|
April 2001, Volume 23, No. 4
|
Update Articles
|
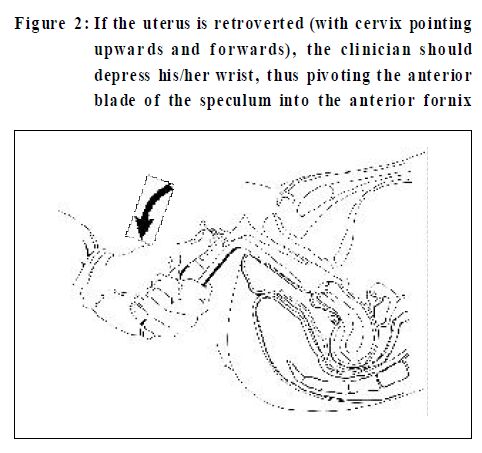
How to take a good Pap smear?S S T Lo 羅善清, SY S Fan 范瑩孫 HK Pract 2001;23:144 - 147 Summary In countries where population Pap smear screening programme is well implemented, the occurrence and mortality from carcinoma of cervix is substantially reduced. Screening programme can be effective only if women have adequate smears taken – a smear that accurately reflects the underlying pathology. In this article, the technique of taking a good Pap smear is described. 摘要 在全面推行宮頸塗片作為宮頸癌檢診的國家,宮 頸癌的發病率及死亡率都明顯下降。有效的塗片篩選 必須取樣準確。本文介紹取樣的方法。 Introduction To take a good cervical smear is relatively simple. It can and should be done by family physicians in their office. Many doctors had learnt this skill when they were medical students. If youwant torefresh your skill, a short attachment to a gynaecologist, family planning clinic, or one of your female colleagues who does Pap smears should be enough. While a gynaecological examining couch makes the examination easier for the doctor, many women find it embarrassing and uncomfortable, and a flat examination bench is just as good for this purpose. The appropriate equipment such as slides and spatula can be easily obtained from medical supplies company and the laboratory will provide the sampler and bottle of medium if you use liquid base cytology. The specula should be properly sterilised.Some gynaecologicalcouches have a built-inwarmingdrawer for keeping specula warm. Pelvic examination and Pap smear taking is a very intimate examination. Therefore, privacy must be ensured tominimise embarrassment of the woman. The examination room should be well screened and unnecessary exposure of the perineum should be avoided. Doctors should give a running commentary of what they are doing during the examination and this helps in alleviating anxiety during examination. If we take into consideration these simple but often forgotten steps, clients' satisfaction of the testing can be much improvedthus encouraging active participation in the screeningprogramme. Timing of Pap smears Pap smears should be taken after menses1 because blood stained smearsmaybe difficultto interpret. However, smears should be taken despite bleeding if local cervical lesion is seen or the woman has abnormal vaginal bleeding that needs investigation. If there are signs of infection or atrophy, they should be treated before Pap smear testing. However, when there mightbe problemwith compliance or return for testing, aPap smear should be done at the first visit. Insertion of the speculum Pap smear must be collected before bimanual examination. The doctor should put on gloves before handling instruments. The speculum should be well lubricated with warm distilled water before insertion. Lubricants such as creamor jelly shouldbe avoided. During insertion of the speculum, the blades of speculum should be closed and inserted at 45° to the vertical axis. The blades should be pointing backwards and downwards along the posteriorvaginalwallwith the tips pointingtowards therectal wall. The blades should then be opened gently to slip the blades intothe anteriorand posterior fornices, thus exposing the cervix adequately. If difficulty is experienced in locating the cervix, the best initial strategy is to elevate your hand thusdirecting the blades further into the vaginal apex (Figure 1). If this is not successful, the position and direction of the cervix can be ascertained by palpation. If the uterus is acutely retroverted, depressing thewrist may help to pivot the anteriorblade into the anterior fornix so that the cervix becomes better visualized (Figure 2).
Cervical cell samplers Several types of sampler are used: wooden Ayres spatula, plastic cervical broom and endocervical brush. The wooden spatula is relatively cheaper but it is too porous leading to trapping of cells in the sampler. Both the wooden and plastic samplers can be used in preparing conventional smears. Liquid-based cytology requires plastic device for sampling. In premenopausalwomenwith an adequate external os, only the spatula or the cervical broom is needed. In postmenopausalwomen and in premenopausalwomen who have previouscervical surgery, endocervical brushshould be used to ensure adequate sampling fromthe retractedsquamocolumnar junction. Sampling technique The sampling technique for conventional smears and liquid based cytologyis the same. Any large plug of mucus that obscures the external os should be removed gentlywith a dry cotton ball or swab prior to taking the smear. The spatula or cervical brush should be inserted into the cervical os (squamo-columnar junction) and rotated through 360° several times to collect enough cells. When using an endocervical brush, only¼ or ½ turn is needed. Overrotation will lead to trapping of cells deep in the bristles. Transfer of cells For conventional smears, cells from both sides of the sampling device should be transferred immediately onto a glass slide with a painting action. Try to paint an even and thin layer of cells on the slide. The slide should be fixed immediately to prevent airdrying of cells. Airdrying will cause degenerativechanges with loss of cellular features thus affecting the accuracy of diagnosis. Allow the slide to stand for 5 to7 minutesbefore storage to allow the fixative to reach all cells evenly. The slide will be transferred to the laboratory in a slide box. Most clinicians prefer using a commercially prepared alcohol aerosol spray for fixation. The ideal technique is to give two sprays 6 inches fromthe surface of the glass slide. Spraying closer than this can cause freezing artefact. Alternatively, each glass slide can be placed in a separate container with 95%alcohol. Many pathologists prefer this method of fixing. For liquid-based cytology, cells in the sampler are transferred into avial of preservative by swirling thesampler vigorously for 10 times. The vial is then transported to the laboratory. Inthe laboratory, the vial will be centrifuged to separate the cervical cells fromdebris,mucus and blood. A fraction of the cells will be transferred to a glass slide. Technical aspects of screening failure Screening failure as a result of technical problem can be due to sampling failure and transfer failure. A false negative smear may occur due to failure in sampling the abnormal area, failure in obtaining adequate cellular component for diagnosis or the lesion fails to exfoliate despiteadequate sampling. Therefore good smear taking technique is essential to ensure good quality of thePap smear. Doctors should ensure adequate exposure of the cervix, targeting the sampling towards the transformation zone and circumferential collection of adequate samples. Only about20%of the cellscollected can be transferred to the slide.2 Therefore false negative slidesmay be due to failure of transferring the abnormal cells onto the slide for diagnosis. Another source of error can be due to unsatisfactory preparation of the slide suchas bloody smear with traumatised cells, layering of cells, airdrying of slides and fixation artefact. All these technical problems can be minimised with the use of liquid-based cytology.1,2 Conclusion Doctors should be competent in taking good quality smears to optimisethechances of diagnosing anabnormality. Liquid-based cytology has helped to improve the quality and accuracy of the test3 and has reduced unsatisfactory smears rate but at a price. Key messages
S S T Lo, MBBS, MRCOG
Senior Doctor, S Y S Fan, MBBS, MRCOG, MPA, DCH Executive Director, The Family Planning Association of Hong Kong. Correspondence to : Dr S S T Lo, The Family Planning Association of Hong Kong, 9/F. , Southor n Centr e, 130 Hennessy Road, Wanchai, Hong Kong.
References
|
|