|
December 2014, Volume 36, No. 4
|
Discussion Paper
|
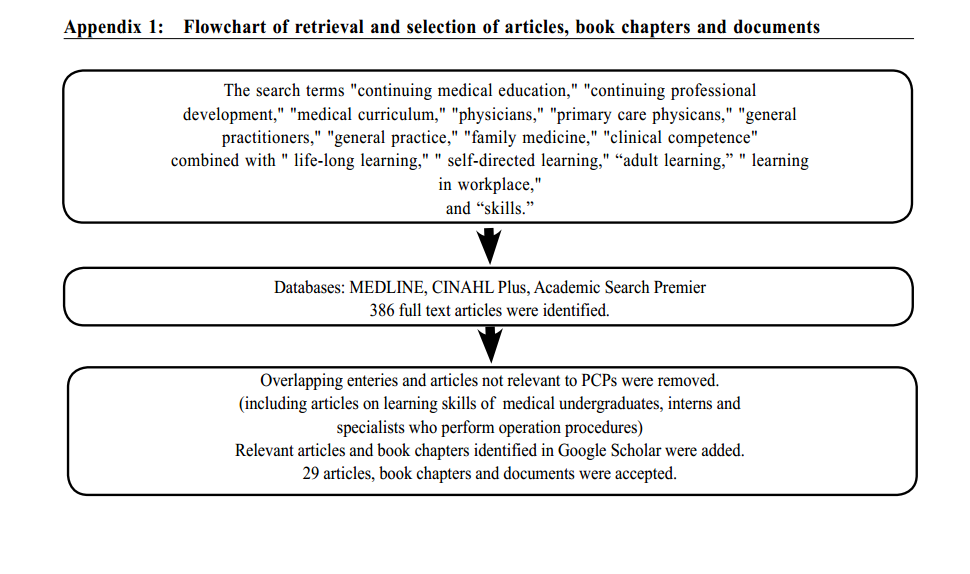
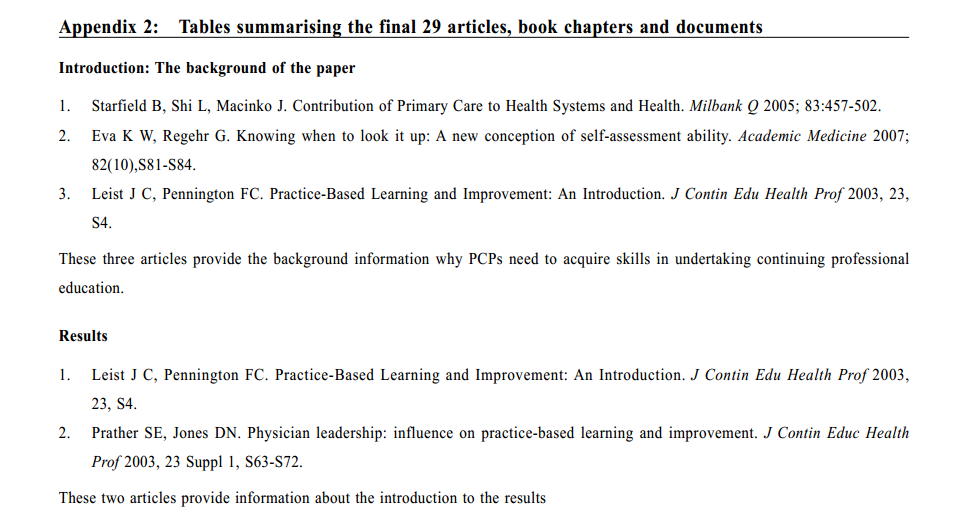
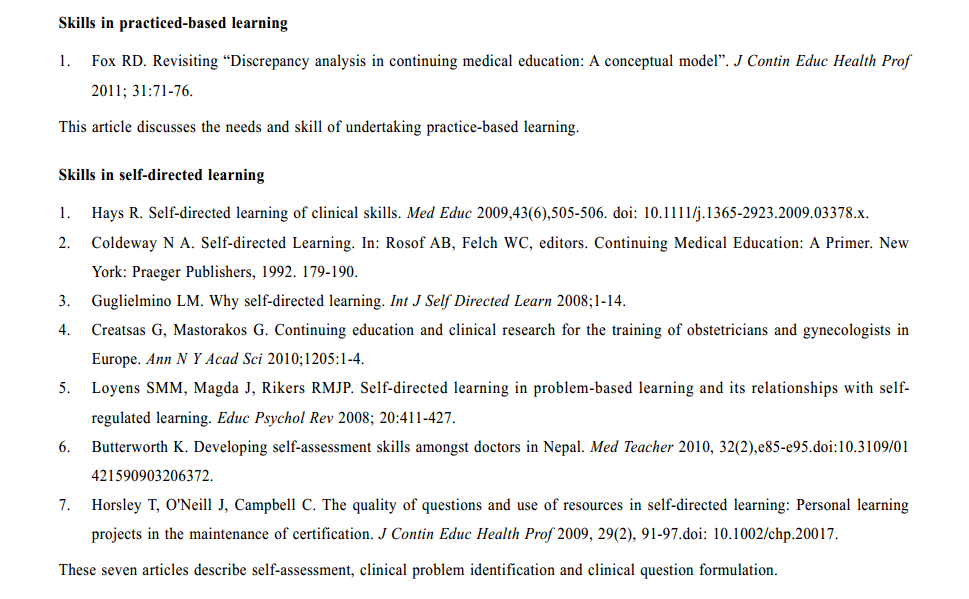
Review on skills in undertaking continuing professional education among primary care physiciansMan-kay Poon 潘文基, Tai-pong Lam 林大邦 HK Pract 2014;36:141-148 Summary Medical knowledge and technologies have made advances more rapidly than ever before. The public is also requesting accountability and transparency of healthcare services. Primary care physicians(PCPs)play the roles of promoting public health, preventing diseases and offering early treatment of chronic diseases to decrease the healthcare burden. Therefore, they need to respond to public's expectations and the changing needs of healthcare services by undertaking continuing professional education. In this article, we discuss the skills which PCPs should acquire in undertaking continuing professional education. The literature is searched for skills in undertaking continuing professional education among PCPs and a review of the skills was made. Critical thinking, information literacy and knowledge management are essential skills. Traditional undergraduate medical curriculum emphasises on didactic teacher-centred learning. Reformed medical curriculum is focused on training students the skills to prepare them to pursue continuing professional education in their working lives.PCPs who acquire the skills can learn independently addressing their learning needs in their workplace. PCPs should acquire skills in undertaking continuing professional education to maintain and improve their clinical competency. 摘要 現在醫療知識和技術發展突飛猛進,速度比以往任何時候都快。公眾要求醫療機構的服務要有問責性和透明度。基層醫生的角色主要是促進公共衛生及健康,預防疾病,為患有慢性疾病的病人提供早期治療,以減少社會的醫療負擔。因此,他們需要通過在職的持續專業學習以改善服務,滿足公眾的期望和不斷變化的醫療服務需求。本文是從學術文獻中檢閱基層醫生應掌握持續專業學習的資料,從而概述他們應掌握持續專業學習的技能。持續專業學習是一種在職的自我主導的終身學習。基層醫生應該有批判性思維,理解信息和知識管理的能力。傳統的本科醫學課程強調老師為中心說教式的學習。改革後的本科醫學課程,注重培養醫科學生主導的終身學習技能,以適應未來工作的需要。基層醫生獲得持續專業學習的能力,以便他們可以在工作的場所獨立解決工作的挑戰。基層醫生應該掌握持續專業學習的技能,以保持並提高他們治病的能力。 Introduction In many big-income countries and regions including Hong Kong,ageing populations and high prevalence of chronic illness have resulted in higher healthcare expenditures. Primary care physicians (PCPs), who provide first contact, convenient, comprehensive, timely and continuous care to the public, have a role in promoting public health and offering early management to patients with chronic diseases to decrease the healthcare burden.1Knowledgeable and skilful PCPs are expected not only to improve practice outcomes, but also to contribute to healthcare system sustainability. Much medical information is available on the Internet, resulting in the general public being able to request for more accountability and transparency of healthcare services. With rapid advances in medicine and technology, PCPs must undertake life-long learning after their medical graduation to maintain and improve clinical competence.2 The traditional continuing medical education (CME) lectures are not able to address all the specific learning needs of PCPs.3 This article is focused on the skills which PCPs should attain to pursue continuing professional education. In this article, continuing professional education refers to any clinical practice relevant learning activities which PCPs undertake. Methods Cambridge Dictionaries Online describes skill as an ability to do an activity or job well, especially because you have practised it. Good outcome brought by the learned capacity is emphasised in the definition. In the literature review, we focus on the medical doctors’ learned capacities which bring forth the solutions of clinical problems in the problem-solving process. A literature search was conducted using electronic databases through MEDLINE, CINAHL Plus, Academic Search Premier and Google Scholar.We used the search terms “continuing medical education”, “continuing professional development”, “medical curriculum”, “physicians”, “primary care physicians”, “general practitioners”, “general practice”, “family medicine”, and “clinical competence” combined with the terms “life-long learning”, “ self-directed learning”, “adult learning”, “ learning in workplace”, and “skills”. We used Google Scholar to search for the relevant articles, book chapters and documents to broaden our database. We selected the materials relevant to PCPs fulfilling the following criteria: “learning skills in CME and Continuing Professional Development”, “learning skills in self-directed learning and workplace learning”, and “learning skills trained in traditional and reformed undergraduate medical curricula”. Articles about skills in self-directed learning and workplace learning in general were also considered because majority of studies on learning skills were focused on medical students, interns and specialists who perform operative procedures. No restriction was applied on the study design. We excluded articles on learning skills for operative procedures, and those targeting medical undergraduates and interns. Only studies published in English after 1989 were included. Results Twenty nine English articles, book chaptersand documents were accepted using the key words and combinations of them. (Appendix 1 and 2) Patient management is directly related to clinical context. As a "bottom-up approach", clinical problem guides the PCPs to acquire what they need to improve their performance in practice.3 CME refers to life-long medical education which fulfils the criteria of accreditation institutes. PCPs may solve their clinical problems by participating in the available content relevant CME activities. With the rapid advances of medical knowledge and computer technology, PCPs need to adapt for the changing practising environment. Otherwise, their medical care services are deemed to be out-dated.4 The format of continuing professional education gradually evolves from CME into a practice-based self-directed approach in which new learning skills are needed. Observations 1) Skills in practice-based learning Competence in both medical knowledge and clinical skills are essential for PCPs to enhance practice outcomes. The gap between clinical knowledge and actual practice can be overcome by practice-based learning. This is because PCPs encounter context specific clinical problems in daily clinical practice and need to solve these problems to achieve the clinical outcomes at the point of care.5 In practice-based learning format, PCPs do not need to await the relevant CME activities to acquire the knowledge to solve their clinical problems and their learning is directly addressing their clinical problems. Therefore, practice-based life-long learning addresses and responds to the clinical problems and the changing needs of patients in clinical practice. 2) Skills in self-directed learning To maintain high clinical competence, PCPs have the responsibility to determine their clinical needs.6 Clinical problems drive PCPs to undertake practice-based life-long continuing professional education in self-directed approach, rather than to follow the pre-designed CME programmes. In self-directed approach, PCPs have the initiatives and responsibility in the whole learning process, from actively identifying learning needs, setting learning objectives, adopting appropriate learning methods, achieving and evaluating the learning outcomes.7 In this approach, three elements which are related to the motivation and direction of learning are context, motivation and universality of learning.8 Firstly, the context is the learning environment which determines what PCPs will learn and allow them to explore their needs and curiosity. In a facilitating learning context, self-directed learning is more effective to help PCPs to achieve learning outcomes,compared with learning in an environment which they are required to comply with institutional regulations. The attitudes and work arrangements of their working practices are important factors to determine their self-directed learning in workplace. For instance, forming study group in workplace can facilitate self-directed learning. In this self-directed learning process, a sense of personal responsibility is developed and enhanced.9 Secondly, motivation of self-directed learning among PCPs is determined by their personal values, attitudes and abilities whichshape the learning in a continuum of different degrees among PCPs. It is their own choice what they should learn in their workplace. Thirdly, in the learning process, they will acquire the ability to create meaning, and reflect and integrate what they have learned to solve their problems. This learning ability is not only restricted to one specific discipline, but also can be generalised to other disciplines. This capacity is stated as the universality of the acquired learning skill. In return, theircompetent problem solving capacity will facilitate them to participate in more self-directed learning in the future.8 Since continuing professional education is shaped by personal factors, social practices, cultural factors, regulations of the working practices and societal expectations, no single approach of continuing professional education matches all PCPs’ learning needs.9 Self-directed learning is so highly flexible thatPCPs determine their own learning foci and strategies, and independently manage the learning activities under their own control.10 However, self-reflection on PCP’s self-assessment of their clinical needs is shown to be inaccurate.11 The low achievers over-estimate their abilities while the high achievers under-evaluate theirs. Accurate self-assessment of their medical knowledge and clinical capacity can be improved over time with the help of evaluation from their peers and mentors. This capacity helps PCPs to recognise their clinical problems.11 To engage in efficient self-directed learning after identifying the clinical problems, PCPs should be able to formulate appropriate clinical question which consists of population, intervention, comparison and outcome, and the level of evidence of the collected information.12 Acquired the capacity, PCPs could be able to identify the required information in response to the public demands and expectations.9,11 3) Skills in information literacy and knowledge management Obtaining the ability to identify clinical problems and formulate the appropriate clinical questions, PCPs should acquire information literacy which is the capacity to locate, evaluate and analyse the relevant information and transfer the knowledge into their practice.13 Computer literacy, the ability of using computer in information management is an indispensable part of information literacy because computer is a tool for PCPs to access the required information on the Internet anytime and anywhere. PCPs should be able to locate their required details in loads of irrelevant information on the Internet.14 They can seek information on specific clinical problems and newly advances on medical knowledge through the Internet websites, such as Medscape, Skyscape and National Institutes of Health (NIH). Although the learning format of online learning is different from the traditional one, online CME learning was shown to be as effective as traditional CME format in terms of knowledge transfer.15 Further, PCPs who participated in online learning were shown to be able to improve their medical knowledge and practice pattern.10,16 Knowledge management is another imperative ability of competent PCPs in self-directed learning.13 Through the application of the information to their clinical problems, they gain experiential knowledge which allows them to put the new information into context to solve their problems. They are able to integrate and generate new knowledge in the process, rather than just recalling the relevant information. 4) Skills in critical thinking and problem solving training Every day, PCPs are required to solve clinical problems by their knowledge and skills in their practices. They pursue continuing professional education which is different from the formal medical education in medical schools. The former one is practice-based life-long learning undertaken in workplace while the latter one is learning between teachers and students in classroom in their medical study period.17 The factual medical knowledge which they acquired in medical schools is no longer enough for them.18 In practice, they need to identify what they should know and prioritise their own learning needs. Therefore, they should be not only competent in information literacyand knowledge managementbut also problem solving capacity which requires them to have the abilities of critical thinking, clinical reasoning and decision making in undertaking continuing professional education.19,20 Critical thinking is a reflective learning process which enablesPCPsto keep open-minded and compare, analyse, judge and challenge the assumptions, conduct inductive reasoning, and make rational and logical deduction.21 At the same time, theyare able to tolerate uncertainties and refuse to accept premature conclusion.20
In 1993, “Tomorrow’s Doctor”, a document published by the General Medical Council criticised that the traditional undergraduate medical curriculum which emphasised on memorisation and regurgitation of medical information was unable to fulfil the expected role of PCPs in providing holistic and compassionate care to patients.22 Since problem-based learning was shown to be effective to promote critical thinking, new curriculum based on problem-based approach was designed and gradually introduced to medical schools.23 The curriculum is emphasised on enhancing the medical graduates’ critical mind and self-directed learning ability to pursue self-directed continuing professional education to face the challenges in their future working lives.24 The learning outcomes of medical graduates trained in the new medical curriculum were evaluated and it was revealed that they had improved problem solving skills and self-directed learning ability, compared with graduates trained under traditional medical curriculum.25 The new medical curriculum can train the graduates to attain critical thinking and self-directed learning ability which are shown to be sustainable.26,27 The medical graduates trained in new curriculum also show better performance in general competence skills including communication skill, scientific attitudes and working in a team and improvement in social ability.27,28 Subjective assessment of medical knowledge among the graduates of the reformed curriculum was lower than that of the traditional ones. However, objective assessment of medical knowledge of the graduates trained in reformed curriculum revealed that their knowledge was comparable to those trained in traditional curriculum.29 The younger PCPs received the self-directed problem-based learning and critical thinking training in new curriculum while the senior PCPswho were trained in traditional curriculum did not receive the training. The behaviours of knowledge seeking and clinical problem solving capacity were demonstrated to be different between these two groups of PCPs, echoing what they were taught in their medical education programme.29 Senior PCPs need to acquire these skills in recognising their education needs, constructing the clinical problems and finding out the solutions by themselves. Besides problem solving skills and self-directed learning ability, the computer literacy of the senior physicians were also identified to be less competent than the junior ones.14 Another review showed that the PCPs trained under a problem-based medical curriculum were more capable to cope with uncertainties and gave more consideration to ethical and legal aspects in practice.20 They were also found that in their daily practice they improved their self-directed life-long learning ability and tended to search for their required information on the Internet in which rich medical information is readily available. The new medical curriculum was shown to be able to prepare the graduates to pursue self-directed continuing professional education in their daily practice while graduates from traditional curriculum have much room to improve in this area. Conclusions The learning needs of PCPs are highly individualised and context specific. No single approach of learning is appropriate to all PCPs. Practice-based self-directed learning is flexible and address the clinical problems encountered in practice. To maintain and improve clinical competence, PCPs need strong skills in critical thinking, information literacy and knowledge management to undertake the practice-based self-directed life-long learning. Although PCPs taught under traditional undergraduate medical curriculum were not trained in the problem-solving and self-directed learning skills, patients request their medical services to be up-to-date and evidence-based. The PCPs who are not proficient in these skills are better to take effort to enhance their ability to meet the daily challenges.
Man-kay Poon, MBBS (HK), PDipComPsychMed (HK), PDipIntMed&Therapeutics (HKU), Tai-pong Lam, MBBS (W Australia), PhD (Sydney), MD (HK), FHKAM (Family Medicine) Correspondence to: Dr Man-kay Poon, Shop 4, G/F, Billion Court, 147 Main Street Ap Lei Chau, Hong Kong SAR, China. References
|
|