|
June 2003, Volume 25, No. 6
|
Original Article
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Prevalence of drug use among the elderly in a local institutional homeX L Sun 孫曉玲, J A Dickinson 狄堅信 HK Pract 2003;25:243-248 Summary
Objective: To review drug use patterns and explore the implications,
thus to identify potential improvements of medical care for the elderly in a nursing
home (NH).
Keywords: Polypharmacy, nursing home, inappropriate prescription and iatrogenic complication. 摘要
目的: 研究護養院老人用藥的情況及形式,探討改善醫療服務的可能性。
Introduction Elderly people are frequently prescribed drugs due to a number of chronic illnesses they have, and hence the likelihood of polypharmacy among them is high.1,2 In Hong Kong, one study on drug use revealed that about 55 percent of the respondents among the community-dwelling elderly had taken medications in the previous month and the average number of drugs was 2.7.3 Another study showed that 70% of respondents were taking drugs, 20% of whom were taking 5 or more.4 Not unexpectedly, the number of drugs used is higher among the institutionalised elderly than the non-institutionalised.5-7 The number of inappropriate medications correlates to the number of medications prescribed.8-10 Not surprisingly, prescription of inappropriate medication is more common among institutionalised elderly persons, so institutionalised elderly are at high-risk of exposure to iatrogenic complications.7,11-20 This also increases the costs of medical care. Studies have shown almost 25% of older outpatients received inappropriate medications, while 50% of inpatients have had inappropriate medication(s).16 Adverse drug reactions are responsible for about 20% of hospital admissions of the elderly.1,4,5,15,16 Knowledge about polypharmacy and its implications in local NHs is limited. To study the prevalence of drug use and explore its implications on the care of the elderly in NH, this paper first describes the profile of drug use and then discusses some important health care concerns in community-based elderly care. Methods Operational definitions
Characteristics of the residents in the NH The NH in this study belongs to a Non-Government Organisation and has 200 beds. The total number of full-time staff was about 130, including 12 professionals (one registered social worker, eight registered nurses, one physiotherapist, one occupational therapist and one doctor). The residents were referred by the Community Geriatrics Assessment Team (CGAT) and had various chronic illnesses. They live permanently in the NH. Their demographic characteristics with their clinical conditions are shown in Table 1. There were 195 residents: 134 were female (68.7%) and 61 were male (31.3%). The mean age was 81.35 years (SD=8.28).
The over 75 years old made up the majority (75.4%) in the NH. Their functional status was poor, 78.5% of them ranging from severely incapacitated to being totally dependent. More than 83.6% were in need of some assistance to move about. There were more residents with impaired cognition (63.1%). The top ten-diseases profile is presented in Table 2. Ten percent of patients attended more than 5 different specialist clinics and 47% more than three. They attended their specialist follow up clinics once every four to 12 weeks.
Drug use The drug-use data were obtained from the population's medication records during the month of June in year 2001. All prescribed drugs including those by the oral, topical, injection and nebuliser routes and p.r.n. medications were recorded. The nine chapter-headings in MIMS21 were used to categorise the drugs, namely: cardiovascular, psychotropic, gastro-intestinal, laxatives, respiratory, metabolism, analgesic/anti-inflammatory, vitamins/minerals and ENT/skin agents. The collected data were statistically analysed by the Statistic Package for Social Sciences. Analysis and results
The total number of drugs prescribed was 813, with a mean of 4.17 (SD=2.31) drugs
per patient shown in Figure 1. Only 4 (2.1%) residents did not
use any medication. Out of 195 residents, 108 (55.4%) were prescribed less than
5 drug(s); while 5 or more medications were prescribed to 83 (42.5%) residents.
Thus, by definition, polypharmacy occurred in 42.5% of all residents. Table
3 shows there was no significant difference in the mean drug-use by
either gender (p = 0.992) or age group (<80 vs
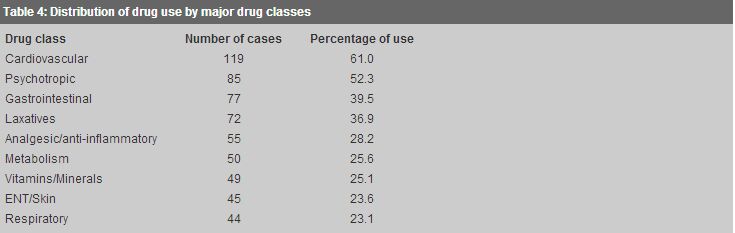
The distribution and usage of the nine drug categories prescribed in the NH are shown in Table 4, as follows: cardiovascular (61.0%), psychotropic (52.3%), gastro-intestinal (39.5%), laxative (36.9%), analgesic/anti-inflammatory (28.2%), metabolic (25.6%), vitamins/minerals (25.1%), ENT/skin (23.6%) and respiratory (23.1%) agents.
Discussion In Hong Kong, there are about 32,000 elderly persons living in residential places belonging to Non-Government Organisations. There is an even higher number living in private residential homes. The majority of them have chronic illnesses.22 The population in this setting is relatively homogenous in terms of the severity of their medical conditions. This NH has identical admission criteria as other NHs, since the CGAT acts as the gatekeeper to NH admissions. The findings in this study can be quite representative of all other NHs in Hong Kong. This study shows that polypharmacy in the NH is prevalent and does not vary amongst the gender and the age group. Compared with previous studies based on community-living older persons in Hong Kong, the number of prescribed medications in this study is higher (4.17 vs 2.4).3 However, the mean number (4.17) is similar to a German study (4.3).5 and that in a medical/geriatric ward of a local hospital (4.65).9 The reasons for polypharmacy among the elderly are complex: multiple chronic medical problems, vague symptoms, patients' and caregivers' pressure to prescribe, use of additional medications to treat drug-related complaints, multiple attending physicians, follow-up by different specialists, lack of co-ordination of total care, size of NH and type of nursing staff all have been implicated as major contributing factors.5,20,23-29 Cardiovascular and psychotropic agents As the Hong Kong population ages so the disease pattern changes and prevalence of chronic disease increases.30 In this study, the top five commonly diagnosed diseases among the elderly are noted to be dementia, hypertension, cerebrovascular accident, heart disease and fractures. Not surprisingly, cardiovascular and psychotropic medicines were among the most commonly prescribed drugs accounting for 61.5% and 52.3% respectively. In Denmark, Nygaard found among 117 permanent NH residents, 75% used cardiovascular agents, and 66.7% used psychotropic drugs.31 In Sydney, Draper et al found that psychotropics were prescribed for 51.1% of residents.32 These findings may reflect the high prevalence of cardiovascular disease and cognitive impairment among patients in NH. However, there are remarkable variations in psychotropic drug use in different NHs with significant variability in treatment cultures.27 There is epidemiologic evidence of misuse of psychotropic and cardiovascular agents in NH; these two kinds of drugs are regarded as the most misused classes in the geriatric population.1,25 In a very busy clinic, it is always easier for a doctor to continue and prescribe the same drug at every treatment visit instead of considering reducing and rationalising the drug used during the follow up. It is essential to critically re-evaluate current diagnosis and management of a patient with cardiovascular disease.33 NH staff are known to mould patients into their institutional routines. The role of psychotropic drugs in the management of the elderly patients with chronic dementing illness is currently unclear.25 Staff perceptions of psychiatric morbidities and their norms as well as the treatment culture of NHs (nurses' beliefs, philosophies of care and their interactions with psychiatrists and mental health workers) have a great impact on the prescription of psychotropic drugs compared to what is the normal practice.25-29 Larson's studies have documented that psychotropic drugs can contribute to global cognitive impairment among older persons.34 It has been shown that residents taking anti-psychotic drugs had significantly more delusions, hallucinations, psychomotor disturbances and aggressiveness. This suggests that there is a role for a non-pharmacological approach, illustrating the need for more research into techniques for patient management in NHs which rely less on drugs. Many authorities now recommend that, among the institutionalised elderly, anti-psychotic drugs should be reserved only for the treatment of acute behavioural disorders, and their routine and long-term use is to be discouraged, even for those with known mental illness.25 Gastro-instestinal agents Chan et al found that gastro-intestinal drugs are the most frequently misused in Hong Kong.9 The H2-receptor antagonists and other antacids are routinely used in asymptomatic patients who are on NSAID and aspirin treatments. Patients and health care workers request these drugs even for asymptomatic patients believing that these drugs can prevent and treat gastro-intestinal bleeding.35 This concomitant therapy has not shown significant benefit in preventing gastric ulcers in patients who have osteoarthritis and are receiving NSAID therapy. A recent prospective study found that asymptomatic patients with rheumatoid arthritis who are taking H2-receptor antagonists had a significantly higher risk of gastro-intestinal complications than those not taking these drugs. The explanation for this interesting observation is unknown.35,36 Although H2-receptor antagonist is effective in reducing NSAID-related dyspepsia, the routine use in asymptomatic patients taking NSAID cannot be recommended.35 Misoprostol, however, can prevent NSAID associated ulcers, but the risks and costs of adding another drug should be borne in mind.1 Laxatives Constipation is a common complaint in the elderly. A Hong Kong study revealed that laxatives were being prescribed to three-quarters of the elderly population in long-term care facilities.37 Only 36.9% of the population in our NH was using laxatives. The low rate of laxative usage was because we were applying a non-pharmacological method in managing our elderly residents and we found this to be effective. We frequently reviewed our residents case by case. Complete cessation of use of oral laxatives may not be successfully achieved. However, the aim should be to reduce these agents and they should not routinely be given without clinical examination. For residents with chronic constipation, bowel dilatation (idiopathic megacolon) is common. The colon should be emptied regularly and enemas or suppositories may be needed sometimes based on the clinical condition. Regular physical examination including per rectum is important; otherwise constipation, leaking stool and faecal incontinence and painless progressive abdominal distension will be missed and intestinal obstruction may occur.37 Conclusion The study found that polypharmacy is a common phenomenon in NHs and does not show any difference between the genders and different age groups. Cardiovascular and psychotropic agents are the most commonly used, followed by gastro-intestinal agents, laxatives and the rest. Further studies are worthwhile to analyse the determinants of drug use and the circumstances in which old people are at risk of polypharmacy. There is a need to find ways to reduce inappropriate drug use as part of the total quality care of the elderly. This will also reduce medical care costs. Since collecting the data in this study and searching through the literatures, the first author has become actively involved in organising and reviewing otherwise unco-ordinated drug treatment regimes. This important role for a family physician is made difficult by the number of specialists the residents attend in order to obtain treatment, and a lack of co-ordination and failure to communicate among caregivers which results in duplicated and conflicting drugs being given to our elderly patients. Acknowledgement We would like to acknowledge our thanks to our reviewers for their constructive comments and to Dr Ho Kin Sang, Consultant of Department of Health for his suggestions. Our special thanks go to Dr Shi Xinping, Associate Professor, Department of Finance and Decision Sciences, Hong Kong Baptist University, for his help with statistics and scrutiny of this manuscript. Key messages
A K Y Cheung, MBBS(HK), DFM(CUHK), FRACGP, FHKAM(Family Medicine)
Private Practitioner, C S Y Chan, MD, LMCHK, FRACGP, FHKAM(Family Medicine) Associate Professor, Department of Community and Family Medicine, The Chinese University of Hong Kong. Correspondence to : Dr A K Y Cheung, c/o: Department of Community and Family Medicine, The Chinese University of Hong Kong, 4/F, School of Public Health, Prince of Wales Hospital, Shatin, N.T., Hong Kong.
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||