December 2012, Volume 34, No. 4 |
Update Articles
|
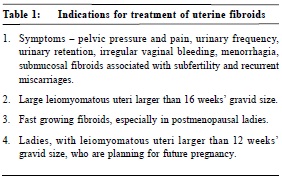
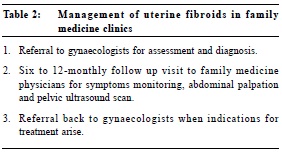
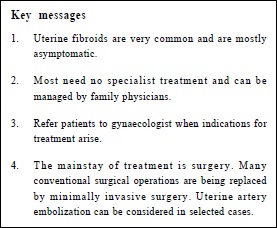
Management of uterine fibroids in primary care medicineChoi-man Yan 忻財敏 HK Pract 2012;34:160-165 Summary Uterine fibroid is a very commonly encountered gynaecological condition seen in primary care.Diagnosis is usually made by ultrasonography. Most cases require no specialist treatment and are suitable for surveillance by family physicians. Patients should be referred for specialist care when indications of treatment arise. The mainstay of treatment for uterine fibroids is surgery. With the various advantages associated with minimally invasive surgery, more and more conventional surgery is replaced by laparoscopic and hysteroscopic operations. Uterine artery embolization is also feasible in selected patients. More studies on safety and effectiveness are required before other newer minimally invasive therapies can be employed. 摘要 子宮纖維瘤是在家庭醫學中常見的婦科病,一般以超音波掃描做診斷。大部分的子宮纖維瘤不需要專科治療,適合由家庭醫生跟進,當病人需要進一步治療時,可轉介病人到婦科專科去處理。藥物不能有效治療子宮纖維瘤,主要治療方法是外科手術。由於微創外科手術的各種優點,越來越多的傳統子宮纖維瘤切除手術被腹腔鏡和宮腔鏡手術所取替。子宮動脈栓塞術也可以選擇性的使用來治療纖維瘤。可是,其他治療方法的使用還需要更多研究來確定。 Introduction Uterine fibroids are the commonest benign tumours in women, with a lifetime risk of nearly 70%.1 In women of reproductive age group, uterine fibroids can be found in one out of every two to three women. Nulliparity and a family history of uterine fibroids are associated factors. Classification and clinical features Most uterine fibroids are asymptomatic . They are classified according to their location: subserosal , intramural , submucosal , cervical , intra-broad-ligamentary, and parasitic (not connected to the uterus). Symptoms are related to the number, size and location. A much enlarged uterus due to either the presence of numerous fibroids and/or big fibroids give rise to pelvic pressure and pain as well as urinary frequency. Fibroids that are incarcerated in the pelvis may cause urinary retention and hydronephrosis. Fibroids that increase the surface area of the endometrium (e.g. submucosal fibroid, fibroid polyp and large intramural fibroids) cause irregular vaginal bleeding and menorrhagia. Submucosal fibroids are also associated with subfertility and recurrent miscarriages. Fibroid polyps may give rise to dysmenorrhoea while pedunculated subserosal fibroid can present with torsion and an acute abdomen. Red degeneration of fibroids in pregnancy may lead to miscarriage or preterm labour. Other pregnancy complications may also occur including malpresentation, obstructed labour and postpartum haemorrhage. Diagnosis Ultrasonography is the mainstay of diagnosis since it is effective, convenient and noninvasive. With higher ultrasound frequency and closer proximity to targets, transvaginal scan can detect uterine fibroids as small as 4-5mm.2 With better tissue penetration, transabdominal scan is more effective in visualizing large uterine fibroids. Magnetic Resonance Imaging (MRI) is excellent for accurate mapping of uterine fibroids as well as assessing the depth of submucosal fibroid penetration. MRI is also a useful adjunct to ultra sound in differentiating uterine fibroids from adenomyosis.3 Indications for treatment Treatmentis considered in the following situations: symptomatic patients, large leiomyomatous uteri larger than 16 weeks’ gravid size, fast growing fibroids, particularly in postmenopausal ladies.Patients with leiomyomatous uteri of 12 weeks’ gravid size and are planning for pregnancy may consider elective myomectomy so as to avoid possible obstetric complications arising from the fibroids. Medical treatment In general, medical treatment is not effective in treating uterine fibroids. Gonadotrophin releasing hormone analogue (GnRHA) is used for preoperative correction of anaemia and shrinkage of fibroids, inducing less blood loss, involving smaller incision wounds and with a minimally invasive approach.7 However, it may lead to blurring of the surgical planes and hence difficulty in enucleation. Small shrunken uterine fibroids may also be missed as a result. There is some evidence that mifepristone and asoprisnil, both antiprogesterone agents, may be effective in reducing the uterine fibroid volume and alleviating symptoms. However, more studies are needed.8 Surgical treatment Surgery therefore is still the main stay of treatment for uterine fibroids. Abdominal myomectomy is the conventional operation for uterine fibroid. Post-operative fever occurs in 12-38% and is likely to be due to haematoma in the myoma bed spaces that have not been fully obliterated.9 The chance of myomectomy converting into hysterectomy because of uncontrollable bleeding is 1-2%.10 Abdominal hysterectomy may also be directly chosen for multiple big uterine fibroids, when patients prefer removing the whole uterus for definitive symptom relief, or when other pathologies co-exist. Vaginal hysterectomy for big leiomyomatous uteri may be difficult. It may involve the need for morcellation of the uterine fibroids before removal. Sufficient vaginal access and uterine descent under anesthesia can make the vaginal approach easier. Vaginal myomectomy may be easy for those uterine fibroids prolapsing out of the cervical os. The stalk is tied and the fibroid removed vaginally. For other uterine fibroids, colpotomy may be required; anterior colpotomy for anterior wall fibroids and posterior colpotomy for posterior wall fibroids. The benefit so flaparoscopic compared to abdominal approach are well recognized, including small incision wounds, better cosmetic result, less blood loss, less tissue trauma, less postoperative pain, shorter hospital stay, and faster recovery. Correct case selection is vital to the success of laparoscopic myomectomy. However, there is no universally accepted criteria for selection, which depends on patient’s characteristics and individual surgeon ’ s skills . In the case of big fibroids , preoperative fibroid shrinkage with GnRHA may be used so that the selection criteria can be met. Preoperative mapping with ultrasonogram, and even MRI, is very important so that small fibroids are not missed during the operation. Laparoscopic myomectomy is a feasible and safe alternative to the conventional open myomectomy in many instances. The major concern is suboptimal tissue apposition during repair of myometrium tissue which can lead to uterine rupture in a subsequent pregnancy. However, if the myometrial repair is performed with the same degree of care as it would be at open myomectomy, there appear stobe no reason why the rate of uterine rupture should be higher after laparoscopic myomectomy.13 The hysteroscopic approach involves resecting submucosal fibroids which have at least 50% protrusion into the uterine cavity. Preoperative GnRHA is given one month prior to procedure so as to facilitate hysteroscopic visualization. There should be less than three uterine fibroids and the size of each is not greater than 2.5cm in diameter.14 Possible complications include fluid overload and electrolyte imbalance, cervical laceration, uterine perforation, bleeding and infection. Laparoscopic hysterectomy has the advantage of a laparoscopic approach, but increases operating time and cost, as well as increases the risk of urinary tract injuries.15,16 Other treatments Uterine artery embolization (UAE) is a safe and effective alternative to surgical treatment. It is not a choice for those who want to retain their fertility since the effect of UAE on future pregnancies is unknown. With antibiotic prophylaxis, bilateral uterine arteries are embolized under X-ray guidance. Analgesia used ranges from general or epidural anaesthesia to medication regimes. A high proportion of patients require opiates for analgesia.17 Post embolisation syndrome is also common, usually occurring towards latter part of the first week when patients complain of low-grade fever, malaise and general discomfort which often settles with conservative management.18 Menorrhagia and pressure symptoms are relieved in most of the patients. Early symptom recurrence appears to be uncommon.18 Overall complications occur in 1-4%, mostly minor.18 Moreover, UAE may also affect ovarian function, resulting in permanent amenorrhoea in 7-14% and 0-3% in patients older than and younger than 40 years of age, respectively.19 In magnetic-resonance-guided focused ultrasound surgery, focused high-energy ultrasound is used to ablate uterine fibroids under magnetic resonance guidance. The fibroid volume reduction is less than that of UAE, but patients do not appear to have post-embolization syndrome.20,21 Laparoscopic destruction of uterine fibroids by heat, cold coagulation or laser is not popular and may result in severe intra-abdominal adhesions.22 Laparoscopic uterine artery occlusion appears to be similarly effective as UAE although more studies are awaited.23,24 All these minimally invasive therapies do not have the uterine fibroid masses eradicated nor are there any histological diagnoses. They are not suitable for patients who desire future pregnancies. Further studies on their safety and effectiveness would be needed. Surveillance in primary care clinics Most patients with uterine fibroids are asymptomatic and can be followed up by family physicians after a clear diagnosis and proper assessment have been made. Twelve-monthly follow up visit with attention to symptoms and abdominal palpation by the family physician is suggested. The uterine size is at least more than 12-week gravid size when the uterus is palpable abdominally, i.e. when the uterine fundus can be felt above the pubic symphysis. Pelvic ultrasonography can be arranged at yearly intervals to monitor the size of uterine fibroids. Referring the patient back to the gynaecologist is necessary when there is indication for surgical treatment. Conclusions Uterine fibroids are very common. Most are sui t abl e for surveillance by family physicians . Indications for referral to gynaecologist care include symptomatic patients, large leiomyomatous uteri, fast growing fibroids, patients whose uterine fibroids are larger than 12 weeks’ gravid size, patients who are planning for future pregnancy and patients suffering from subfertility and recurrent miscarriages in whom no other causes for the suboptimal reproductive outcome are found. With the various advantages of minima l l y invasive surgery (MIS), more and more conventional surgery is replaced by MIS with laparoscopic an hysteroscopic surgery. Conventional surgery still plays a role when MIS is not feasible. UAE can be considered in selected cases and for those approaching menopause or those with no desire for pregnancy and are willing to sacrifice the uterus when complications arise. More studies on safety and effectiveness are required before other newer minimally invasive therapies can be employed.
Choi-man Yan, FRCOG (UK), FHKAM (O&G), FHKCOG Correspondence to: Dr CM Yan, Room 1301, 26 Nathan Road, Tsimshatsui, Kowloon, References
|
|