|
November 2002, Volume 24, No. 11
|
Original Article
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Elderly health centres - the first year experienceR S Y Lee 李兆妍, K S Ho 何健生, K L Chua 蔡金陵,K Y Lee 李啟源,N S C Wu 胡瑞枝,W M Chan 陳慧敏 HK Pract 2002;24:530-539 Summary Objective: To study the demographic, socioeconomic characteristics and health profile of elderly subjects enrolled in the Elderly Health Centres of the Department of Health. Design: One-year survey. Subjects: Elders enrolled in the twelve Elderly Health Centres in 1998-1999. Main outcome measures: Patients' characteristics and various categories of morbidity and health problems commonly encountered in elderly. Results: 25,105 elders were enrolled in the Elderly Health Centres, with 68.4 % female and 31.6% male. The ten commonest health problems among members are: musculoskeletal (52.8%), cataract (41.7%), hypertension (37.4%), hypercholesterolaemia (28.9%), hearing loss (19.1%), cardiovascular disease (16%), diabetes (14.1%), constipation (10.9%), urinary in continence (10.9%) and COAD (6%). Other health problems include: history of fall more than twice in the past 6 months (3%), polypharmacy (6.9%), cognitive impairment (5.7%) and probable depression (9.1%). Conclusion: Local data on health status of community dwelling elderly people are scanty. Our study provides useful information on the health profile of this age group.Keywords: Elderly, health assessment 摘要 目的: 統計及分析衛生署長者健康中心參與者的人口 結構,社會經濟特徵及健康狀況。 設計: 為期一年的統計。 對象: 1998年至1999年度十二個長者健康中心的參加者。 測量內容: 病人特徵,疾病類別及一般長者常見的健康問題。 結果: 共有25,105位長者參與長者健康評估,68.4%為女性,31.6%為男性,十個最普遍的健康問題為,肌肉骨骼問題(52.8%),白內障(41.7%),高血壓(37.4%),高膽固醇(28.9%),聽覺減退(19.1%),心臟血管疾病(16%),糖尿病(14.1%),便秘(10.9%),小便失禁(10.9%)及慢性阻塞性肺病(6%)。其他健康問題有,最近六個月內曾經跌倒兩次(3%),同服多種藥物(6.9%),認知失調(5.7%)及可能患有憂鬱症(9.1%)。 結論: 本地社區老人健康資料並不多,這個長者健康 評估報告及分析對本港長者健康問題提供多一些有用的數據。 主要詞彙: 老人,健康評估 Introduction With the growth of the elderly population in recent years in Hong Kong, the health status of our elders has become an increasing concern. The Department of Health has launched the new Elderly Health Services in July 1998. The strategic direction of this service is to identify the health risks of the individual community-dwelling elderly and to initiate intervention through primary care services with a multiple disciplinary team approach. There were twelve Elderly Health Centers in Hong Kong by June 1999 with 25,105 newly enrolled members. Methodology Elders aged 65 or over with a Hong Kong Identity Card were eligible for enrolment in one of the Elderly Health Centers. The enrolment was on a voluntary basis. An enrolment fee of HK$110 was charged with a waiving mechanism for those on social security. All members enrolled in the twelve centres were included in the study. All members enrolled were provided with a comprehensive annual health assessment, which consisted of:
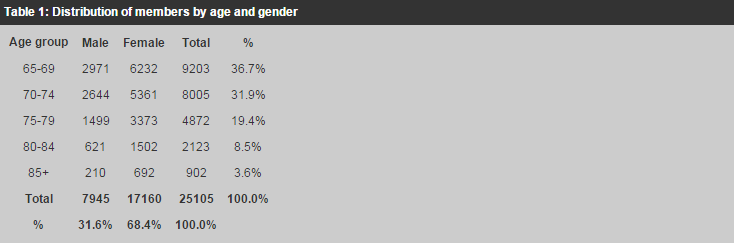
Results There were 25,105 elders enrolled in the twelve Elderly Health Centers from July 2, 1998 to June 30, 1999. Their findings were as follows: Demographic and socioeconomic characteristics Gender and age distribution
Among the 25,105 members enrolled from July 2, 98 to June 30, 99, there were 36.7%,
31.9%, 19.4%, 8.5% and 3.6% in the 65-69, 70-74, 75-79, 80-84 and
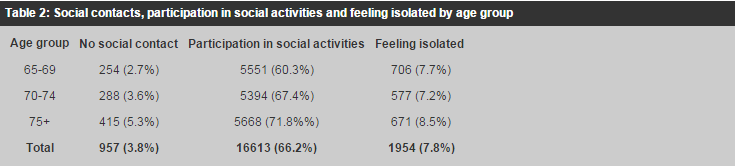
Housing The majority of our members lived in self-owned residences (45.4%) or public and aided housing (40.7%). Five percent lived in institutions. Education level Of our members, 45.3% were illiterate or received no formal education; 38.6%, 12.9% and 3.2% attained primary, secondary or post-secondary education respectively. Source of income As for income source, 62.8%, 18.8%, 9.1% and 4.2% of our members obtained their major source of income from relatives' contribution, CSSA, savings and salary respectively. Social contact Of our members, 55.1% (13,832) were cared for by at least one regular caregiver. 3.8% (957) of our members had no regular contact with any children, relatives, carers or friends and this increased with increasing age. (p<0.01) (Table 2) 66.2% of our members participated regularly in some form of social activity and this increased with increasing age. (p<0.01).
Women (71.9%) were more actively participating than men (53.9%) (p<0.01). Feelings
of isolation were not uncommon. 7.8% of our members subjectively felt isolated.
There was a general trend towards increasing feelings of isolation among our members
with increasing age (p<0.01), from 7.7% in the 65-69 age group to 11.3% in those
aged
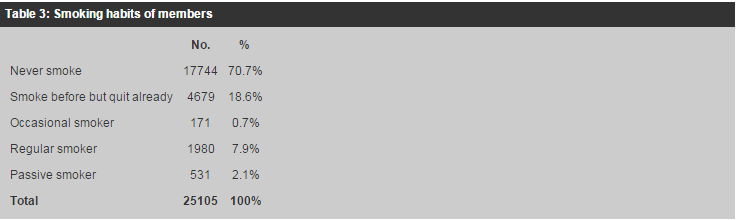
Health practice Smoking Smoking was a problem among our clients. 7.9% were current smokers, 18.6% had quit before joining our service, 70.7% had never smoked and 2.1% were passive smokers (Table 3). Among the 1980 smokers, 68.5% (1357) were male and 31.5% (623) were female. More males (17.1%) than females (3.6%) were regular smokers (p<0.01).
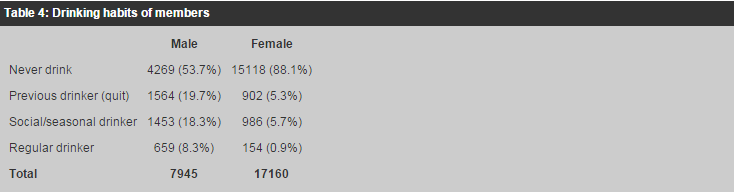
Drinking Drinking alcohol was uncommon among our members. Only 3.2% were regular drinkers, while 9.7% drank alcohol only socially. 8.3% of our male members and 0.9% of our female members were regular drinkers. (Table 4) Among the 813 regular drinkers in our centers, only 188 (0.7% of the total number of members) drank more than the recommended safety limit of 21 units per week for men or 14 units per week for women. Among these 188 excessive drinkers, 158 (84.0%) were male.
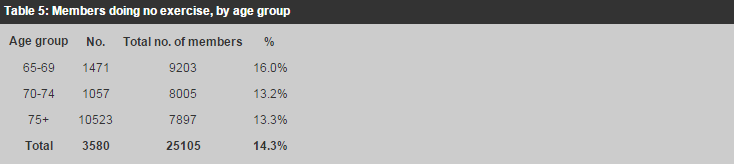
Exercise Exercise has been found to be a protective factor for disability6 and reduces the risk of functional decline and mortality in elderly subjects.7 85.7% of our members exercised regularly.
16.0% of the 65-69 age group, 13.2% of the 70-74 age group and 13.3% of
The most common exercise performed was stretching (37.2%), followed by traditional exercise like Tai-chi (19.5%), slow walking (16.7%) and aerobic exercises (9.8%).
Health status Prevalence of chronic diseases At enrolment, 87.4% of our members reported suffering from one or more chronic illnesses. The five most common health problems were musculoskeletal problems (52.8%), cataract (41.7%), hypertension (37.4%), hypercholesterolaemia (28.9%) and hearing loss (19.1%) (Table 6).
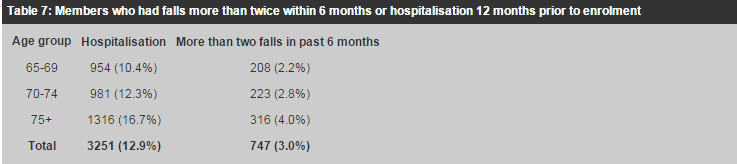
Fall Three percent of our members had suffered more than two falls in the 6 months prior to enrolment. This was found to increase with increasing age (p<0.01) (Table 7).
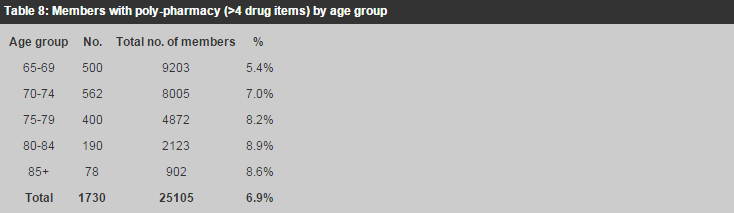
Medication Of our members, 53.9% had been taking medications regularly before enrolment in our Elderly Health Centers. 6.9% were taking more than 4 items. Polypharmacy increased with increasing age, from about 5.4% in the 65-69 age group to 8.9% in those aged 80 or over (p<0.01) (Table 8). Only 52.1% of the members reported that they understood the dosage and time schedule, and 45.1% reported good compliance before their enrolment.
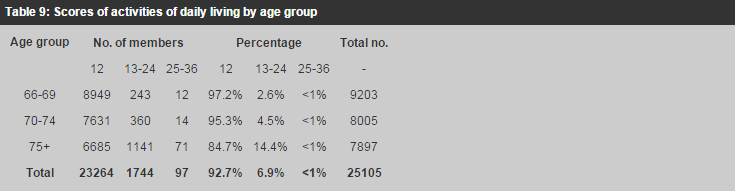
Activities of daily living (ADL) Many studies12-14 including a local study6 have found loss of independence and autonomy, and impaired ADL to be important predictors of mortality. Our questionnaire included 12 questions regarding ADL and Instrumental Activities of Daily Living (IADL). Members scored 1 for each question if they were fully independent, 2 if they needed assistance, or 3 if they were dependent in that area. They would, therefore, score 12 if they were fully independent, 13-24 if mildly dependent and 25-36 if severely dependent. A majority of our members were independent: 92.7% scored 12, 6.9% scored 13-24 and <1% scored 25-36. The impairment of ADL was found to increase with age (p<0.01) (Table 9).
Body mass index (BMI)
Height and weight were measured routinely in the health assessment. 12.3%, 50.0%,
32.1%, 5.5% of our clients had BMI <20, 20-24.9, 25-29.9 and
Abbreviated mental test (AMT) The AMT was used as a screening test for cognitive impairment. Members who scored less than eight were further assessed by the Chinese Mini-Mental State Examination and were also clinically assessed by the doctor. There were 4 missing data on the score. 5.7% of our members scored less than the cut off level at eight. This proportion increased with increasing age, from 2.8% in the 65-69 age group to 10.0% in those aged 75 or above (p<0.01) (Table 10). Geriatric depression scale (GDS) The Chinese version of GDS15 was used as a screening tool for elderly depression in our centres.23 Among our members 9.1% were found to score eight or above and required further assessment and management. Those screened positive increased with increasing age, from 8.0% in the 65-69 age group to 10.8% in the 75 or above age group (p<0.01). More women (10.3%) than men (6.6%) were screened positive (p<0.01) (Table 10).
Diseases/problems detected at health assessment Between July 2, 1998 and June 30, 1999, 25,105 elders were screened with 15,003 newly detected diseases and problems. The most common newly detected problem was hypercholesterolaemia (20.93%), followed by cataract (19.56%), hearing loss >40dB in either ear (8.96%), obesity BMI30 (5.64%), osteoarthritis (5.08%), cardiovascular disease (4.87%) and depression (3.21%) (Table 11). There were also 35 newly detected cancers. Only those with reply from hospitals confirming the diagnosis were entered and therefore the real incidence may be much higher. Among these 35 cases, there were 12 breast cancers, 9 cervical cancers, 7 colon cancers and 3 lung cancers.
Discussion Compared with the general elderly population, our clients were younger: 4.3% higher in the 70-74 age group and 4.4% lower in the 75 age group.1 The average female to male ratio was 2.2 compared to 1.2 in the general population.1 The proportion living in public and aided housing was lower than that of the general elderly population (52.7%).1 In the general population 43.7%, 40.2%, 11.7% and 4.4% attained no formal education, primary, secondary or post-secondary education respectively1 whereas our figures were 45.3%, 38.6%, 12.9%, 3.2% respectively. As for income source, 62.8% of our members obtained their major source of income from relatives' contributions and 18.8% from public assistance. A local study of the Hong Kong old-old population aged 70 and above2 showed that 37.1% and 44.4% obtained their major source of income from family and public assistance respectively. As for social contact, 55.1% of our members were cared for by at least one regular caregiver and 3% had no regular contact with any relatives, caregivers or friends. This was in contrast with the Ho & Woo study, in which more than 30% had social contact less than once a month with friends, neighbours or relatives. Our members were also more socially active than the elderly population in their study. 66.2% of our members participated in some form of social activities as compared with 24.2% and 13.1% of their population participating in community and religious activities respectively. The percentage of current smokers was 7.9% in our members and was lower than the Ho & Woo study, which reported 16.4% current smokers, and also low compared to other Southeast Asia or Western countries.3-5 The figure on regular drinking, 3.5%, was lower than that of the Ho & Woo study, which found 40% of men and 15% of women drinking 5 or more times per week. In our study, 85.7% of our members did some form of exercise regularly, as compared with 63.3% in the Ho & Woo study. The prevalence of hypertension and diabetes among our members was high compared with some other local studies (Table 12). In a study on elderly aged over 70 living in the community in Hong Kong (Chi & Boey 19948), 80.3% of the study population reported at least one chronic illness. The five most common were arthritis (65.7%), hypertension (25.1%), osteoporosis (12.8%), heart disease (11.2%) and diabetes (10.3%). In another survey of the elderly aged over 70 by Ho & Woo 1994,2 77.3% reported chronic diseases. The five most common were arthritis (35.9%), hypertension (31.6%), cardiac disease (18%), peptic ulcer (16.2%) and old fracture (15.1%); other reported diseases in this study were diabetes (10.3%), COAD (8.1%), cerebrovascular accident (8%), dementia (2%) and psychiatric disease (1.3%). In Ho & Woo's study, 33.8% of their population reported cataract of one or both eyes and 24.7% reported poor hearing. Compared with this study cerebrovascular accident, which was an important cause of disability, was considerably less common among our clients (3.3%).
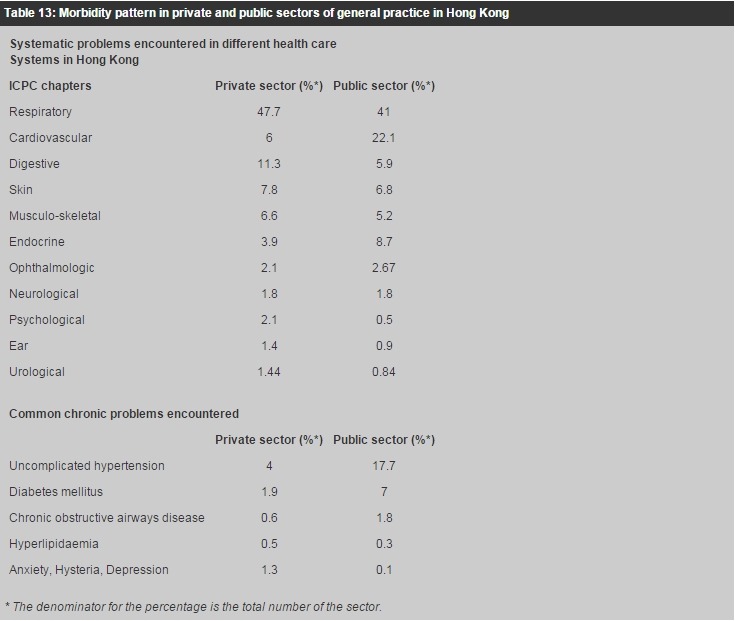
Compared with a survey of elderly Hawaiian Japanese and Australian men in Dubbo aged 70-81 years,10 our prevalence of hypertension was higher: 37.4% compared with 31% in Hawaiian Japanese and 29% in Australians; heart disease was 16%, higher than the 14% in Hawaiian Japanese but lower than the 29% in Australians; and cerebrovascular accident was lower (3.3%) compared to 6.4% in Hawaiian Japanese and 10% in Australians. Our diabetes figure of 14.1% resembled Hawaiian Japanese (13%) but was higher than the Australians (9%). Overall, the pattern was more similar to the Hawaiian Japanese. In another local study of elderly people,2 76.8%, 17.2% and 5.9% were found to have no impairment, mild and severe impairment of their ADL, respectively. This is in contrast with our members in whom 92.7%, 6.9%, and less than 1% had no impairment, mild and severe impairment of ADL, respectively. This could be explained by the fact that our target population was community-dwelling elders. The association between BMI and mortality is not very clear in the elderly population. Elderly subjects at the extremes of body mass index have been found to have an increased risk of disability and mortality.2,15-17 However, the correlation between higher BMI and excessive mortality is challenged by other authors18-20 In our study, 36.7% of participants had BMI less than 20 and 5.5% had BMI greater than or equal to 30. In the Ho & Woo study, 36.7% were underweight (BMI<20), 45.1% had BMI 20-24 and 18.3% had BMI 25. This was again due to different sampling methods. Elderly suicide is a serious problem in Hong Kong. One local study found that the suicide rate for the elderly was 4 to 5 times above the mean rate of the general population.22 Early detection of depression would help to reduce the suicide rate. In a local study24 of elderly Chinese aged 70 and over using a GDS cut-off point of 8, the overall prevalence of a positive GDS screening was 29.2% for men and 41.4% for women. In another survey in rural Chinese community25 for those aged 65 or above, 26% screened positive. In our study, only 9.1% were screened positive. As for AMT score, 5.7% of our members scored more than 8. This is lower than the 29.7% found in another local study which sampled those aged 70 or above on old age allowance.21 12.9% of our members had been admitted to hospital in the preceding 12 months. This figure was relatively low compared with other studies. In the Ho & Woo study,2 15.4% had been admitted once and 6.9% more than once, giving an overall figure of 22.3% admission in the past twelve months. In the U.K. 20% of men and 16% of women aged 75 years and over had been admitted in the preceding twelve-month period. In a USA study, 20% of Americans aged 65 and over were admitted to hospital over a one year period.11 Although the findings from our members might not represent the general population, they provided valuable information regarding the elderly population in our community where there was previously a general lack of data. Compared to the census data,1 more of our members were in the 70-74 age group, fewer were in the 75 or above age group, and the female to male ratio was higher. The proportion living in public and aided housing was lower than the general elderly population.1 Education attainment and source of income was comparable. They were socially more active with a general trend towards increasing feelings of isolation with increasing age. They had healthier lifestyles, they smoked and drank less, and they exercised more. They scored better on ADL, AMT and GDS screening tests. The most common chronic diseases were muscu-loskeletal problems, hypertension, cataract, hyperchole-sterolemia, hearing loss and cardiovascular disease, similar to the pattern observed in the other local studies.2,8 As many of our members had been provided with health services before, the number of newly detected problems might be lower than expected. Compared to morbidity patterns in private practice and the public sector of general practice described by Wun YT et al,27 the elderly population in our study had a higher prevalence of hypertension and diabetes mellitus, and more musculoskeletal, hearing, ophthalmological, urologic and psychological problems (Table 13).
Conclusion Local data on the health status of community dwelling elderly people are scanty. Our study provides some useful information on the health profile of this group, particularly on psychosocial issues and social contact. Although this is a biased sample, the information generated can provide better understanding on the health needs of the elderly population. The number of persons 60 years of age and older continues to increase dramatically in Hong Kong. It is estimated that the number of this group will grow to 2.3 million in 2029. A comprehensive health maintenance program of this population is becoming an important task for primary care physicians. In the past 10 years or so, the value of the annual physical examination has been questioned. A standard "annual physical" may not cater the needs of specific age group. As persons grow older, the goals of maintaining social independence, functional mobility and cognitive abilities become increasingly important. In Hong Kong, the top 5 disease burden causing significant patient days of occupancy of hospital beds in the Hospital Authority are: cerebrovascular disease, chronic obstructive pulmonary disease, pneumonia, carcinoma of lungs and fracture of the neck of the femur. The health maintenance programme should therefore include identification of cardiovascular risk factors, lifestyle modification, improvement of function and mobility and prevention of falls. Elderly suicide is also an important problem in Hong Kong. From 1981 to 1995, of all the suicide cases, 35% were elderly aged 60 and above. In a local study, about 30% of those aged 70 or above are possibly depressed whereas in our study 9.1% of elderly client aged 65 and above are possibly depressed. Therefore, screening for depression in high-risk cases appears to be cost-effective. Effective primary care health maintenance of the elderly should include a comprehensive geriatric assessment of physical, functional, social and psychological areas. Using simple and easily administered assessment tools, physicians can improve identification of specific problems that are common in the elderly26 Intervention can be done through health education, lifestyle modification, fall prevention advice, exercise programmes to improve mobility and balance, carer education and support, counselling and medical intervention. These measures could help to bridge the gap between current practice in primary care and hospital geriatric service and ultimately lead to decreased need for hospital admission.
R S Y Lee, FHKAM(Family Medicine)Senior Medical Officer,
K L Chua, FHKAM(Family Medicine) Senior Medical Officer, K Y Lee, FHKCFP, FRACGP Senior Medical Officer, N S C Wu, FHKAM(Family Medicine) Senior Medical Officer,Department of Health. K S Ho, FHKAM(Medicine), FHKAM(Family Medicine) Consultant, W M Chan, FHKAM(Community Medicine) Assistant Director, Elderly Health Services, Department of Health Correspondence to: Dr R S Y Lee, , Room 3502-4, 35/F, Hopewell Center, Queen's Road East, Wanchai, Hong Kong. References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||