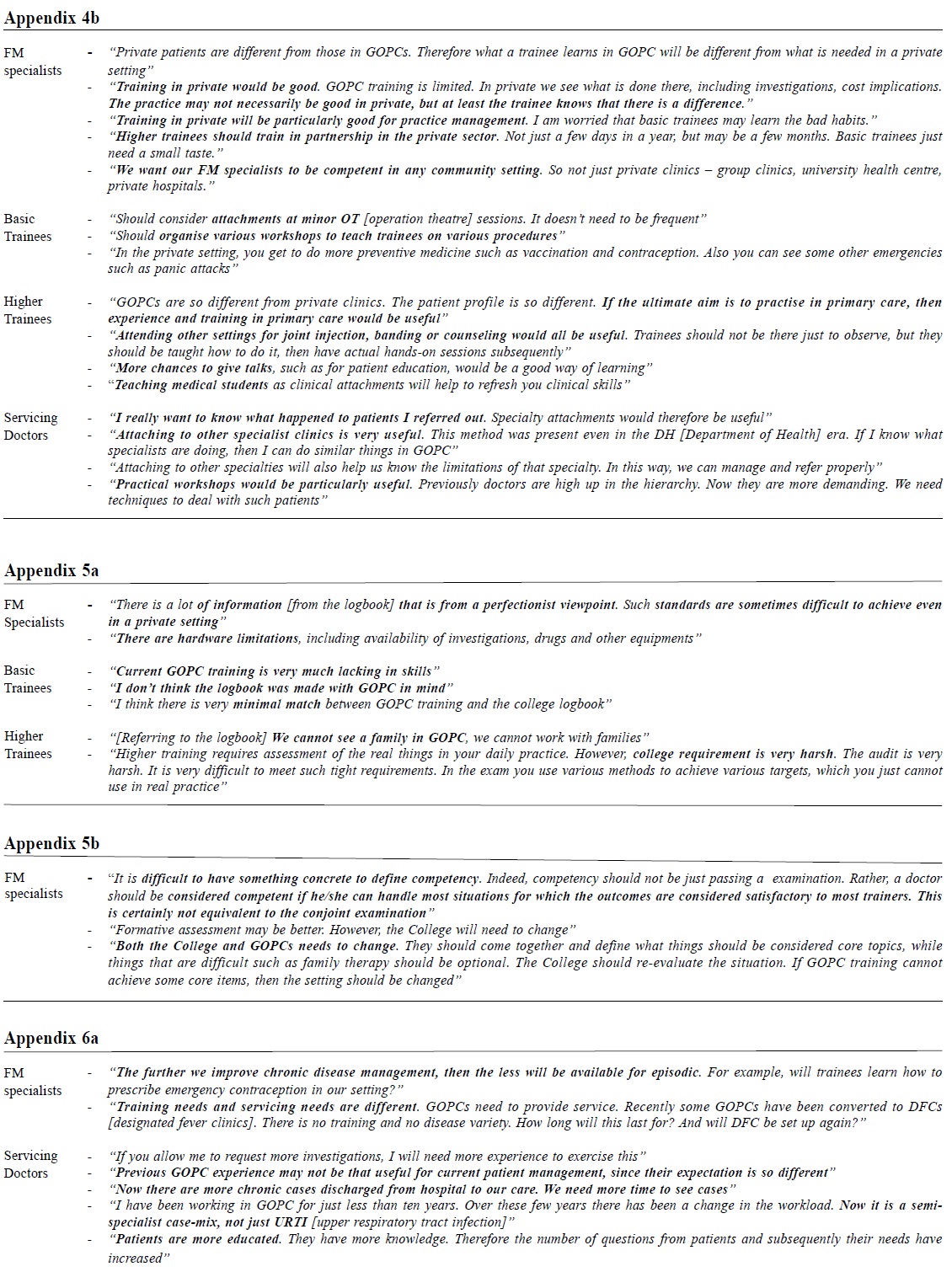
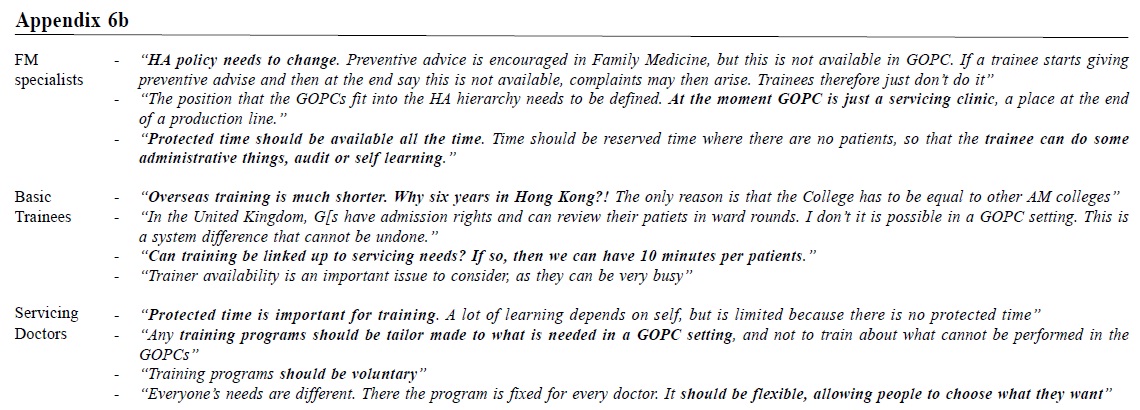
l current training modalities The transcripts were analyzed for recurring themes with the aid of NVivo 8 software. A group analytical approach was conducted to enhance the reliability of the analysis. The transcripts were read by one investigator and possible broad themes identified. Emergent themes that occurred repeatedly within the group would be noted as recurrent themes. Similarly, another investigator would read all the transcripts and generate emergent and recurrent themes independently. Subsequently, emergent themes were agreed upon. Groups of related recurrent themes was organized under a master theme. Results The 4 focus groups met in November 2009. Six basic trainees, 11 higher trainees, 5 Family Medicine specialists and 12 servicing doctors made up the 4 groups, respectively. Recurrent themes noted are as follow: 1. Large variation in training modalities All the trainers used different modalities for training their doctors. These included sit-in consultation sessions, video recording and discussion, case discussion, practice management assessment and hot topic discussion on an individual and group basis. Some trainers also gave training on procedural skills. (Appendix 1a) Everybody was aware of the training modalities provided at the local cluster-wide level. However, nobody was able to provide information regarding the type of training in overseas settings. Basic trainees, higher trainees and servicing doctors had different experience of their training, both in an intra-group and inter-group settings. The amount of training provided for servicing doctors was often viewed to be minimal; indeed some HA trainers were not providing training if the doctor was not a trainee. Servicing doctors' way of getting training involved learning from peers, lunch time meetings and learning from journal reviews and seminar updates. For basic trainees, there appeared to be a large variation in the amount of training provided; some had only a few formal sessions per year, while some had regular weekly sessions. If the trainee was working in a nonaccredited centre, then training may not be available. There was no formal training for higher trainees. Training may sometime be led by the trainee him/ herself. (Appendix 1b) There were differences even at the trainers level. Trainers had their own work to do. Some of them were sometimes not readily available, and may not be working at the same clinic as the trainee. In addition, some trainers may not be up-to-date with the latest College requirement. (Appendix 1c) 2. Time constraint and protected time Eight out of 12 servicing doctors, 7 out of 11 higher trainees, 5 out 6 basic trainees, and 4 out of 5 trainers raised the issue of time constraint. Participants used words such as "squeeze" and "rush" to describe their experience. Both trainers and trainees agreed that short consultation periods limited the quality of training. The need for protected time was repeatedly mentioned. (Appendix 2a) For all non-trainers and servicing doctors, setting aside time specifically for training appeared to be important. (Appendix 2b) Two servicing doctors saw the advantages of the GOPC time limit, where time management and cost effectiveness can be learnt. Indeed, they felt that giving them extra time will not actually be that useful. (Appendix 2c) 3. Manpower and resource limitations Manpower was a frequently mentioned limitation for training. Doctors mentioned that because GOPCs were expected to provide a minimum service throughout, doctors often found that they needed to maintain a high patient load, thereby compromising their training opportunities. In addition, trainers were part of the servicing team and may also be involved in other administrative duties. Higher training involved many practice-based issues which were often not within the higher trainees' control, and may affect training. These barriers included electronic consultation notes, lack of genograms, record-based continuity and the telephone booking system. (Appendix 3) 4. Changing patient variety GOPC had a well defined set of patients and related disease variety. Some viewed this as part of limitations in providing FM training, while others were positive towards this, especially when compared to training in the integrated clinic-setting. Nevertheless, many agreed that exposure to what went on in private practices was important. (Appendix 4a) All agreed that there were limitations to what training could provide in GOPCs. In addition, most trainers in GOPCs were GOPC-trained, and had limited knowledge on what was needed in private and other settings. In this respect, alternative training locations including private clinics and specialist attachments were considered useful for training purposes. (Appendix 4b) 5. Discrepancy between College requirements and reality The requirements set by the College were comprehensive, and appeared from a perfectionist's view point of what should be attained. Many of the indices provided could only be achieved in principle, but the process may not be achievable both in a GOPC or real setting. (Appendix 5a) Some trainers considered a trainee to be competent in Family Medicine if they passed the conjoint fellowship examination. This level of achievement has been recognized internationally, and is equivalent to the MRCGP and FRACGP examinations. The FM exit examination that defines specialist status is a legal requirement unique to Hong Kong, but there are questions as to whether competency should be considered only after AM fellowship is obtained, or whether the exit examination requirements should be added to the conjoint examination. In addition, some felt that one single examination alone may not be adequate to define competency. Ultimately, if training in GOPC is to be considered competent for Family Medicine training, then both College requirements and the process by which training is being offered in GOPCs must change. (Appendix 5b) 6. Future Implications as a result of GOPC Changes As mentioned above, the disease mix of patients have been quite stable, something that is intrinsic to the GOPC system. However, there is a risk that this small variation will disappear in a few years, which may eventually affect training requirements. (Appendix 6a) In order to be in line with Family Medicine principles, various barriers must be overcome in the future. Such barriers include consultation issues, HA policy, and administrative needs. But whatever changes in training are to be implemented, individualized training programmes may be more effective for some doctors. (Appendix 6b) Discussion Summarising focus groups findings The advantages of GOPC in providing FM training include the wealth of patients with chronic illness, a reasonable spectrum of patients attending for episodic illnesses and also the large pool of chronic patients encountered. Nevertheless, the inherent servicing needs of GOPCs appear to be the major limiting factor in training provision. Such servicing needs result in short consultation time, high patient load and lack of patient continuity. Department may not be able to release sufficient manpower for training, let alone allow room for protected training time. In addition, even trainers may not be available to provide training. All participants saw the need for training that conformed to their work in the GOPC, as well as providing alternative training outside GOPC setting. There is as yet no consensus with regard to the core FM competencies within our local context and the best way to measure competency.
Implication for HKCFP Some trainees, whether basic or higher, made a link between FM training and the conjoint or exit examination. Examinations are important milestones which trainees view they must achieve in order to proceed higher in their career, since passing examinations are equivalent to owning quotable qualifications as well as financial increments. In order to provide trainees with a consistent view of FM qualities and competencies, collaborations between the HKCFP and HA would be essential so that training provision and requirements are in line with each other. Implications for GOPC and HA Since HA is currently the major provider for FM training in Hong Kong, it is essential that FM training in the GOPC can catch for future enhancement in primary care provision in our region. Issues surrounding consultation quality can be addressed through reviewing time allowed for and the quality involved with training. There may be a need to review the appointment booking system so that continuity can be extended beyond the informational level. Opportunities for non-GOPC training can also be explored, including collaboration with hospital specialists and private doctors. It is interesting to note that most specialties do not have protected time for training. However, hospital specialty training facilitates supervision by senior colleagues simply because of the nature of their duties (such as ward rounds and surgical operations). This is different in FM training, where the large majority of clinical duty is under independent/solo practice. Knowing that many doctors voice out the need for protected training time and that current GOPC manpower calculations are service orientated, future changes may need to consider incorporating protected time for training as a manpower planning parameter. Importance of an independent regulatory body Communication between the different levels is essential to allow effective changes to occur. It may be necessary to form a working group that incorporates these different parties so that the different ideas can be intertwined. This suggested form of multilevel communication and coordination is similar to the UK's Postgraduate Medical Education and Training Board (PMETB), which is an independent body set up in 2003 that oversees postgraduate training and specialist certification. The Hong Kong Academy of Medicine has a similar certification function, yet lacks the communicator role. Limitations This focus group study only obtained the views of less than 10% of the entire GOPC doctor workforce. Selection bias may be present, since those without any negative feelings towards GOPC or training may have declined study participation. Development of a questionnaire structured with findings from this qualitative study will help in assessing opinions from all GOPC doctors. Conclusion The government's plan to improve primary care mandates high quality family medicine training in the GOPC setting. The government, HA and HKCFP will need to collaborate closely in the coming years so that our future frontline doctors can be nurtured in an environment that promotes Family Medicine. Only through this can Family Medicine blossom and only through this will the Hong Kong population receive the most appropriate primary care.
Kenny Kung, MFM (Monash), FHKAM (Fam Med), FHKCFP, MRCGP (UK)
Assistant Professor (Clinical) Samuel Y S Wong, MD (CUHK), MD (Toronto), MPH (Johns Hopkins) Professor (Clinical) Carmen Wong, MBBCh (UK), DRCOG (London), DFFP (London), MRCGP (UK) Assistant Professor (Clinical) Martin C S Wong, MD, MSc, MPH, FHKAM (Fam Med) Associate Professor (Clinical) Ting Gao, MSc (Liverpool), BSc Research Assistant Division of Family Medicine and Primary Healthcare, School of Public Health and Primary Care, The Chinese University of Hong Kong. Sian Griffiths, FHKAM (Com Med), FRCP, FFPH, FHKCCM Director School of Public Health and Primary Healthcare, The Chinese University of Hong Kong. Correspondence to : Dr Kenny Kung, Family Medicine Training Centre, 3/F LKSSC, Prince of Wales Hospital, Shatin, New Territories, Hong Kong SAR.
References
|
|