How well can family physicians manage
osteoporosis? A retrospective case series in
a local public clinic in Hong Kong
Pui-kwan Chan 陳佩君, Vincent WS Li 李穎信, Yim-chu Li 李艷珠, Catherine XR Chen 陳曉瑞
HK Pract 2023;45:70-78
Summary
Objective:
To explore the clinical effectiveness among
osteoporotic patients, in terms of DEXA T-score
improvement, of Multidisciplinary Osteoporosis Clinic
(MOC) which was organised by primary care physicians
in a local primary care clinic.
Design:
A Retrospective case series
Subjects:
All osteoporotic patients who had attended
MOC of Kowloon Central Cluster during the period 1
January 2015 to 31 December 2018.
Main outcome Measures:
Primary outcomes:
1. Changes in DEXA T-score
after two years of management at MOC.
2. Subgroup
analysis: 2-year interval DEXA T-score changes among
patients with or without history of fragility fracture;
and among patients with or without pharmacological
treatment.
3. Serial interval DEXA T-score changes
of recruited patients who had completed 5 years of
bisphosphonate treatment.
Secondary outcome: The occurrence of new
osteoporotic fracture during two years of management
in MOC.
Results:
A total of 186 osteoporotic patients were
recruited in this study. After two years of management
at the Multidisciplinary Osteoporosis Clinic (MOC),
there was an improvement in the T-scores at the lumbar
spine and femoral neck, from -2.71±0.76 to -2.35±0.83
and -2.40±0.75 to -2.10±0.76 respectively (P <0.001).
For subgroup analysis on patients with or without a
history of fragility fracture and patients with or without
bisphosphonate treatment, improvement in T-scores of
both lumbar and femoral neck were all significant at
two years (P <0.05).
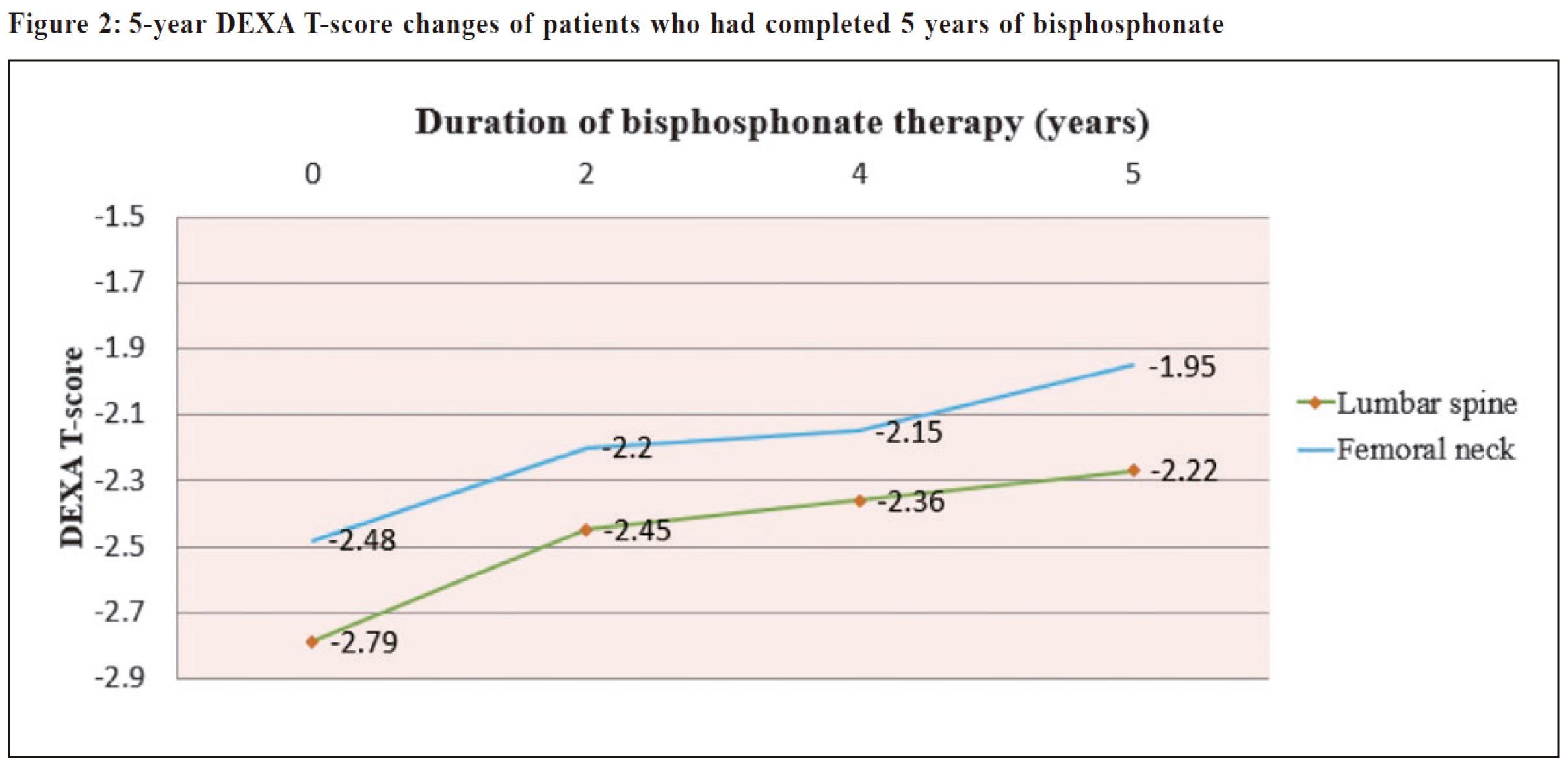
Among those who had completed 5 years of
bisphosphonate therapy, progressive improvement
in T-scores of both lumbar and femoral neck were
observed (P <0.001).
One patient suffered from new fragility fracture during
the two-year follow up period.
Conclusions:
Multidisciplinary Osteoporosis Clinic (MOC)
run by family physicians in the public primary care
setting could effectively treat osteoporotic patients with
significant improvement in DEXA T-scores.
Keywords:
Family physician, osteoporosis, primary
care, multidisciplinary
摘要
目的:
探討由初級保健醫師組織的多學科骨質疏鬆症診所(MOC)在當地初級保健診所的骨質疏鬆患者中的臨床效果。
設計:
回顧案例系列
對象:
所有在2015年1月1日至2018年12月31日期間參加九龍中聯網MOC的骨質疏鬆症患者。
主要觀察指標:
主要結果:
(1) 在MOC管理兩年後DEXA T-score的變化。
(2) 亞組分析:有或無脆性骨折病史的患者2年間隔DEXA T-score變化;以及在接受或未接受藥物治療的患者中。
(3) 已完成5年雙膦酸鹽治療的招募患者的連續間隔DEXA T評分變化。
次要結果:
在MOC的兩年管理期間發生新的骨質疏鬆性骨折。
結果:
共招募了186名骨質疏鬆症患者。MOC治療2年後,腰椎和股骨頸T值分別從-2.71±0.76提高到-2.35±0.83和-2.40±0.75到-2.10±0.76 (P<0.001)。對有無脆性骨折病史的患者和有無雙膦酸鹽治療的患者進行亞組分析,腰椎和股骨頸T值在兩年時均有顯著改善(P<0.05)。
在完成5年雙膦酸鹽治療的患者中,腰椎和股骨頸的T值均逐漸改善(P<0.001)。
一名患者在兩年的隨訪期間出現了新的脆性骨折。
結論:
由家庭醫生在公共初級保健環境中運行的MOC可以有效治療骨質疏鬆症患者,DEXA T評分顯著提高。
關鍵詞:
家庭醫生,骨質疏鬆症,基層醫療,多學科
Introduction
With the ever-ageing population and longer life
expectancy, osteoporosis is increasingly becoming a
global health concern.1 Currently it is estimated that
more than 200 million people suffer from the disease
worldwide.2 Approximately 30% of all postmenopausal
women have osteoporosis in the United State and
Europe.3 According to a meta-analysis published
in 2016, there has been an obvious increase in the
prevalence of osteoporosis in China over the past 12
years (prevalence of 14.94% before 2008 and 27.9%
during the period spanning 2012-2015). The pooled
prevalence of osteoporosis in people aged 50 and older
was 34.7%.4 In another local study, the prevalence of
osteoporosis in Hong Kong Chinese females increase
with age dramatically. In women aged 70 or above, over
half have osteoporosis at the hip.5
Despite the enormous social and economic impact
of osteoporosis and its related complication, namely
fracture, osteoporosis remains under-diagnosed and
under-treated worldwide.6
According to the Osteoporosis Society of Hong
Kong, much of the responsibility for delivering
effective treatment to osteoporotic patients falls on
endocrinologists and orthopaedic surgeons in Hong
Kong. With the long waiting time in specialty clinics,
many patients miss the golden time for treatment,
i.e. before the happening of fragility fractures and its
associated morbidity and mortality. Meanwhile, our
counterparts in Australia play a major role in managing
osteoporosis in the community.7 We believe family
physicians in Hong Kong can also take on an active
role in combating osteoporosis. Therefore, a dedicated
Multidisciplinary Osteoporosis Clinic (MOC) was set
up at Yau Ma Tei Family Medicine Specialist Clinic
(FMSC), Department of Family Medicine & General
Outpatient Clinic of Kowloon Centre Cluster (FM &
GOPC, KCC) in 2010. The objective of setting up this
clinic was to provide comprehensive management for
osteoporotic patients within the primary care setting
and to enhance community-based care. However, to
date, studies are lacking in the evaluation of the clinical
effectiveness, in terms of improvement in bone mineral
density (BMD), of osteoporosis management by primary
care physicians.
Objective
This study aims to evaluate the clinical
effectiveness of MOC, in terms of DEXA T-score
improvement of osteoporotic patients. Through MOC,
we believe we could provide effective treatment
to patients and fill the service gap in osteoporosis
management in Hong Kong.
Methods
The multidisciplinary osteoporosis clinic (MOC)
Patients with confirmed osteoporosis or osteoporosis
related conditions such as history of fragility fractures
were referred to MOC for further management. The
referring source was mainly from different GOPCs
of KCC and other primary care providers in Hong
Kong. This multidisciplinary clinic was specially
designed to cater the needs of osteoporotic patients.
Patients referred to the clinic were invited to a
Community Based Specialty Nursing Session which
included a health talk on osteoporosis and an individual
counselling session. Fracture risk assessment tool
(FRAX), a scoring system assessing one’s 10-year
osteoporotic fracture risk based on the individual’s
clinical risk factors as well as BMD at the femoral
neck8, was used and FRAX score was calculated during
the session. Advice was given accordingly.
After the nursing educational session, a doctor
consultation session was arranged in the following
weeks. Doctors conducting the consultation acquired
at least fellowship qualification of both Hong Kong
College of Family Physicians (HKCFP) and Royal
Australian College of General Practitioners RACGP
(RACGP). In addition, they were trained and equipped
with updated knowledge regarding osteoporosis
management via a training session. The consultation
time was on average 15 minutes per patient, which was
longer than the 7-minute consultation time in GOPC.
This was to ensure sufficient time had been given to
attending doctors to formulate a comprehensive and
whole-person management plan with patients.9 Exercise
and nutrition are essential elements in combating
osteoporosis. Therefore, allied health services such as
dietitian counselling, physiotherapy and occupational
therapy was included in the management plan as needed.
Bisphosphonates are recommended as first line
treatment in most guidelines including the National
Osteoporosis Foundation (NOF) guidelines and the
American Association of Clinical Endocrinologists
(AACE) guidelines.10,11 Oral alendronate is the only
pharmacological agent that can be reimbursed via the
Hong Kong Hospital Authority (HKHA) for patients
with a history of osteoporotic fracture. Therefore,
guideline directed medical therapy, namely alendronate
was regularly prescribed in our clinic. Calcium and
Vitamin D supplement were also regularly prescribed.
Dual X-ray absorptiometry (DEXA) scan was
performed upon joining MOC, i.e. baseline DEXA
scan. It was repeated after 1-2 years of initiating
pharmacological treatment and every 2 years thereafter
if BMD had been stabilised or improved, compatible
with most guidelines’ recommendations.10-12 After 5
years of bisphosphonate therapy, patients were offered a
drug holiday.
To ensure uniform data comparisons, patients were
urged to have their DEXA scans repeated in the same
diagnostic center, assuming the same DEXA machine
was used. Doctor follow up appointment was arranged
depending on clinical needs.
Study Design
Retrospective case series study conducted in a FM
(Family Medicine) clinic in the public setting
Subject
Inclusion criteria
All osteoporotic patients, coded by International
Classification of Primary Care (ICPC) L95
(osteoporosis) , who had a t tended MOC of the
Department of FM & GOPC, KCC from 1 January 2015
to 31 December 2018.
Exclusion criteria
-
Osteopenia patients
-
Osteoporotic patients due to secondary causes
such as osteoporosis due to endocrine diseases or
corticosteroid use
-
Osteoporosis patients who had been followed up by
other specialists or private doctors
-
Osteoporotic patients who had been treated with
osteoporosis medication before joining MOC,
Osteoporosis medication means any type of bone
antiresorptive and anabolic drugs, not including
vitamin D and calcium supplement
-
Osteoporotic patients who had no baseline DEXA
scan
-
Osteoporotic patients who had no interval DEXA
scan
Definition of Osteoporosis
Dual X-ray absorptiometry (DEXA) is the gold
standard and most precise technique for BMD (Bone
mineral density) measurement.13 Osteoporosis was
defined as DEXA T-score of ≤ -2.5, according to the
World Health Organization.14
Determination of variables
The recruited patients’ age, gender, ethnicity,
smoking status, drinking status, body mass index (BMI),
family history of fracture, past history of fracture, other
past medical history or co-morbidities, menopausal
status (for female), age of menopause, FRAX score
were retrieved from nursing consultation notes of
Clinical Management System (CMS) of HKHA. The
BMI was calculated as body weight (kg)/body height2
(m2). The patient was considered a smoker if he/she
was an active smoker or had quit smoking within 6
months. Baseline blood test including complete blood
count, liver function test, calcium level, phosphate level
and thyroid function test of patients were collected
from the CMS (Clinical Management System) of HKHA
(Hong Kong Hospital Authority).
Baseline and 2-year interval DEXA T-scores were
collected. Baseline DEXA T-score was the T-score of
DEXA scan performed upon joining MOC, within one
year before or after first doctor consultation. The 2-year
interval DEXA T-score was the T-score of the DEXA
scan performed at or nearest to 2 years after joining
MOC. The serial interval T-scores of those who had
completed 5 years of bisphosphonate were collected.
These data were retrieved from doctor consultation
notes from CMS of HKHA. If in any doubt, the original
copy of DEXA report was referred to. The occurrence
of new osteoporotic fractures documented in the
consultation notes was also recorded.
Study Design
Primary outcomes
-
Changes in DEXA T-score of recruited osteoporotic
patients after two years of management at MOC.
-
Subgroup analysis: 2-year interval DEXA T-score
changes among patients with or without history
of fragility fracture; and among patients with or
without pharmacological treatment
-
Serial interval DEXA T-score changes of recruited
patients who had completed 5 years of bisphosphonate
Secondary outcome
The occurrence of new osteoporotic fracture of
recruited osteoporotic patients
Sample size calculation
From previous studies, the mean BMD difference
between treatment and non-treatment group was 0.03 g/
cm2, with a SD of 0.13.15,16 At 95% confidence level and
a power of 0.8, with the use of paired sample T test for
sample size calculation, the sample size required is 147.
To allow the room for data exclusion (~20%), totally 186 patients were included into the data analysis.
Statistical Methods
All data were entered and analysed using a
computer software (SPSS version 23, Chicago, IL, US).
Categorical variables were presented as frequencies
and percentages. Continuous variables were presented
as mean, plus standard deviation. Paired Student’s
t test was used to analyse continuous variables. All
statistical tests were two-sided, and a P value of <0.05
is considered significant.
Ethical approval
This study was approved by the Hong Kong
Kowloon Center / Kowloon East Cluster Research
Ethics Committee, with reference number: KC/KE-18-
0183/ER-1.
Results
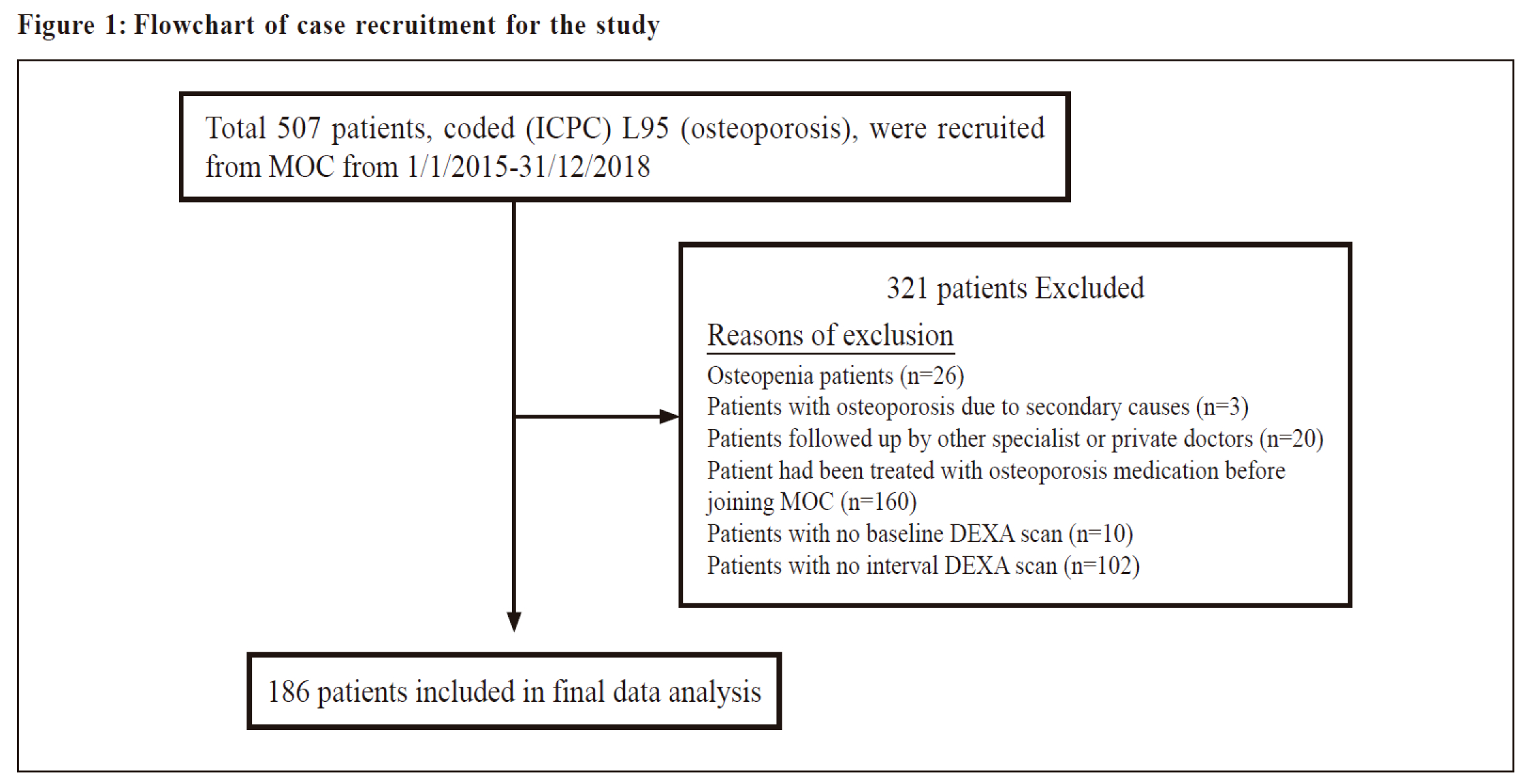
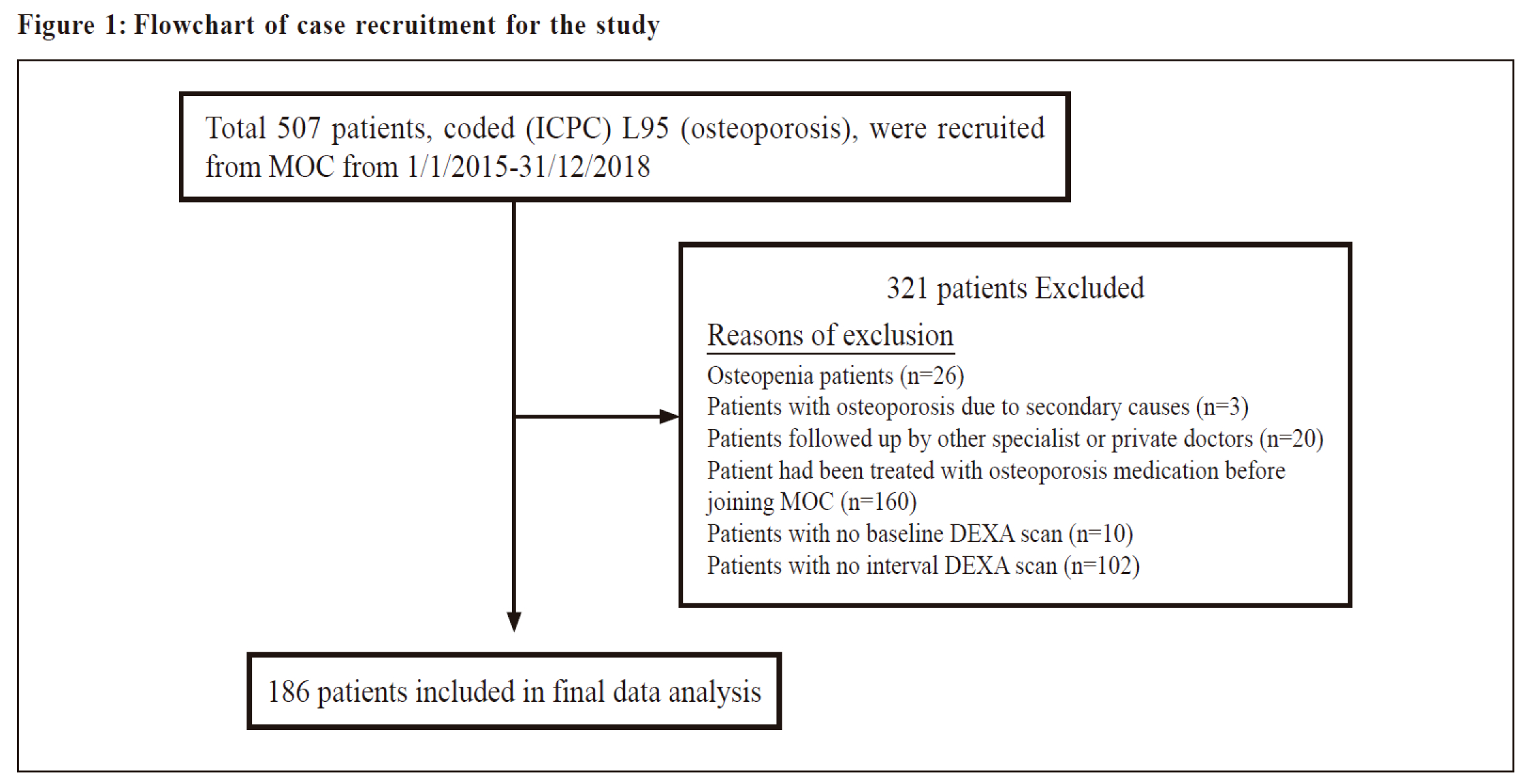
A total of 507 patients with ICPC coding L95
(osteoporosis) attended MOC during the period 1/1/2015
to 31/12/2018. In the final data analysis, 186 patients
were included. Among the 321 excluded patients,
majority of them were excluded because they had been
treated with osteoporosis medication by other doctors
before joining MOC (N=160, 50%) or they had no
interval DEXA scan performed during the study period
(N=102, 32%). The flowchart of case recruitment is
summarised in Figure 1.
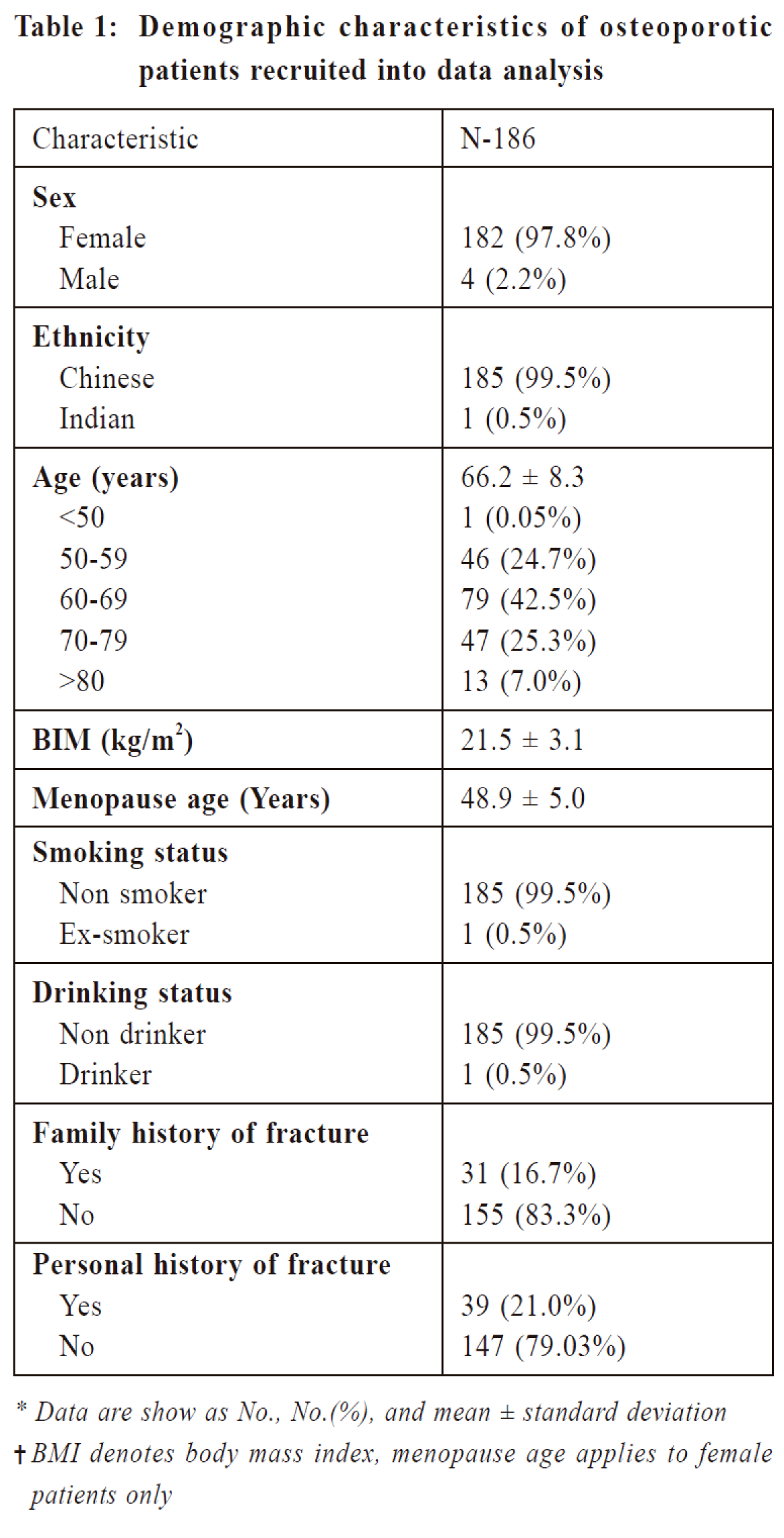
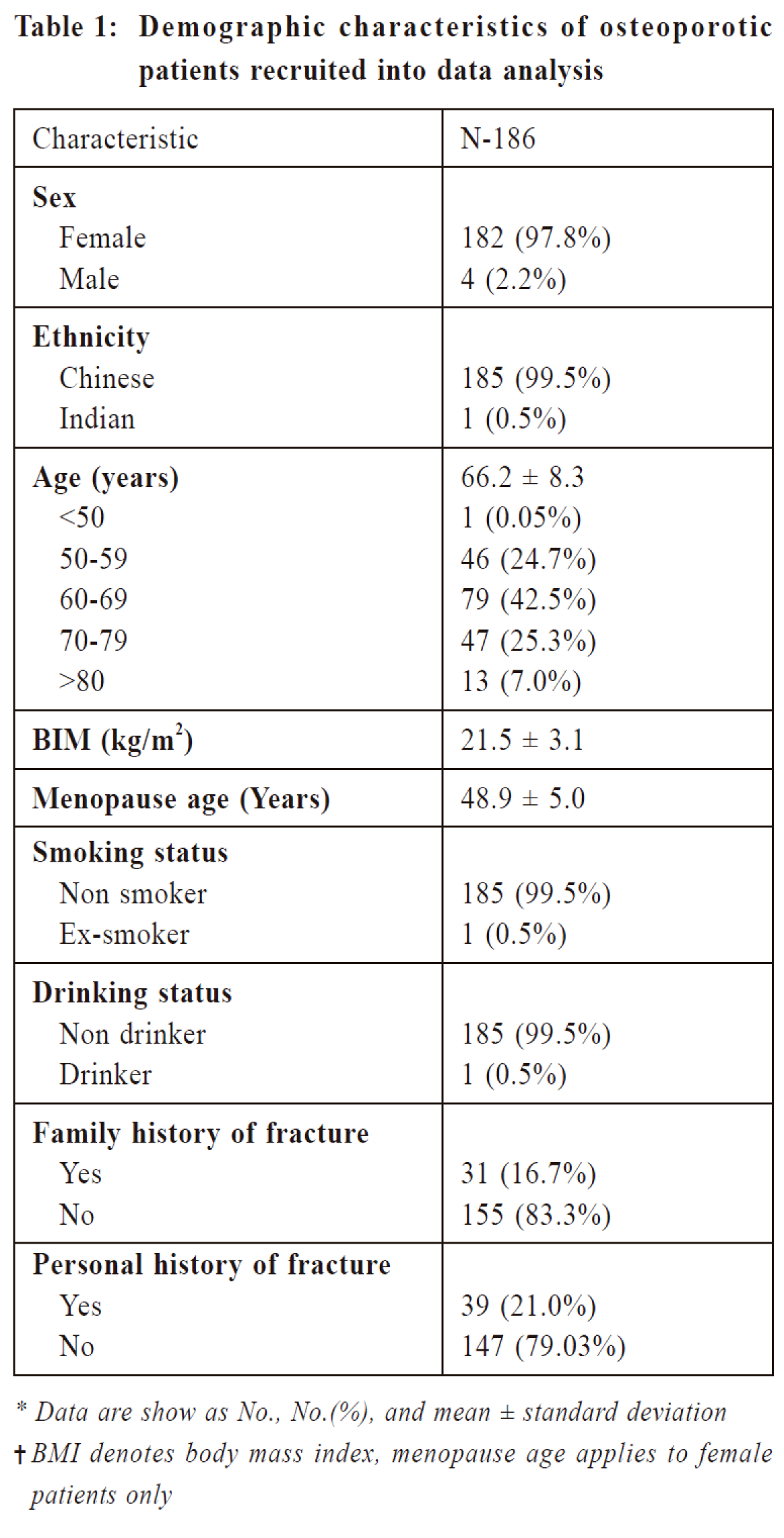
Among the 186 recruited patients, majority of them
are Chinese females, with a mean age 66.2 +/- 8.3 years
old. The demographics of the patients are summarised
in Table 1.
Furthermore, there were 39 patients who had a
personal history of fragility fracture (21.0%). Among
them, 15 suffered from spinal collapse (38.5%), 9
had history of distal radius fractures (23.1%), 4 had
proximal humerus fractures (10.2%), 3 suffered from
metatarsal fractures (7.7%), and 2 suffered from hip
fractures (5.1%).
Baseline blood test showed 12 out of 186 patients
had anaemia. Six patients were thalassemia carrier, 1
suffered from per rectal bleeding, and the remaining 5
had no identified cause for the anaemia. The baseline
liver, calcium, phosphate and thyroid hormone levels
were normal.
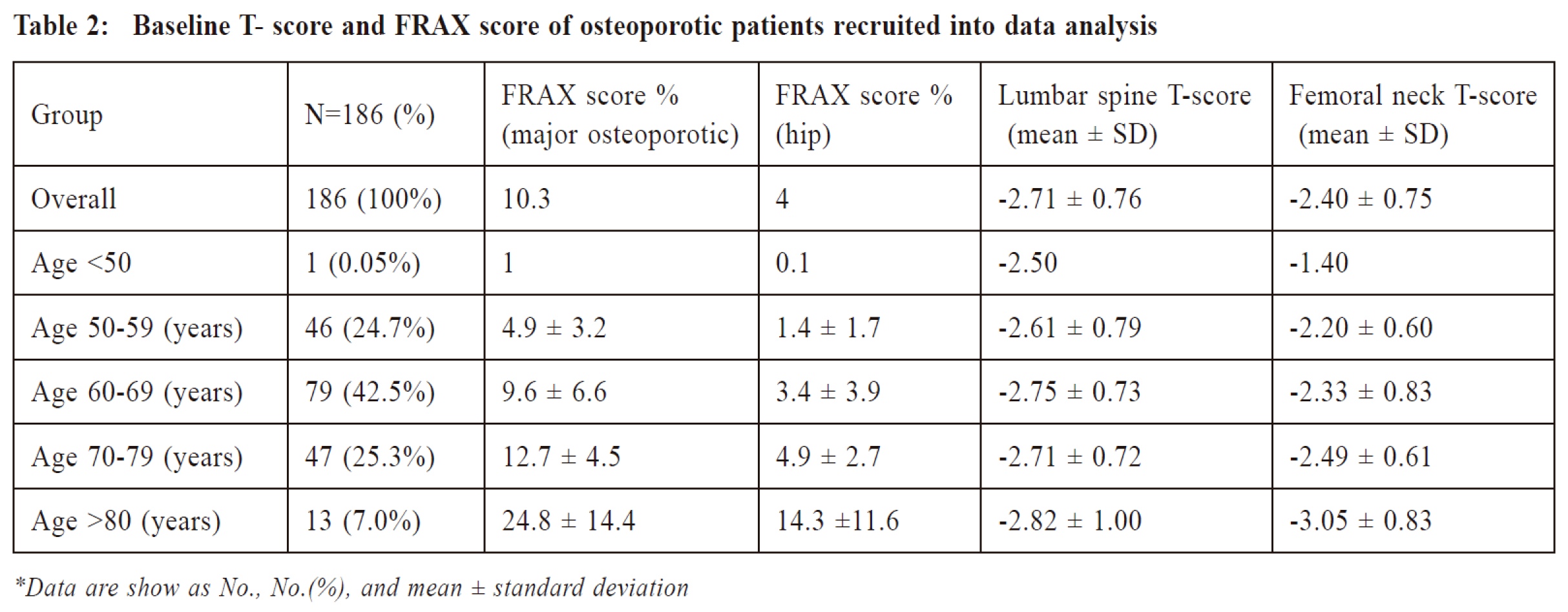
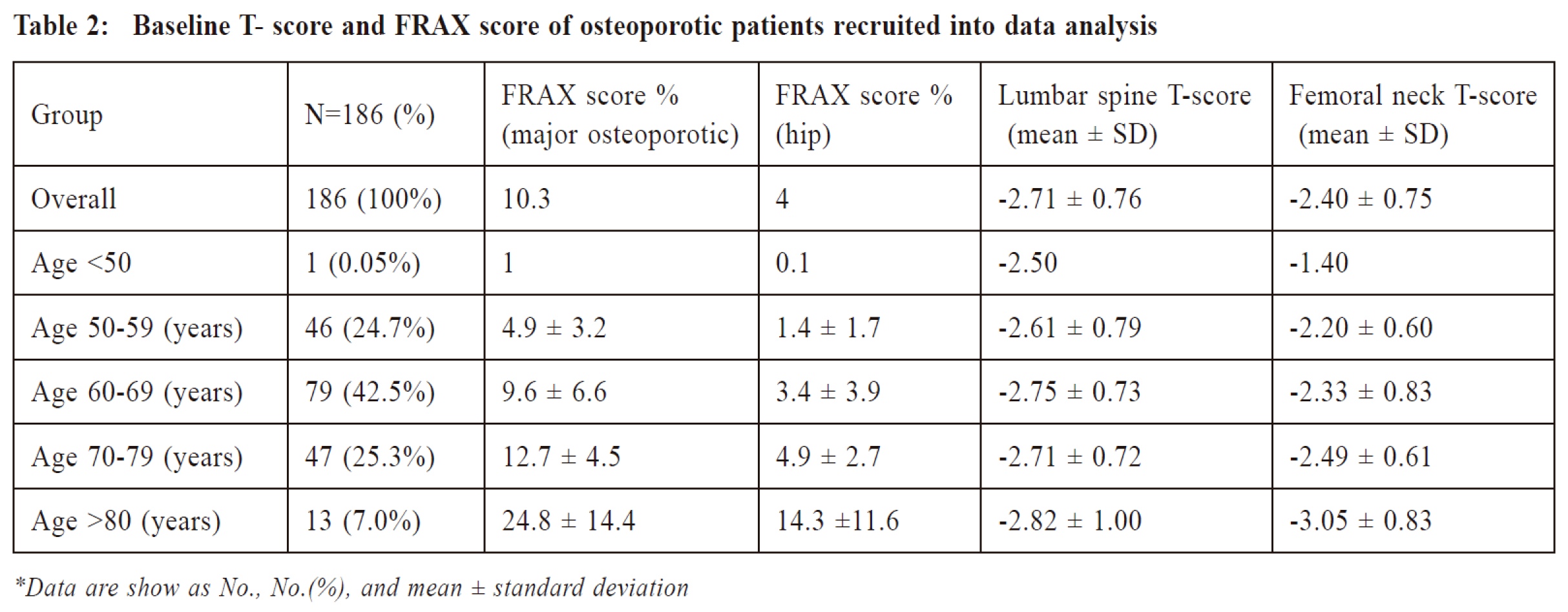
The mean baseline DEXA T-score of lumbar spine
and femoral neck were -2.71±0.76 and -2.40±0.75
respectively. While the FRAX score was 10.3±8.0%
for major osteoporotic fracture and 4.0±5.3% for hip
fracture. The baseline T-score and FRAX score for
different age groups of patients were summarised in
Table 2.
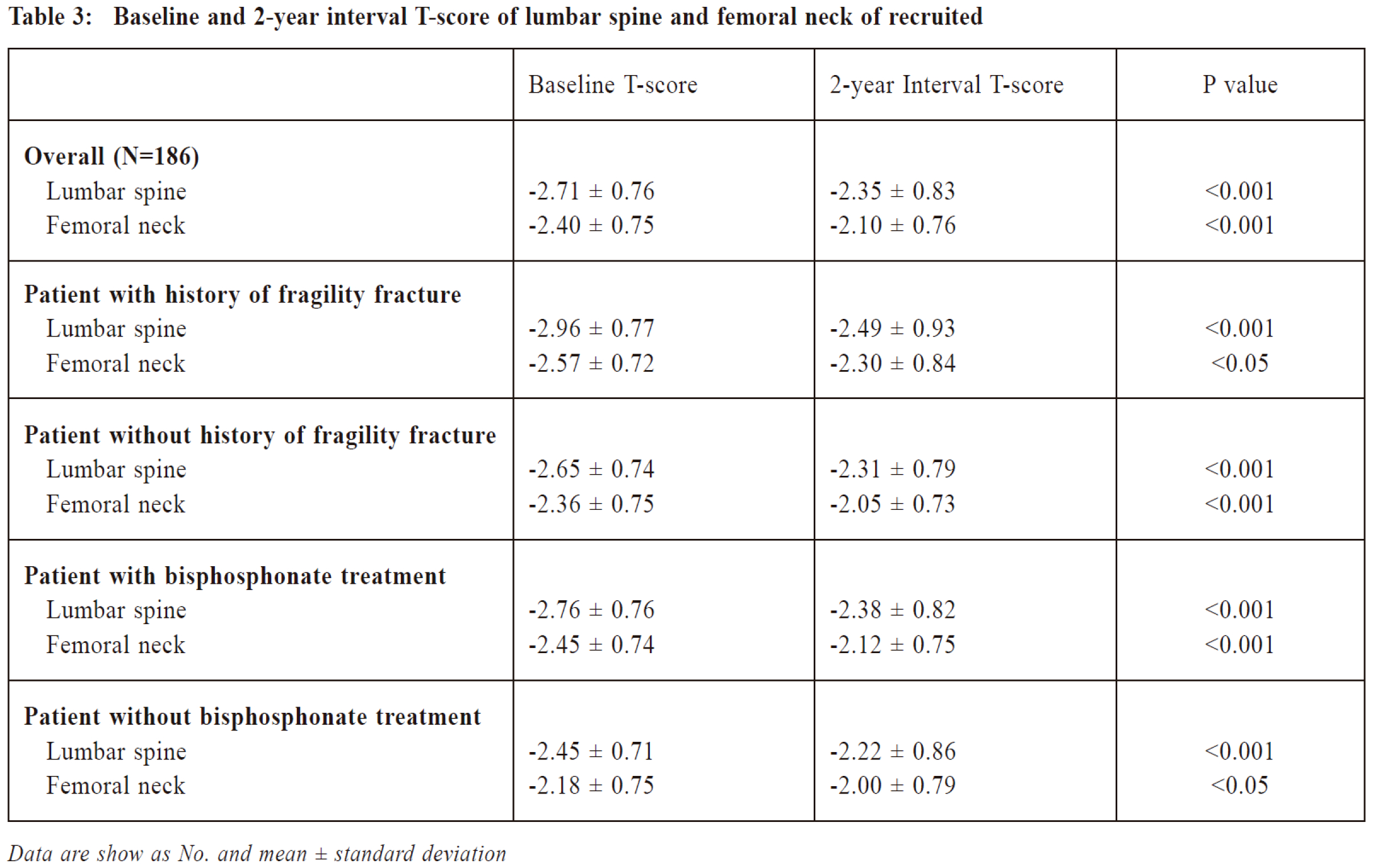
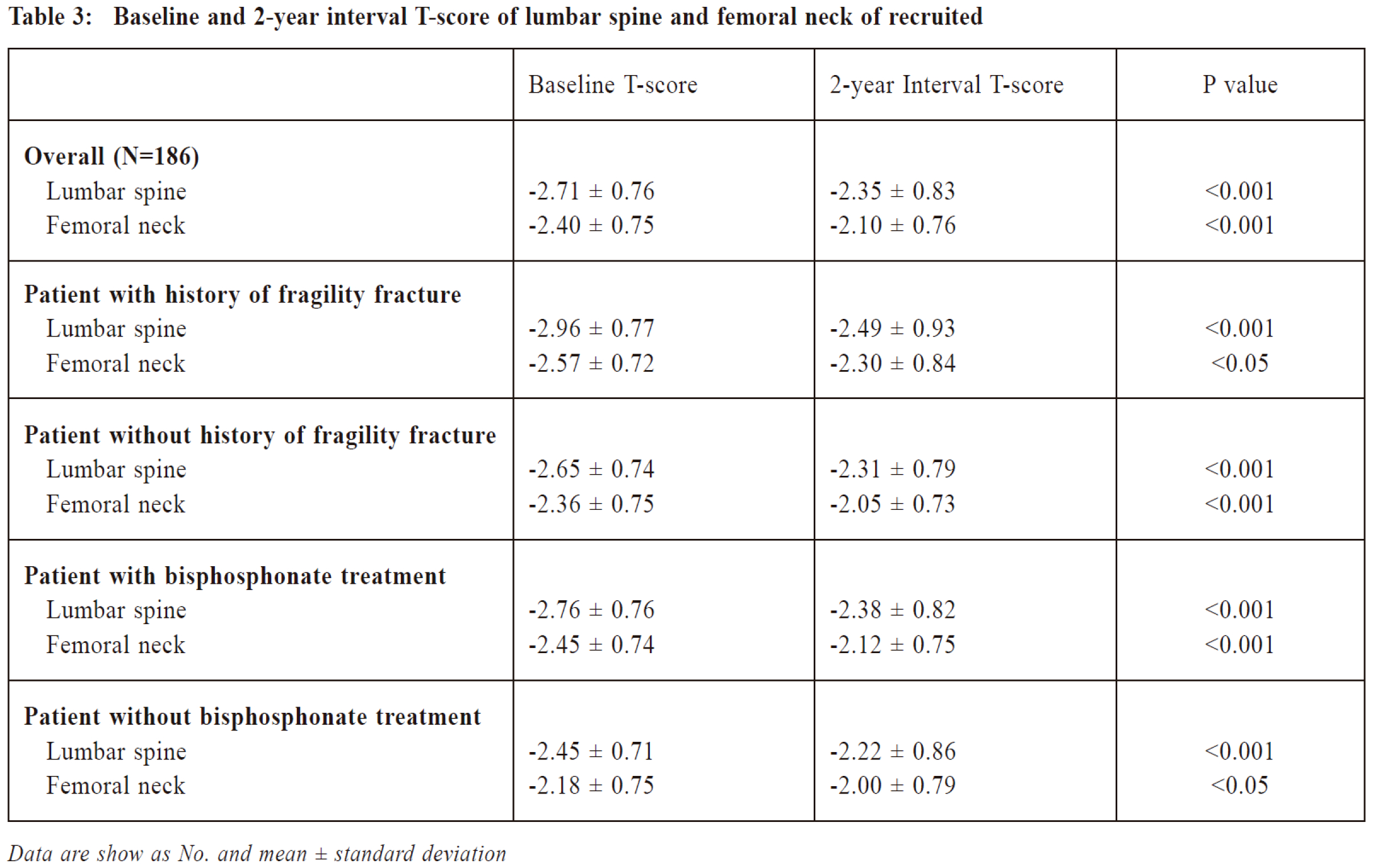
After 2 years of management via the MOC,
T-scores of recruited patients simproved from
-2.71±0.76 to -2.35±0.83 at lumbar spine, and from
-2.40±0.75 to -2.10±0.76 at femoral neck, which were
both statistically significant (P<0.001).
Subgroup analysis of patients with a history of
fragility fracture showed that the baseline T-scores
were lower at both the lumbar and femoral neck region
compared to those without any history of fragility
f racture, which were -2.96±0.77 and -2.57±0.72
respectively. Improvement i n T-scores o f both
lumbar (P<0.001) and femoral neck (P=0.0017) were
significant at 2-year follow up. For those without a
history of fragility fracture, improvement in T-score
of both lumbar and femoral neck were also observed (P<0.001).
Among the 186 patients, 153 of them
(82.7%) received osteoporosis drug treatment, namely
bisphosphonate via the MOC. While 33 of them (17.3%)
had not received drug treatment and were on life
style modifications. Subgroup analysis of those who
received pharmacological treatment showed significant
improvement in the T-scores of both lumbar and femoral
neck (P<0.001). While those who were on lifestyle
modifications without drug treatment also enjoyed
T-scores improvement at both lumbar spine (P<0.001) and femoral neck (P=0.025).
The 2-year interval T-score changes of patients
were summarised in Table 3.
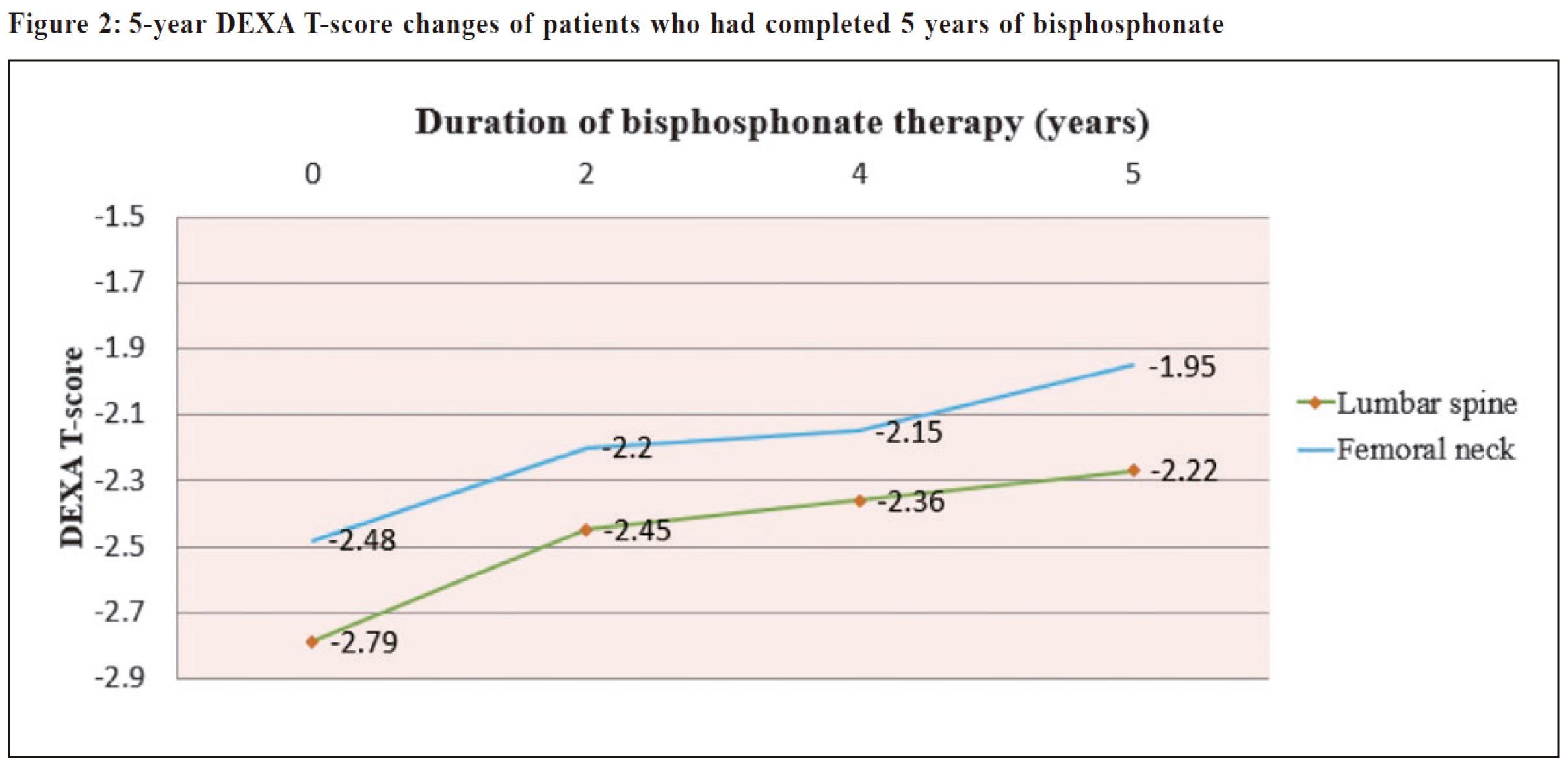
During the follow up period, 46 patients received
and completed 5 years of bisphosphonate therapy.
Progressive improvement in T-scores of both lumbar
and femoral neck were observed. The interval T-scores
of lumbar spine and femoral neck during the 5 years of
drug treatment were shown in Figure 2.
Regarding the secondary outcome, 1 out of the 186
osteoporotic patients suffered from a new osteoporotic
fracture within the 2-year follow-up period. The
incidence rate was 2.7 cases per 1000 person-years.
This patient suffered from a left hip fragility fracture
after two years of oral alendronate.
Discussion
To our knowledge, no similar team based
management model in primary care for osteoporotic
patients has been described. In this retrospective case
series analysis, we demonstrated that a dedicated team
led by primary care physicians could significantly
improve the bone mineral density of osteoporotic
patients. Our patient demographics are in line with that
of other studies on osteoporotic patients conducted in
china and Asia.17-19 The results of our study were very
promising in that the DEXA T-scores of the recruited
patients improved significantly in both lumbar and
femoral neck (P<0.001). Over 80% of osteoporotic
patients joining the MOC were started on osteoporosis
drug treatment which was significantly higher than the
treatment rate of previous studies.20 For patients with
pharmacological treatment, predominately treated with
alendronate, their 2-year interval T-score improved
0.38SD (from -2.76 to -2.38) at lumbar spine and 0.33
SD (from -2.45 to -2.12) at femoral neck, which were
comparable with other published clinical studies.21-23
Furthermore, subgroup analysis of patients who
were not on drug treatment also showed significant
improvement in T-scores of both lumbar and femoral
neck. This suggests that the T-score changes and BMD
improvements could not be solely explained by the
pharmacological effect of bisphosphonates but also by
the comprehensive service provided by the MOC.
The reasons why this MOC is highly effective in
improving BMD of patients is multi-factorial. First
of all, the MOC is a well-designed clinic tailored
to manage osteoporotic patients in the community.
Comprehensive, continual and coordinated care plan
could be delivered proficiently by the primary care
team in the MOC. Secondly, management plan offered
to each patient is very individualised in the MOC. Our
nurse would meet every patient during the individual
counselling session and give personalised advice. With
a longer consultation time, doctors can also formulate a
whole-person management plan with patients. Thirdly,
doctors who have attended the MOC are relatively
experienced family physicians and were equipped
with updated knowledge on osteoporosis management.
Previous research on doctors’ barriers on osteoporosis
treatment have revealed that a lack of knowledge on
osteoporosis drug treatment and specifically its adverse
effects may deter many doctors from treating the
disease.24-25 By centralising this group of osteoporotic
patients to the MOC with dedicated doctors and team
players, many of these obstacles of care could be
overcome, resulting in improvement in outcomes.
This study has several strengths. This is the
first study ever in the primary care of Hong Kong
to evaluate the effectiveness of a community based
osteoporosis clinic, in terms of DEXA T-score changes
in osteoporotic patients. Previous studies published
mainly focused on the detection and treatment rate of
osteoporosis6,20,26 or tried to explore factors preventing
the delivery of effective osteoporosis treatment to
osteoporotic patients.20,27 Our study is comprehensive
and impactful in terms of the outcome measurements.
It assessed not only the treatment rate of osteoporotic
patients but also the changes in their BMD and the
occurrence of fall during the follow up period, which
are important parameters directly influencing the
mortality and morbidity brought about by the disease.
Another strength of the study is that the clinical data
were precisely documented and complete, by using
preset templates and the CMS of HKHA. Doctors would
also document patients’ clinical condition, DEXA scan
results and blood investigation reports in consultation
notes of the CMS with a similar format. These measures
minimised the possibility of missing data or recall bias.
There are some limitations in this study. Firstly,
a large proportion of patients were excluded from the
final data analysis, which might result in selection
bias. The majority of the patients excluded had been
treated with bone resorptive agents before joining MOC
(N=160) or they had no interval DEXA scan within
the follow up period (N=102). Bone resorptive agents
could have lasting effects on residual BMD and fracture
prevention despite stopping the drug.28-29 A patient’s
DEXA T-score change after joining the MOC could be
related to previous treatment instead of the true effect
of the MOC, therefore were excluded. We believe this
treatment naive group could provide a fair reflection
of the effectiveness of the MOC. Secondly, this study
was carried out in a single public primary care clinic in
HA and therefore, the results of this study may not be
generalised to all primary care clinics in HK or in the
private setting. In addition, most patients followed up
in the MOC had to pay for their own drugs and DEXA
scans as they were not readily available from HKHA for
free, except for osteoporotic patients with a past history
of fragility fracture. Therefore, those who continued
to attend follow-up in the MOC could well represent a
group of patients who were more health conscious and
financially capable. Thirdly, since this is a retrospective
study without a control group, we should be cautious
in attributing all the positive outcome to the effect of
the MOC. However, available literature has reported
that age-related T-score of Chinese women who are
treatment naive deteriorates with age.30 Hence, despite
the lack of a control group, in view of the significant
improvements in the T-score of patients who joined the
MOC, especially in the non-pharmacological group, it
is justifiable to credit improved BMD of osteoporotic
patients to the effective management at the MOC.
Conclusion
With its growing incidence and increasingly
significant complications, osteoporosis represents a major
burden to healthcare. This study provided invaluable
evidence that a multidisciplinary osteoporosis clinic
run by dedicated family physicians in a public primary
care setting can effectively treat osteoporosis patients
with significant improvement in T-scores. We believe
that, based on the findings of this study, an integrated,
comprehensive and multi-disciplinary service model could
be developed in primary care to meet the service demand
in managing osteoporosis patients in the community.
Acknowledgement
We would like to express our sincere gratitude to
all medical staff and nursing staff for their professional
service at MOC of YMT FMSC.
References
-
Reginster JY. Burlet N. Osteoporosis: A still increasing prevalence. Bone
2006;38: S4-S9.
-
Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a worldwide
projection. Osteoporos Int. 1992 Nov;2(6):285-289.
-
Melton LJ, III, Chrischilles EA, Cooper C, et al. Perspective: How many
women have osteoporosis? J Bone Miner Res. 1992;7:1005–1010.
-
Peng Chen, Zhanzhan Li, and Yihe Hu. Prevalence of osteoporosis in China:
a meta-analysis and systematic review. BMC Public Health 16; 1039.
-
Ho SC, Lau EM, Woo J, et al. The prevalence of osteoporosis in the Hong
Kong Chinese female population. Maturitas. 1999 Aug 16;32(3):171-178.
-
Elliot-Gibson V, Bogoch ER, Jamal SA, et al. Practice patterns in the
diagnosis and treatment of osteoporosis after a fragility fracture: a systematic
review. Osteoporos Int. 2004;15:767–778.
-
The Royal Australian College of General Practitioners and Osteoporosis
Australia. Osteoporosis prevention, diagnosis and management in
postmenopausal women and men over 50 years of age. 2nd edn. East
Melbourne, Vic: RACGP, 2017.
-
FRAX, WHO fracture risk assessment tool. https://www.sheffield.ac.uk/FRAX/.
-
Freeman GK, Horder JP, Howie JG, et al. Evolving general practice consultation
in Britain: issues of length and context. BMJ. 2002 Apr 13; 324(7342):880-882.
-
Cosman F, de Beur SJ, LeBoff MS, et al. Clinician's Guide to Prevention
and Treatment of Osteoporosis. Osteoporos Int 2014; 25:2359.
-
Pauline M. Camacho, Steven M. Petak, Neil Binkley, et al. American
association of clinical endocrinologists and American college of Endocrinology clinical practice guidelines for the diagnosis and treatment
of postmenopausal osteoporosis 2016. Endocrine practice Vol 22 (suppl 4)
September 2016.
-
2013 ISCD Official Positions - Adult http://www.iscd.org/officialpositions/
2013-iscd-official-positions-adult.
-
Blake GM, Fogelman I. The role of DXA bone density scans in the diagnosis
and treatment of osteoporosis. Postgrad Med J. 2007;83:509–517.
-
World Health Organization (2007) Assessment of osteoporosis at the primary
health care level. Summary Report of a WHO Scientific Group. WHO, Geneva.
-
Liberman UA, Weiss SR, et al. Effect of oral alendronate on bone mineral
density and the incidence of fractures in postmenopausal osteoporosis. The
Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med.
1995 Nov 30;333(22):1437-1443.
-
Chan W. P., Liu J. F. & Chi W. L. Evaluation of bone mineral density of
the lumbar spine and proximal femur in population-based routine health
examinations of healthy Asians. Acta Radiol. 45, 59–64 (2004).
-
Suzanne C. Ho, Edith M.C. Lau, Jean Woo, et al. The prevalence of
osteoporosis in the Hong Kong Chinese female population. Maturitas. 1999
Aug 16;32(3):171-8.17.
-
Tian L1, Yang R, Wei L, et al. Prevalence of osteoporosis and related
lifestyle and metabolic factors of postmenopausal women and elderly men:
A cross-sectional study in Gansu province, Northwestern of China. Medicine
(Baltimore). 2017 Oct;96(43):e8294.
-
Hyun Koo Yoon, Young-Kyun Lee, and Yong-Chan Ha. Characteristics of
Patients Diagnosed with Osteoporosis in South Korea: Results from the
National Claim Registry. Bone Metab. 2017 Feb; 24(1): 59–63.
-
A.W. Kung, T. Fan, L. Xu, et al. Factors influencing diagnosis and treatment
of osteoporosis after a fragility fracture among postmenopausal women in
Asian countries: a retrospective study. BMC Womens Health 2013 Feb 14;13:7.
-
Rozkydal Z, Janicek P. The effect of alendronate in the treatment of
postmenopausal osteoporosis. Bratisl Lek Listy. 2003;104(10):309-313.
-
Rizzoli R, Greenspan SL, Bone G 3rd, et al. Two-year results of once-weekly
administration of alendronate 70 mg for the treatment of postmenopausal
osteoporosis. J Bone Miner Res. 2002 Nov;17(11):1988-1996.
-
Ho AY, Kung AW. Efficacy and tolerability of alendronate once weekly
in Asian postmenopausal osteoporotic women. Ann Pharmacother. 2005
Sep;39(9):1428-1433.
-
Simonelli C, Killeen K, Mehle S, et al. Barriers to osteoporosis identification
and treatment among primary care physicians and orthopaedic surgeons.
Mayo Clini Proc. 2002 Apr; 77(4): 334-338.
-
Mendis AS, Ganda K, Seibel MJ. Barriers to secondary fracture prevention
in primary care. Osteoporosis Int 2017 Oct;28(10):2913-2919.
-
Stephen H. Gehlbach, Maureen Fournier, Carol Bigelow, et al. Recognition
of Osteoporosis by Primary Care Physicians. Am J Public Health 2002
February; 92(2)271-273.
-
Ip TP, Lam CLK, Kung AWC. Awareness of osteoporosis among physicians
in China. Osteoporos Int 2004;15:329e34.
-
Black DM, Schwartz AV, Ensrud KE, et al. Effects of continuing or stopping
alendronate after 5 years of treatment: the Fracture Intervention Trial Longterm
Extension (FLEX): a randomised trial. JAMA 2006;296(24):2927.
-
Black DM, Delmas PD, Eastell R, et al. Once yearly zoledronic acid for
treatment of postmenopausal osteoporosis. NEJM 2007;356(18);1809.
-
Er-Yuan Liao, Xian-Ping Wu, Diao-Ge Deng, et al. Age-related bone mineral
density, accumulated bone loss rate and prevalence of osteoporosis at multiple
skeletal sites in Chinese women. Osteoporosis Int (2002) 13:669-676.
Pui-kwan Chan,
MBchB, FHKCFP, FRACGP, FHKAM (Family Medicine)
Resident Specialist,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority Hong Kong
Vincent WS Li,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Consultant,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority Hong Kong
Yim-chu Li,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Chief of Service and Consultant,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority Hong Kong
Catherine XR Chen,
MRCP(UK), PhD(Med, HKU), FRACGP, FHKAM (Family Medicine)
Consultant,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority, Hong Kong.
Correspondence to:
Dr. Pui-kwan Chan, Room 807, 8/F, S Block, Queen Elizabath Hospital,
Hong Kong SAR.
E-mail: cpk241@ha.org.hk
|