Essential traditional Chinese medicine: Western scientific medicine
perspective*
E C L Yu 余秋良
H K Pract 20 0 1;2 3 :2 0 -2 7
Summary
An attempt has been made to briefl y describe the
framework of Tradi tional Chinese Medicine and i ts original
intent and meaning. Thi s has been contr asted wi th the
demands of current scienti fic medicine while provi sions
to understand its concepts by an expanded pl atform have
b ee n i l l us t r a te d . T h e ph y si c al s i gn s, di ag n os ti c
techniques as well as the principles of Chinese Medicine,
when further defined and formal i sed can be an asset to
di agnosis and treatment in mainstream medicine.
摘要
本文描繪了傳統中醫學的框架,簡述了其實質和
涵意。並與現代西方醫學的要求相互對比,在拓展的
層面來解釋中醫學的概念。如果能夠將中醫學的臨床
病徵,診斷方法及治療原則更準確的界定和規範化,
則可以增加主流醫學在診斷治療的寶貴資產。
There is a wide gap between Traditional Chinese
Medicine (TCM) and Western Scientific Medicine
(WSM), even in conceptual framework,terminology, and
practical clinical methods. In an earlier article, why they
evolved differently was addressed by comparing the
differences of the two cultures as these shaped their own
medical worlds in concept formation, instrumentation,
knowledge acquisition methods, practice behaviour, and
evaluation standards.
1 All these wide gaps were the
results of the long history of separate development between Eastern and Western thoughts and philosophy. In
essence,WSM culture promoted science,its methodology,
and the use of scientific technology to identify and treat
diseases. On the other hand, the culture that embodied
TCM favoured a perfectionistic approach, viewed the
universe and body philosophically and developed
inductive tools and methodswith such principlesto guide
restoring the total balance of the body.
In this era, when TCM practice is coming out of its
veil and obscurity, workersin mainstream medicine may
like to know how the wa y that TCM rea ches its
therapeutic goals can be justified in current WSM
perspective. No easy job, and depending on the amount
of understanding and experience with TCM as well as
WSM,the gap unfilled by adequate work and efforts could
raisemuch difficulty for different individuals. This article
is an attempt to guide the initiated readers to view TCM
along a path the author experienced,so that hopefully they
will be able to see that medicine can be practised with
both TCM and WSM like resources, from left and right
pockets, each with their strengths and weaknesses.
A different way to practise medicine
TCM started in the days before science. While
current workers in medicine emphasise the need of a
scientific basis, TCM emphasis was based on another
world view the Chinese then treasured. The scholars of
China, even Confucius, prioritised the basis offered by
Yijing (易經), the Book of Cha nges. Simp ly, as
everything in the universe is changing,Yijing depicts a
mechanism to describe such patterns of changes. The
origin of such principles hasbeen attributed to Fu Xi (伏
羲), while metaphorical and mathematical methods to
evaluate its applications in estimating directions and
changes have been developed by later workers.
TCM developed in such an environment. In the days
of Shen Nong (神農), theDivine Farmer, agriculture was dominant, and people began to systematically document
plants which were toxic, and medicinal effects were
identified and classified under such framework. The
classic Huangdi Neijing (黃帝內經) using a dialogue
between Huangdi and QiBo, described naturalistic
observations of life and ways of living, and applied these
to man. Though not a mature practical clinical method,
it founded the roots of TCM: the integral perspective,
application of yin-yang and 5-phases principles in
pathogenesis, and a framework for diagnostic and
therapeutic methods. Debates during the wisdom boom
around the era of Warring States established the
philosophy and methodology of knowledge acquisition.
Later in the Eastern Han Dynasty, in the Discussion of
Cold-induced and Miscellaneous Diseases (傷寒雜病論),
Zhang Zhonging developed a systematic practical clinical
method which dominated the treatment of febrile illnesses
for centuries.
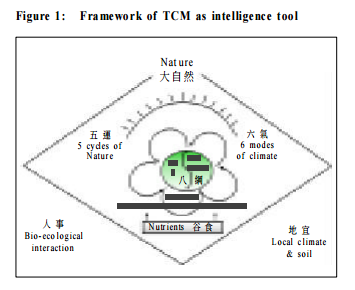
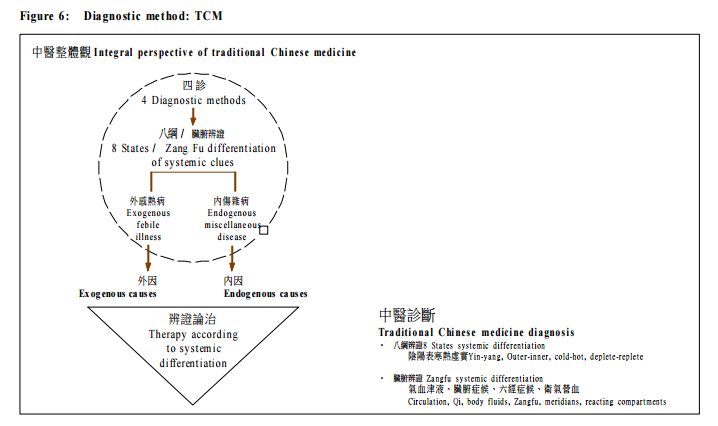
From these and later developments, TCM used its
basic framework as an evaluational tool (Figure 1).
Throughout the centuries, the framework allowed
accumulation of clinical observations. Its emphasis on
mechanism of changes probably led those early workers
to develop formats and intelligence instruments that
describe functional changes better. Indeed, it may be said
that TCM often is more useful than WSMto describe and
categorise functional problems in diseases.
The TCM framework
Huangdi Neijing described man and his functional
adaptation a nd reactions to the environment. It emphasised how health and longevity could be improved
when the body and mind harmonize with the ways of life
according to nature. Projecting from this, it explained
how observations of the functional reactions of living
things can be a way to observe man in his environment.
The TCM framework developed intelligence tools to
evaluate. In the framework, the body can be assessed by
the 8 states, using opposites: yin-yang, inner and outer,
deplete or replete, hot or cold (陰陽表裏寒熱虛實).
Furthermore, the pattern of interactions inside the body
is taken as similar to the universe and can be assessed in
relation to the zang-fu, blood circulation and qi (臟腑氣
血). Important though often under-emphasised, an
assessment of the harmony between the body and the
environment ismade, where the environment is evaluated
in terms of seasonal changes, climate and soil. This
framework (Figure 1) became the evaluational tool.
To describe the changes in the universe, the use of
characteristics and properties to depict changes had
become useful. Thus the universe was described by its
yin-yang properties, and there being so many elements
that may change, a simplified model with five elements
which portray the phases or their functions interacting
with each other in a balanced whole was used. It was
believed that man would function in that same pattern,
and the body needed to achieve that same balance inside
in order to achieve balance with the environment.
TCM continued to say more. For example, where
could such body framework, apart from balance, derive
its energy and momentum. This drove the search for the
body stem or core (本). Initially in Neijing, the zang heart
was taken as the driver of the body. This probably took
it as analogous to the heart-felt feelings that drive the
mind and body. The continued search took much
discussion and controversy. Finally in the Ming dynasty,
the body stem that subserved the basis of the body was
taken as coming from two zangs.
2 The zang spleen which
essentially means the absorptive and assimilation system
provides the energy as it constantly takes in. The zang
kidney, likened to the neuroendocrinal axis, gives the
body the born energy capital that supports its life.
The current demands from scientific medicine
So much for the TCM framework. The worldview
framed by science demands validity to any such reality
to be understood on a more solid basis. Scientific medicine has evolved far in the last few centuries and has
gone deeper into understanding of cellular biochemistry
and physiology, cellular pathology including cancer,
embryology and developmental science, and others. The
most dramatic development of WSM in the last half a
century has been supported by the vast and extensive
development ofscience and technology. Whatscience has
developed, medicine has used to its advantage. The hot
topic may have been laser technology then, or DNA
techniques now, or at another time another scientific
development. These have added on power to look into the
body with more and more specific details.
Such biomedical worldview has created wider and
wider gaps with the naturalistic observations of everyday
life, and even more so with the evaluational perspective
of TCM. It may be presumptuous to call TCM scientific.
However, this once important methodology can not be
wholly discounted by modern science. For thosewho rely
on nothing except the biomedical approach as scientific
medicine, much work would be needed to transform the
concepts and basis behind TCM into its frame.
Provision of understanding by other scientific developments in medicine
While the above went on, WSM developed into other
streams. Some of these developments might lend strength
to bridge the gap,particularly towardslooking at the body
as an integral unit. In social medicine, man is seen as
interactive with his environment including social,
poli tical, e conomica l and te chnical issues. The
understanding is that a better social environment helps
health. There are studies to show how the body and the
mind are linked to such social phenomena. For example,
it was found that a socially isolated person compared to
one well supported socially has a higher blood cortisol
level
3 analogous to a higher idling machine speed to cater
for life. An equivalent thinking may be used in TCM to
similarly view the core or state of body reacting to its
physical environment. The overexposure of glucocorticoids
and catecholamines meant for short term
mobilisation of energy, when extended over time, can
produce myopathy, fatigue.
4
In fact, the development of
psychological medicine
5
is also towards these directions.
Identification of the determinants of positive outcomes in
individuals at risk has been useful to uncover healthprotecting
factors, both constitutional or intrinsic
(biologically based) or extrinsic (social-contextual).
6
The body and environment in TCM
While WSM studied mostly the chemical and
biological environment around the body, the TCM
observations and emphasis were on the physical and
bio-ecological environment. It thus took a careful look
at the body reactions to heat and humidity and other
climatic changes. It even looked at hair changes and
skin changes with environment. Reviewing the use of
TCM framework as an intelligence instrument to assess
the body state and changes, it can be noted that the
assessment is on such body ties with the physical
environment. The idea is to assess how much a body
that is maladapted to climatic changes would have
poorer function similar to the cortisol example above.
While WSM used cortisol and other experiments to
document validity, TCM essentially tried to assess the
body core and used other experiential observations to
justify itself.
The scenario and clinical methods developed by
Zhang Zhonging is one such example. It derived its
heritage from the Neijing observation that after being
chilled by a very cold Winter, a person would have
febrile illness in Spring.
7 Using the then current
clinical methods of pathogenetic classification with 6
major body meridians and aided by the diagnostic
modality with assessing the 8 states, the illnesses could
be classified and treated accordingly. Examples of
treatment methods in TCM would be like: warm the
chilled, cool the hot, expel what comes in, etc. As long
as t he rig ht me di cin e w it h suc h c ou nte rac ti ve
properties could be tailored right, then treatment is
likely to be successful.
How such an idea, incomprehensible to the present
world, that a body chilled could develop months later
a feb rile illne ss now ca lled a viral syndro me or
in fect ion , c ould do mina ted TCM in th e p ast is
interesting. What seems like simple truth, it took
centuries before other TCM workers advocated that
there could be a new infliction apart from the winter
chill to cause a febrile illness in spring. Thus, it was
but not too long ago in Qi ng d ynast y, th at t his
observation finally matured and Ye Tianshi developed
the other important practical clinical method on febrile
illness, on Discussion on Febrile Illnesses (溫熱論),
de scr ibin g a mo del of dif fer ent bo dy laye rs or
reacting compartments to assess the body reactions
to infection.
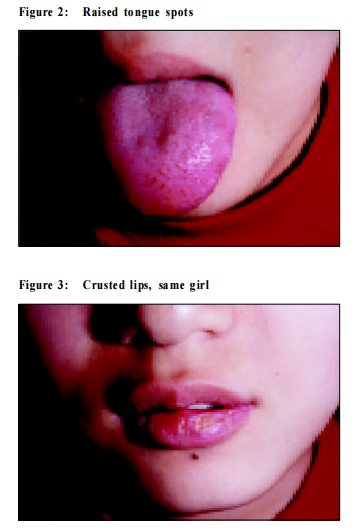
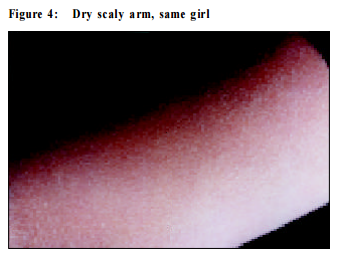
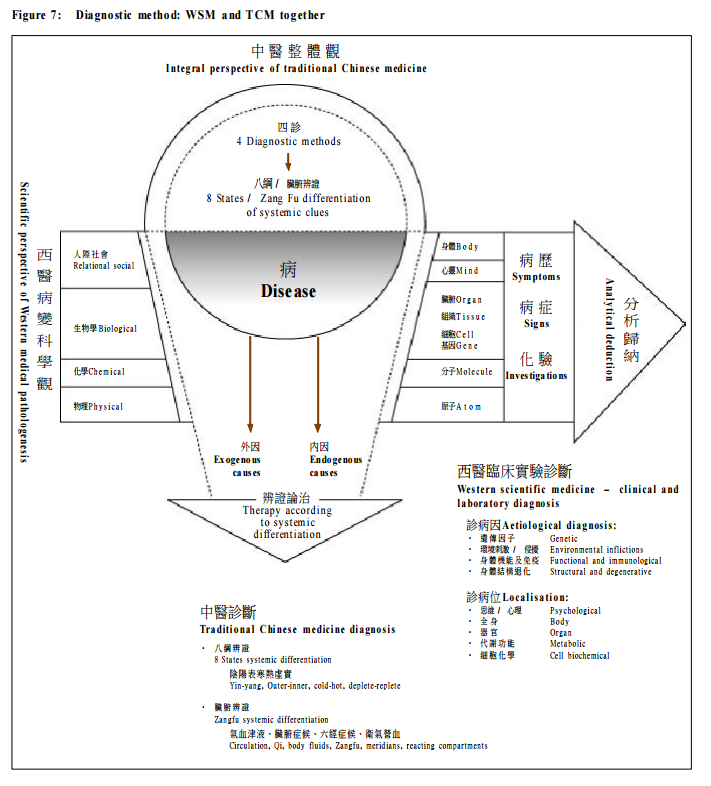
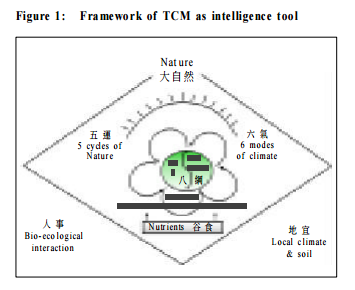
A note on signs of heat
Excess body heat can be assessed by raised tongue
spots (Figure 2). There are many signs (and symptoms)
of a hot state including dry furred tongue, crusted lips,
and dry scaly skin according to TCM diagnostics in the
same patient (Figures 3, 4). Though it may be argued
that the association may be pure coincidence, such
combination does occur to varying degrees in different
patients. Treatment of such patients with the TCM
category of drugs against hot states (cold herbs) alleviates
the signs (and symptoms) which could otherwise have
been there for a long time.
To take this further, many eczematous patients also
have such signs of hot states. Attention to this aspect
would alleviate their eczema. Combined with other signs
and managed accordingly, even psoriasis can be treated.
My other dissertation
8 may illustrate how treatment along
such principles could help these patients. Signs of hot
states in general can be defined, reproducibly identified and treated. It seems to be a physical sign of its own
right, not to be ignored, only the interpretation seems out
of bounds or without applications for WSM practice.
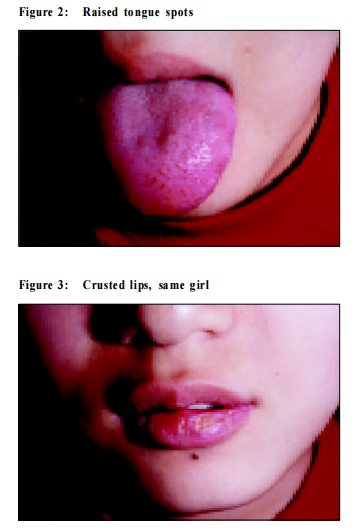
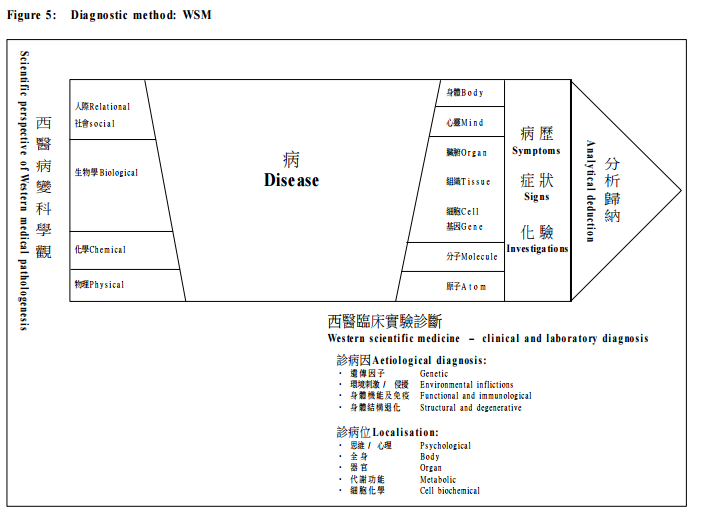
The diagnostic platform of TCM
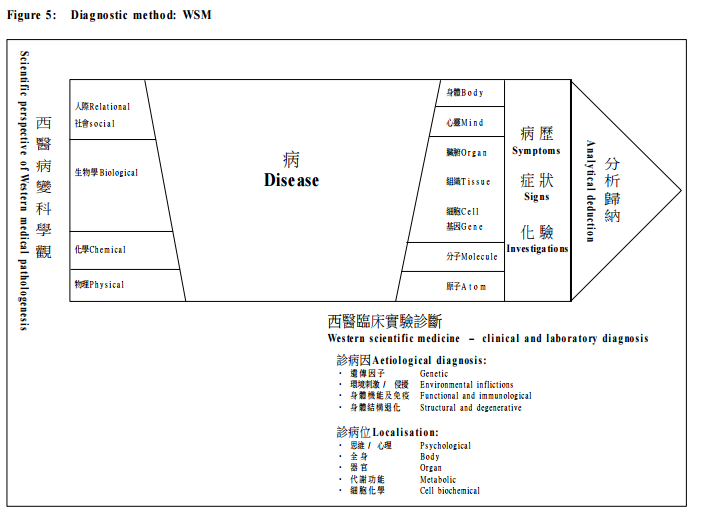
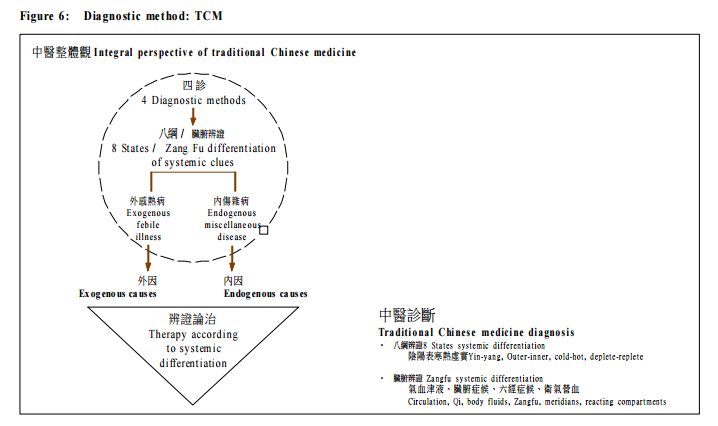
It should be understood that TCM assesses the core
integral unit of the body, and diseases could be the
maladaptations of such. With this framework, TCM
evaluates the whole integral body and its reactions to the
environment with the 8 states perspective and assessment
of the zangfu, blood circulation and qi. It would arrive
at an evaluation or diagnosis of the SystemicClues of the
body (証) (Figure 5), or the conglomerate evidence of
core functional changes.
9
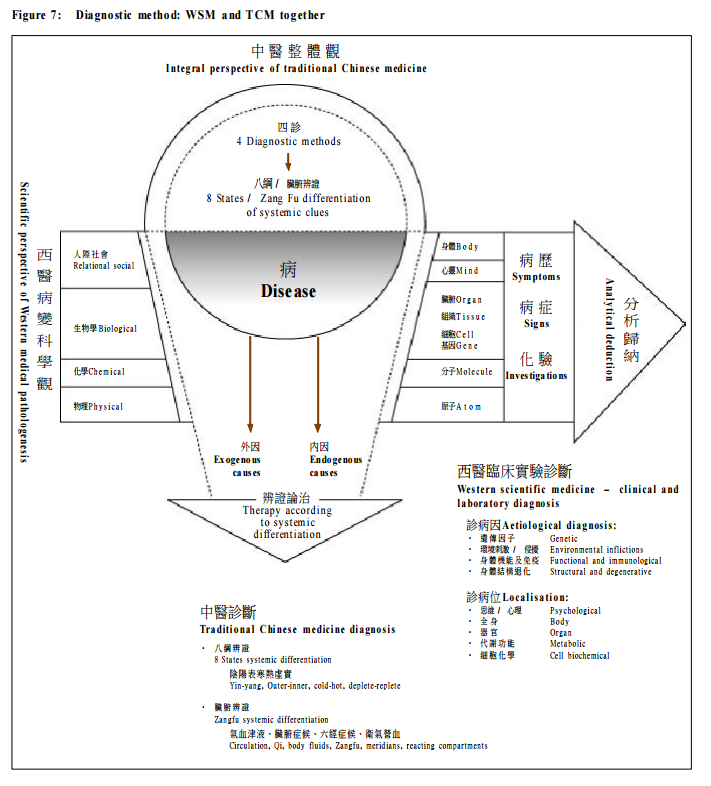
Taken together (Figure 7), the “disease” at the centre
overlaps issues that the two disciplines are assessing.
Along the linear arrow, WSM methods continue to add
on factorial analysis of the disease. On top, TCM also
assesses the deviations in reactions of the whole body as
a form of health disturbance, which may amount to
disease production.
A full diagnosis in academic medicine needs to
account for pathological diagnosis, symptomatic diagnosis, biomedical diagnosis, cellular diagnosis, and
similar definable issues. Now these are defined against
tangible issues. TCM could extend this to diagnose body
changes related to less tangible issues like weather. For
examp le, in WSM, aller gy to chemicals m ay be
recognised but not allergy to weather. TCMon the other
hand describes the abnormal reactions (analogous to allergy) to weather changes. TCM diagnosis adds to the
unfinished spectrum of assessing the body.
The importance to practise academic medicine
What we need with academic medicine is a firm
foundation to allow effective and well based decisions. The development of research techniques like double blind
studies helps to define effectiveness and what good
medicine is. The evolution to use outcome research
facilitates TCMdevelopment. Evidenced based medicine
is important to show what is necessarily valid to be useful.
Not all TCM is necessarily valid and useful, but
understanding of the limitations of WSM and the strength
of TCM allows further growth of mainstream medicine
using both. TCM by itself is a great resource. Scientific
efforts used to validate what has been noted to be useful
through the ages would be tiring, but careful selection
should lead the way to tremendous assets. Documentation
helps to lay ground for further development to best utilise
the resources. Drug research needs to be done on how
TCM herbs are useful to the current understanding of the
body and il lness includi ng, cel lular, organ, and
immunological changes. However, one should not be
blinded by the old habits of WSM and forget to assess
scientifically how these also affect the core state. How
to evaluate the scientific structure and effectiveness of
TCM and the difficulties to do so will be addressed in
later articles.
Final remark
It is helpful to understand TCM practice in its own
right and in consideration of its assets to WSM. For
example, along with the principle of Winter Storage, TCM
advocates that helping the asthmatic patient’s body
reserve in winter is better than at other times of the year.
I have tried using even simple WSM tonics according to
tailored counteractive properties assessed by 8 states to
help such patients in winter and found that some aged
patients suffering from asthmatic attacks throughout the
years weremuch relieved for a few years. There are other
examples where simple TCM principles helped and
guided WSMpractice. While strength and dominance of
WSM is established, TCM concepts and understanding
perfused into the mainstream will expand the domain of
medicine.
Acknowledgment:
I am grateful to Professor Chen Keji,Academician,
Chinese Academy of Science, and President, Chinese
Association of the Integration of Traditional and Western
Medicine, for his gracious help to review this article.
Key Message
- Western s cientific medicine (WSM) workers would
best be open to traditional Chines e medicine (TCM)
framework and methods as it takes a different
approach to observe man and life.
- WSM studies the chemical and biological while TCM
emphasis es the physical and eco-biological body
reactions to environment.
- Understanding TCM framework and diagnostic
me thod s c ould ex pand th e W SM a ss e ssme nt
repertoire to functional disorders.
- In the practice of academic medicine, WSM may be
taken as a resource for s cientific methodology, but
higher s cientific standards need to be achieved to
comprehensively evaluate TCM therapeutic methods.
|
References
- Yu E C L. Essential traditi onal Chi nes e medi cine, from differences to
scientific understanding. HK Pract 2000;22(4):185-188.
- 李中梓,明:醫宗必讀〈腎為先天之本,脾為後天之本論〉
- Sapolsky R, Al berts S, Altmann J. Hypercortisolism associated with social
subordinance orsocial isolation among wild baboons. Arch Gen Psychiatry
1997;54:1137.
- Sapolsky R. Hormones, t he stress response and indi vidual differences. In:
BeckerJ, Breedlove M, Crews D (eds). Behav Endocrinology 1991;287,
MIT Press.
- Millenson ER. Historical and psychological background of medical models.
Psychol Med, Eastl and Press, Seattle, 1995;11-10
- Ben-Yehuda N. Positive and negative deviance: more fuel for a controversy.
Deviant Behavior, 1990;11:221-243.
- 王冰校正,唐:黃帝內經素問卷三〈生氣通天論第三〉
- Yu ECL. Hong Kong Academy of Medicine
http://www.hkam.org.hk/temp/tcm.html
- Yu ECL. The basic clinical diagnostic framework synergized. Chin Med J
1998;111(5):460-465.
|