December 2012, Volume 34, No. 4 |
Original Articles
|
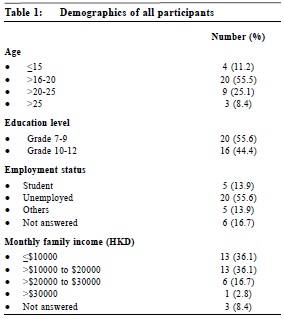
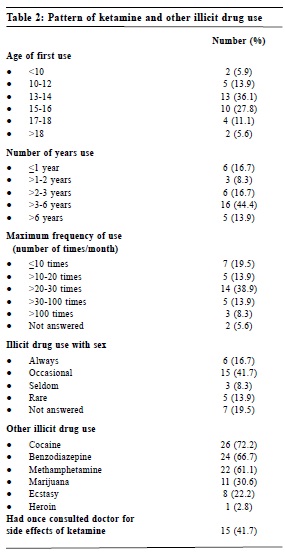
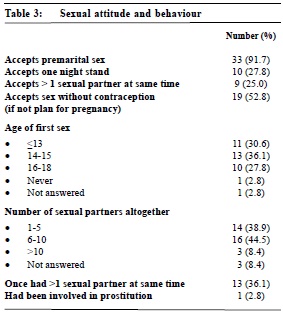
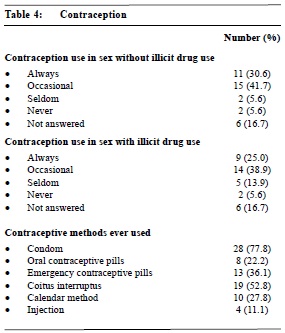
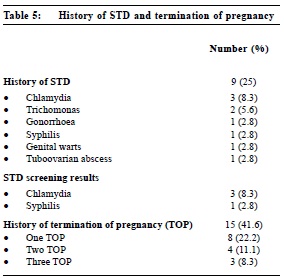
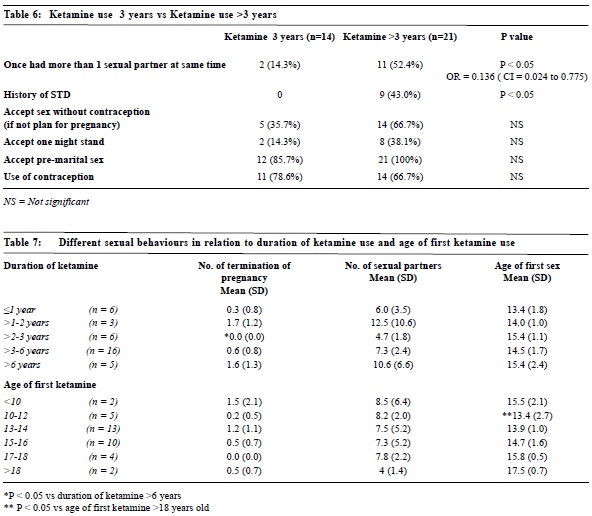
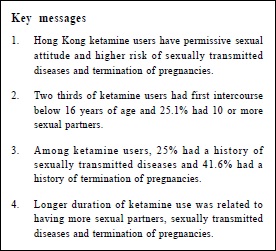
A pilot study on sexually transmitted diseases and high risk sexual behaviour in Hong Kong female ketamine usersJacqueline HS Lee 李灝思, Rachel YK Cheung 張優嘉, Symphorosa SC Chan 陳丞智, Albe WL Pang 彭煒琳, Tony KH Chung 鍾國衡 HK Pract 2012;34:132-144 Summary Objective: To explore sexual attitude, high risk sexual behaviour and prevalence of sexually transmitted diseases (STD) in Hong Kong female ketamine users. Keywords: Illicit drug use , ketamine , sexually transmitted diseases, sexual attitude, high risk sexual behaviour 摘要 目的:研究香港濫用氯胺酮少女的性觀念,高危性行為及感染性病之普遍性。 設計:橫切面式調查。由2009年11月至2010年2月,在威爾斯親王醫院婦科門診部招募來自某戒毒所的少女進行研究。她們填寫一份關於性觀念及高危性行為的問卷,並接受婦產科病史面談及性病篩選檢查。 研究對象:濫用氯胺酮的少女。 主要測量內容:性觀念,高危性行為及感染性病之普遍性。 結果:共36位濫用氯胺酮少女參與是項研究。其中三分二在16歲或以下己開始發生性行為。25.1%有10個或以上性伴侶;27.8%接受一夜情;91.7%接受婚前性行為;25%同時有多於一位性伴侶。25%曾患性病;41.6%曾經墮胎。8.3%之衣原體篩查結果呈陽性反應。相比起吸食氯胺酮達3年以上的少女, 吸食3年或以下的較少患性病或同時有多於一位性伴侶。濫用氯胺酮時間愈長者,會較多有墮胎經歷。年紀愈小開始吸食氯胺酮,也會較早開始發生性行為。結論:濫用氯胺酮少女性觀念開放,及多有高危性行為。同時亦有高的感染性病率及墮胎率。此高危族群需受到關注,以免出現高危性行為的後遺症問題。 主要詞彙: 濫用藥物、氯胺酮、性病、性觀念、高危性行為 Introduction There has been a progressive liberalization in attitudes towards sex in many Asian societies which had previously been comparatively conservative. The age of sexual debut has been decreasing worldwide.1 Similar trend is seen in Hong Kong. The number of 15-18 years old females having sexual experience has increased from 5.2% in 2001 to 8.2% in 2006.2,3 This increase in sexual activity has increased the vulnerability of young people to sexually transmitted diseases (STDs). The United Nations had estimated that about half of new HIV infections worldwide will occur among young people aged 15 to 24.4 Methods The study was carried out in Prince of Wales Hospital in Hong Kong, from November 2009 to February 2010. All non-pregnant Chinese women who had a previous history of ketamine use were referred to our gynaecology clinic from a local drug rehabilitation centre. All of them who attended our clinic were invited and those who refused to join the study were excluded. A written explanation of the study was provided by a female research assistant and written informed consent was obtained. Participants filled in a 47 item questionnaire (Appendix 1) in a private room. The questions were designed so that they could reflect the participant’s sexual attitude and behaviour. Trained researchers provided explanations if required and reviewed the questionnaire for completeness. The questionnaire included 19 items on pattern of ketamine use and use of other illicit drugs. Sexual attitudes, sexual behaviour, contraception practice and history of STD were explored with 20 questions. Most questions were in a yes or no format and option of “no comment” was provided. Demographic data were also obtained. The participants would then be interviewed by a researcher and asked about gynaecological and obstetrics history, details of STD acquired and treatment received. All participants were interviewed by the same investigator who was blinded to the questionnaire results. Screening for STD include hepatitis B surface antigen (HbsAg), anti-hepatitis C virus antibodies (anti- HCV), HIV, Venereal Disease Research Laboratory test (VDRL) and high vaginal swab for bacterial culture, endocervical swabs for gonorrhoea and Chlamydia cultures. Chi square test was used to compare categorical variables. Fisher's exact test was used when there were more than 20% of cells with an expected value of less than 5 in a contingency table. Analysis of variance (ANOVA) was used to compare categorical variables with continuous variables. All analyses were performed with the Statistical Package for Social Science version 17.0 (SPSS Inc., IL, USA). The significance level was set as P < 0.05 Ethics Approval: The study was approved by the local institutional ethics committee (CRE Ref: 2009.453). Results During the study period, 38 ketamine users were referred to our unit for assessment and 36 agreed to participate in the study. All of them filled in the questionnaire and were interviewed by the investigator. Thirty-five out of the 36 participants underwent STD screening. STD screening was not performed in one participant because she was not sexually active. The demographic data and pattern of ketamine use were shown in Table 1 and 2 respectively. The mean age was 19.8 (SD = 3.41) years (range 13 to 29 years old). Details of sexual behaviour and contraception were shown in Table 3 and Table 4 respectively.Nine (25%) reported a history of STD or pelvic inflammatory disease . Among them, three had Chlamydia, two had trichomonas, one had gonorrhoea, one had syphilis, one had genital warts and one had tubo-ovarian abscess (Table 5). All nine reported completion of treatment before the current consultation. However, STD screening performed at the time of study in all sexually active participants (n=35) detected Chlamydia infection in 8.3% and reactive VDRL in 2.8% (Table 5). Besides, 22.2%, 11.1% and 8.3% had one, two or three termination of pregnancies respectively (Table 5) and 2 (5.6%) had a previous confinement. Comparing the 2 groups (ketamine use ≤ 3 years and > 3 years) with Chi square test, less participants in the group with ketamine use of ≤ 3 years had more than 1 sexual partner at the same time (P < 0.05, OR 0.136, 95% CI = 0.024 to 0.775) or had history of STD (P < 0.05) (Table 6).A one way between groups analysis of variance test indicated a statistically significant difference in age of first sexual intercourse among the 6 age-groups of first ketamine use (P = 0.02). Post hoc comparison indicated that age-group 10 to 12 was significantly different from age-group older than 18 years old (P < 0.05, Table 7). Taking ketamine at a younger age was related to having first sex at a younger age.Similarly, there was also a statistically significant difference in number of termination of pregnancy between the 5 groups of duration of ketamine use(P = 0.02). Post hoc comparison indicated that the number of termination of pregnancy in the duration-group of more than 2 to 3 years of ketamine use was significantly different from the more than 6 years of ketamine use duration-group (P < 0.05, Table 7). Longer duration of ketamine use was related to more termination of pregnancies.There was no statistically significant difference between the frequency of contraceptive use with or without ketamine use (P = 0.70).The frequency of ketamine use was not found to be related to the number of termination of pregnancy (P = 0.89) or history of STD (P = 0.67). Discussion Our study included young female ketamine users with a mean age of 19.8 years (SD = 3.4) and an education of up to secondary level. They had a more permissive sexual attitude. Their acceptance towards premarital sex or having mor e than one s exua l partner were as high as 91.7% and 25% respectively, comparing with 44% and 7% among 14 to 17 years old reported in another local study.2 This permissive attitude explained their much higher prevalence of sexual activity (97.2%) as compared with 8.2% reported in another local study.3 The age of first sexual intercourse was significantly lower for those who started taking ketamine at 10 to 12 years of age (mean 13.4 years of age) compared to those who started taking ketamine at >18 years of age (mean 17.5 years). Ketamine user were also more likely to engage in high risk sexual activity with 36.1% having more than one sexual partner at the same time and 52.9% had more than five life time sexual partners, 8.4% even had more than ten life time sexual partners. These results show that ketamine users have much higher risky sexual behaviours and have more consequences of high risk sexual behaviours such as having STD which were shown in the other results of this study.Up to 25% of participants had a history of STD and 11.1% were found to be suffering from STD during our screening. This was much higher than 1.5% to 8.9% in other Asian countries.10,11 Less participants in the group of less than or equal to 3 years of ketamine use had history of STD when compared to the group with ketamine use for > 3 years (P = 0.05). Duration of ketamine use can be regarded as an indirect reflection of the duration of an individual’s overall high risk behaviour. Therefore longer duration of ketamine use is associated with longer exposure to high risk sexual behaviour and its consequences, e.g. STD. Ketamine users are a high risk group from a number of perspectives. Targeting them by offering STD screening or education on STD prevention when they present to medical personnel for other problems allows more effective use of limited resources. Selective screening of Chlamydia infection was shown to be effective in reducing incidence of pelvic inflammatory disease.12 Some had proposed to include STD screening and treatment in standard treatment programmes.13 These efforts, from an individual perspective, can promote reproductive health; while, in a global perspective, can reduce the burden of the ever increasing incidence of HIV. However, drug abuse is illegal and this group is difficult to identify. Medical personnel in a primary care setting are in a good position to provide such intervention since drug abuse is associated with various consequences necessitating medical attention. In our study, 41.7% of participants had consulted a doctor for side effects related to ketamine. Appropriate training for general practitioners is important in the delivery of STD Limitations of study Ketamine abuse is limited to a specific population in Hong Kong and it is difficult to find a large sample size of subjects who are willing to participate. To identify them more effectively, healthy promotion, education and collaborations with various organizations which help ketamine users can do. This is also a biased group as they are a hospital clinic-based population. This study is limited by selection bias as they were all female subjects referred from a rehabilitation centre. The conclusion cannot be generalized to the male subjects and it may not reflect the same conditions in all ketamine users in our community. This is a cross-sectional study and cannot address causal relationships between ketamine use and high risk sexual behaviour. Results of this study might also be affected y recall bias and under reporting. However, under reporting generally results in fewer positive findings. It is likely that the positive response will likely be even higher than the ones reported here. Conclusion Acknowledgement This study was financially supported by the Beat Drug Fund 2010, Narcotics Division, Security Bureau,
Jacqueline HS Lee, MBChB (CUHK) Rachel YK Cheung, MBChB (CUHK), MRCOG, FHKCOG, FHKAM (Obstetricians and Gynaecologists) Symphorosa SC Chan, MBChB (CUHK), MRCOG, FHKCOG, FHKAM (Obstetricians and Gynaecologists) Albe WL Pang, Bachelor of Science (University of Queensland) Tony KH Chung, MBBS (University of Sydney), MD (CUHK), FRANZCOG, FHKCOG Correspondence to: Dr Jacqueline HS Lee, Department of Obstetrics & Gynaecology, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, NT, Hong Kong SAR. Email: jaclee@cuhk.edu.hk Reference
|
|