|
December 2001, Volume 23, No. 12
|
Original Article
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
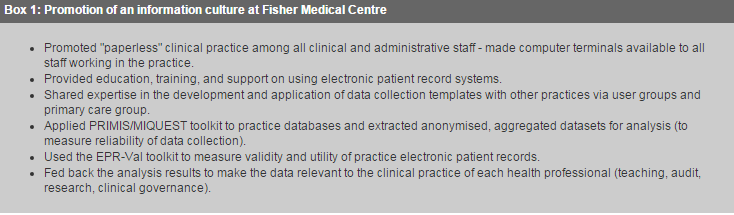
A survey of validity and utility of electronic patient records in a general practice*A Hassey, D Gerrett, A Wilson HK Pract 2001;23:540-547 Summary Objective: To develop methods of measuring the validity and utility of electronic patient records in general practice. Design: A survey of the main functional areas of a practice and use of independent criteria to measure the validity of the practice database. Setting: A fully computerised general practice in Skipton, north Yorkshire. Subjects: The records of all registered practice patients. Main outcome measures: Validity of the main functional areas of the practice clinical system. Measures of the completeness, accuracy, validity, and utility of the morbidity data for 15 clinical diagnoses using recognised diagnostic standards to confirm diagnoses and identify further cases. Development of a method and statistical toolkit to validate clinical databases in general practice. Results: The practice electronic patient records were valid, complete, and accurate for prescribed items (99.7%), consultations (98.1%), laboratory tests (100%), hospital episodes (100%), and childhood immunisations (97%). The morbidity data for 15 clinical diagnoses were complete (mean sensitivity=87%) and accurate (mean positive predictive value=96%). The presence of the Read codes for the 15 diagnoses was strongly indicative of the true presence of those conditions (mean likelihood ratio=3917). New interpretations of descriptive statistics are described that can be used to estimate both the number of true cases that are unrecorded and quantify the benefits of validating a clinical database for coded entries. Conclusion: This study has developed a method and toolkit for measuring the validity and utility of general practice electronic patient records. Introduction The NHS and its workforce are being made accountable for the services they provide through the emerging mechanisms of clinical governance.1,2 These mechanisms will depend crucially on the availability of high quality health information in clinical practice,3,4 and such data will need to be accessible through electronic patient record systems.5 These factors led us to consider the validity and utility of the electronic patient record system in a general practice and how these might be measured. The principal aim of this study was to measure whether the practice's electronic patient records were a true record of the health events associated with the patients of the practice. The prime function of the medical record is to support patient care.5 The general practice record is based on an individual and is a contemporaneous list of entries about that person's health. Record entries in computerised general practice systems generally consist of a mixture of text and Read codes. Together these form the narrative structure and content of the electronic patient record. Measures of validity tell us whether an item measures what it is supposed to that is, whether a measurement is true.6 An example would be to test whether the presence of the Read code for diabetes in the database truly means that the patient has diabetes. Reliability refers primarily to the consistency or reproducibility of the data or test. The degree of reliability of the measures applied to the data will set limits on the degree of validity that is possible. Reliability is usually measured by the degrees of correlation between measures of data. Reliability and validity must both be in place to enable useful comparisons of sets of data to take place. For the purpose of this study we extended Neal etal's definition of record validity: "Medical records, whether paper or electronic, record health events. Records are valid when all those events that constitute a medical record are correctly recorded and all the entries in the record truly signify an event".7 Attempts to validate electronic patient record systems have usually involved validating the database against either a paper record or patient survey.8-13 Sensitivity and positive predictive value have been used as measures of completeness and accuracy of recording respectively.8-10 In Britain the primary care information services (PRIMIS) project was designed to help primary care organisations improve patient care through the effective use of their clinical computer systems.14 PRIMIS uses a methodology based on standard MIQUEST queries15 to interrogate practice clinical databases. These queries include validation checks, but they are primarily useful as a tool for assuring the reliability of health data and facilitating the analysis of aggregated anonymised datasets. We could find no other published accounts of attempts to validate electronic patient records based solely on the contents of the clinical database. Subjects and methods The study practice, Fisher Medical Centre, is based in Skipton, serving 13500 patients in the Yorkshire Dales. The practice has used the EMIS clinical system since 1990 and has been "paperless" since 1994. Patient data are entered by general practitioners, practice nurses, administrative staff, and attached community nurses. All patient events and contacts with the practice should be recorded by direct entry, electronic scanning of letters, or clinical messaging from local NHS providers (such as laboratory reports). Much time and effort have been spent fostering an "information culture" in the practice over the past six years (see Box 1).16 The practice clinical database should be valid, complete, and accurate since 1994.
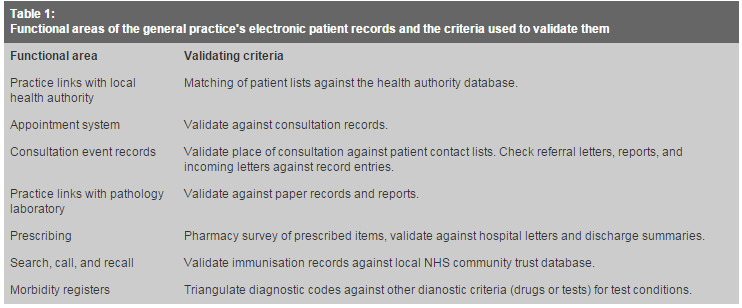
We performed our study (which was approved by the local ethics committee) in two stages. The first stage was to build confidence in the validity of the clinical database across the main functional areas of the electronic patient records (Table 1). We sampled practice activity retrospectively, so staff were not alerted to the study beforehand and had no chance to change their recording behaviour. We sampled the details of all patient events and contacts with the practice over a typically busy week. We selected the study week at random but excluded weeks containing a bank holiday. We validated the practice database for registrations and items of service against the local health authority's database over three months. We also measured the completeness and accuracy of practice prescribing with a one month retrospective survey of the town's busiest local pharmacy. All prescriptions are issued via the practice computer except those issued when working for the general practice cooperative or on house calls. We surveyed the pharmacy to measure the number of practice prescriptions dispensed by them and checked all handwritten prescriptions against the practice electronic patient records. Finally, we compared the separate record systems used by the practice's health visitors for preschool children with the practice system to identify and check the vaccination status of all 3 years old children in 1999.
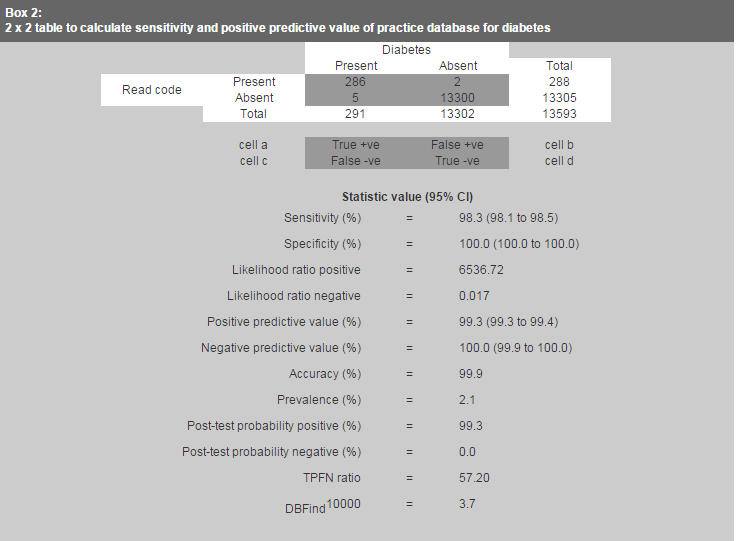
In the second stage of our study we measured the validity of the clinical entries in the practice's electronic patient records. The principal innovation in our study was to consider the Read codes in the records as tests for the true presence or absence of the associated conditions in the database. The method was based on using Read coded entries over the previous five years (or previous year for asthma and ischaemic heart disease) to validate available criteria in the electronic records for 15 clinical diagnoses (for details, see extra information on the BMJ's website). These criteria would act as the standard for each diagnosis. We developed search strategies for these conditions and tested them against a standard PRIMIS toolkit.14 We chose the 15 diagnoses on the basis that they represented important causes of morbidity across the spectrum of chapter headings in ICD-9 (international classification of diseases, ninth revision), that they could be validated against other criteria in the patient record (drug treatment or diagnostic test), and that comparative data were available from other published studies. Statistical analysis We used standard statistical tests to compare the practice database with the validating criteria and other data sources such as the Morbidity Statistics from General Practice: Fourth National Study.17 We measured the completeness and accuracy of the electronic patient records in terms of sensitivity and positive predictive value respectively. These statistics can be calculated from a simple 2?2 table and can be applied to any "test" as a measure of its usefulness.18,19 The figure in Box 2 shows a worked example for diabetes.
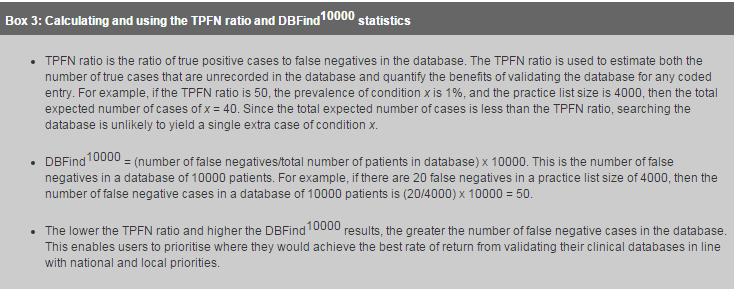
The power of a test can be understood in terms of its ability to change the prior (pre-test) probability that a patient does or does not have the test condition.20,21 The positive predictive value gives the power of a test to change the probability that the patient has the test condition. The likelihood ratio for a positive test is the odds that the test will be positive in a patient with the condition compared with a patient without the condition. The pre-test probability for any test condition is the prevalence of that condition in the community. Likelihood ratios are an accepted method of "testing tests".22,23 In this study they represent a quantifiable measure of the validity of the Read coded entry to predict the true presence or absence of the associated condition. We checked valid data against recognised diagnostic standards for each condition to confirm existing diagnoses and identify potential further cases. The difference between the number of conditions existing in the database and the total number identified was made comparable through development of two new descriptive statistics, the TPFN ratio and the DBFind10000 (See Box 3 for details). We developed a toolkit in Excel (EPR-Val) to calculate the full range of statistics (including the TPFN ratio and DBFind10000) from the test data.
Results Validity of the main functional areas of the electronic patient records The practice list and all claims payments were fully reconciled with the health authority over three months in 1999. These payments are an important check on validity because they include procedures that can be carried out only on patients of the appropriate age and sex. During the study week, we checked all appointments and visits with practice clinicians against the database to confirm that every appointment had a consultation entry: 98.1% of 1029 consultations were recorded in the clinical records. Of the 20 not recorded, 12 were "Did not attend", and eight consultations were missed. During the study week, the practice received 202 hospital letters, 358 pathology reports, and 12 contact sheets from the general practice cooperative and made 44 referrals. There were several minor transcription errors, but clinical details were correctly recorded in every case. When we surveyed Skipton's busiest pharmacy we found a total of 639 practice prescriptions were dispensed by them over one month, 629 computer generated and 10 handwritten prescriptions. Of the handwritten ones, eight were properly recorded in the computer clinical record and two were missed. Overall 99.7% of prescriptions tracked were recorded by the electronic patient record during that month. When we checked the vaccination status of all 3 year old children in 1999 we produced a list of 144 children. The records matched with the separate record systems used by the practice's health visitors in 140 (97%) cases, the remaining four children had just registered with the practice and were unknown to the health visitors. Validity of clinical entries in electronic patient records We ran a series of standard MIQUEST validation queries, which included checks on codes that are sex specific. Two men were recorded as having had cervical smears, but there were no other unreconciled procedural coding errors. This gave us the confidence in our coding to populate the 2?2 contingency tables (details available on the BMJ's website) and calculate the statistics for each of the 15 diagnoses (Table 2). These results show that the practice database was valid, complete, and accurate. The results for obesity are an exception and reflect a coding practice of recording body mass index rather than the diagnosis of obesity. The likelihood ratios indicated that the presence of the Read codes for the 15 conditions indicated a true diagnosis in 96% of cases. The absence of the Read code indicated the true absence of those conditions in 99.5% of cases (Table 2).
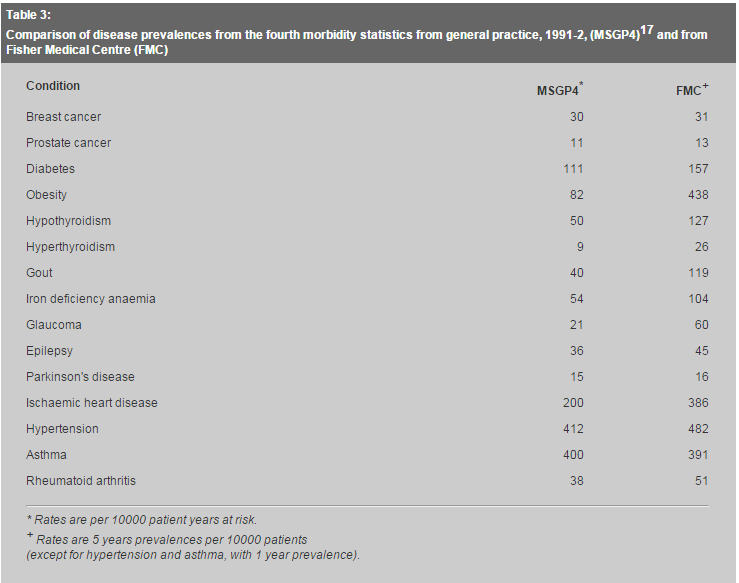
The TPFN ratios and DBFind10000 results for asthma, iron deficiency anaemia, hypothyroidism, and ischaemic heart disease indicate high priority areas for the practice to identify previously undiagnosed true cases of these conditions in the database. Discussion The first stage of this study established a method for validating a general practice electronic patient record system. The study period covered just one-geek, and other random checks might be important for particularly busy times. However, we are confident that our sample was representative of typical practice activity. The practice database was generally valid for prescribed items, consultations, laboratory tests, hospital episodes, and childhood immunisations. The results compare favourably with those of other published studies.9,13,17 The second stage of the study measured the validity and utility of the clinical database for 15 diagnoses. The morbidity data associated with these conditions were highly valid and reliable. The prevalences of these diagnoses in this study were generally higher than those reported in the Morbidity Statistics from General Practice: Fourth National Study17 (see Table 3).
Our study assessed the power of a diagnostic code (Read code) to alter the probability that a patient actually had a test diagnosis through the calculation of a range of statistics. Sensitivity, positive predictive value, and likelihood ratio are useful in combination to assess the overall validity of clinical diagnostic coding in an electronic patient record because of their different strengths and weaknesses.18-20 We suggest that overall validity of electronic patient records should be assessed with these measures in combination. Health workers could use the method and toolkit described here to quantify the validity of their electronic patient record systems. The derived statistics TPFN ratio and DBFind10000 facilitate the estimation of the true prevalence of medical conditions in the database, based on setting clinical criteria, and help quantify the benefits of validating the database for each condition. Users could then prioritise where they would achieve the best rate of return from developing and validating their clinical systems in line with national and local priorities. The statistical tests applied in this study are sensitive enough to enable health professionals to measure the degree of confidence they can have in clinical coding at the level of a single practice. A validation toolkit (EPR-Val) was developed as part of the research project. This provides a full range of statistical tests (including the TPFN ratio and DBFind10000), and we have made it freely available on the BMJ's website. In conclusion, we have developed a new approach to the validation of clinical databases in general practice. We have validated a general practice electronic patient record system and developed a standard method and toolkit for quantifying the validity and utility of data in clinical databases. The results of this study are relevant to all those involved in patient care and performance management in the "New NHS". We thank Dr James Newell for providing independent statistical advice on the methods developed and applied in this paper, Dr Richard Neal for his support through the Yorkshire Research Network (YReN) and for his comments on the draft manuscript, Dr Nick Booth for his advise, support, and encouragement; and Ms Sheila Teasdale for her advice and encouragement. Contributors: All three authors conceived and planned the study. AH and DG developed the toolkit and performed the analysis. AH was the main author of the paper, with revisions from AW and DG. DG will act as guarantor for the paper. In addition, Dr David Pearson helped in the planning of this study and provided constructive criticism and comments on the draft manuscript and Dr John Williams helped in checking and correcting the EPR-Val toolkit. Funding: The Fisher Medical Centre is a research practice funded by Northern and Yorkshire Region of the NHS Executive.
A Hassey,, General Practitioner, Fisher Medical Centre.
D Gerrett,, Senior Research Fellow, Research School of Medicine, University of Leeds. Correspondence to: Dr A Hassey, , Fisher Medical Centre, Millfields, Skipton BD23 IEU, United Kingdom. References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||