|
March 2003, Volume 25, No. 3
|
Original Articles
|
How well do we know chronic hepatitis B patients in Hong Kong family practice? A pilot studyY T Wun 溫煜讚, J A Dickinson 狄堅信 HK Pract 2003;25:108-113 Summary
Objective: To survey (a) family physicians' awareness of patients
with chronic hepatitis B (CHB), (b) some characteristics about these patients including
e-antigen and alanine aminotransferase (ALT).
Keywords: hepatitis B, chronic; hepatitis B e antigens; physicians, family; Hong Kong 摘要
目的: 調查家庭醫生對其患慢性乙型肝炎 (CHB) 病人的了解程度,以及包括e抗原和丙氨酸轉氨酵素 (ALT) 在內的肝炎特徵。
Introduction Chronic hepatitis B (CHB, replacing the previous term "hepatitis B carrier"1) is still common in Hong Kong. The prevalence of positive surface-antigen (HBsAg) ranges from 4.4% in new blood donors to 17.5% in lifeguards.2 Given that family physicians (FPs) as a whole see patients with demographic profiles close to the general population,3 each FP is expected to have around 10% of patients being HBsAg+ve. From the authors' other surveys, we noted that most local FPs were aware of only a minority of their patients' hepatitis B (HB) status. Better knowledge of CHB in the community would help FPs to select appropriate treatment or surveillance for different groups of CHB patients. Though this condition has been widely studied in Hong Kong, most studies are on hospital patients who are likely different from those seen in the community. CHB patients may be either e-antigen positive (HBeAg+ve) or negative. The hepatitis B virus ceases replication in most HBeAg-ve patients,4,5 who do not respond well to interferon6-8 and are more appropriate to be followed in the community rather than in hospital liver clinics.9 The prevalence of HBeAg-ve CHB in Hong Kong population is unknown. An early study in 1980 found that 52.5% of adult blood donors aged 16-40 were HBeAg-ve.10 There are two studies of hospital liver clinics. In 1987 Lok et al reported that 56.2% of their CHB patients (aged 1-75 years) were HBeAg-ve.11 In 2000, Chan et al reported a rate of 69% of their patients (aged 12-80 years).12 These rates are different probably because patients in Lok's study were younger and more likely to be HBeAg+ve. The knowledge of the prevalence of these patients in Hong Kong is important as it "may change our treatment strategies and focus research on the safety and efficacy of treatment".12 A cohort study on CHB patients in the community could provide guides for management options. The aim of this pilot study was to test the feasibility of a large-scale cohort study. Specifically, we sought the rates of HBsAg and HBeAg in family practice, patients' willingness to be followed and the recall of these patients for surveillance. Method The project obtained ethical approval from the Survey and Behavioural Research Ethics Committee, The Chinese University of Hong Kong. We recruited FPs in private practice from East New Territories and East Kowloon. This choice of study population was based on administrative efficiency: FPs in the private sector had more autonomy and office-time in additional activities besides service, and arrangement to access a commercial laboratory was easier for patients from one locality. We compiled a list of private FPs from our Department's list of tutors and the doctor-list of a local pharmaceutical firm (GlaxoWellcome). Letters to all the FPs explained the study and invited them to join. Each FP was asked to collect data from 100 patients aged 30 to 70 years. The FPs could choose to recruit every consecutive or every nth patient they saw within the study period. If a patient was known to be a "carrier" or wished to know his/her HB status, the FP then tested the HBsAg and HBeAg status with a Rapid Diagnostic Kit ("Hepatitis B sAg/eAg whole blood" by AMRAD ICT, Australia). The Kit is a convenient office-test using 100 of blood from a finger prick giving the result within 15 minutes. A study in the US reported a sensitivity of 94.8% and specificity of 100% for HBsAg, as well as 80% and 99.8% respectively for HBeAg.13 All those patients known to be "carriers" or tested positive for HBsAg by the Rapid Diagnostic Kit were recalled six months later for laboratory blood tests that included HBsAg, HBeAg, alpha foetoprotein (AFP), and alanine aminotransferase (ALT) in a commercial medical laboratory with certified quality control. A random sample (generated with computer software) of 10% patients tested negative for HBsAg by the Kit was also recalled for re-testing the HBsAg and anti-HBs antibody. The antigen, antibody and AFP tests were done with the Microparticle Enzyme Immunoassay (MEIA) technology (Abbot Laboratories). ALT was measured by reflectance spectrophotometry of oxidation rate of NADH by alanine (Vitros Chemical Products). Descriptive statistics were used for demographic data. Subgroups were compared with chi-squared test and the significance level (p) was taken as 0.05. Result GP recruited We sent out invitation letters to 143 practices (of which nine were branch clinics) from which about 50 FPs expressed their initial interest. After a briefing seminar to explain the protocol, 20 FPs agreed to participate. Later five FPs withdrew: two changed their practices, two found technical difficulty in drawing blood sample from patients, one found doing the test at office inconvenient to the patient flow. Finally 15 FPs completed data collection. Among them, one FP did not use the Rapid Diagnostic Kit due to time constraints in the practice. Patients recruited Nine FPs sampled 100 consecutive eligible patients. One FP sampled one patient out of every 10, 3 FPs one out of five, one FP every third and another FP every second patient. A total of 1285 patients aged 30-69 years were recruited. Gender was available in 1258 (97.9%): 526 (41.8%) male and 732 female. The mean age ( standard deviation) was 44.2 9.4 years. They had stayed in Hong Kong for 37.4 11.8 years (range: 0-69); 904 (70.4%) were born in Hong Kong, 326 (25.4%) in Mainland China, 29 (2.3%) in South East Asia and 26 (2.0%) in other places of the world. Of them 195 (15.2%) were smokers and 275 (21.4%) were social drinkers. Past history of liver diseases (e.g. jaundice of unknown origin, hepatitis A, acute hepatitis B, hepatitis C) was noted in 81 (6.3%) patients. Eleven (0.9%) were known to have liver cirrhosis of whom one was "carrier". Hepatitis status previously known The FPs knew the HB status of only 251 (19.5%) of previously seen patients but 583 (45.4%) of the patients knew their own HB status. In 595 (46.3%) patients, either the FP or the patient knew the status. Among patients who knew their own HB status, 78 (6.1%) were "carriers". Of these 78, only 17 (21.8%) knew the e-antigen status (3 HBeAg positive and 14 negative), 57 (73.0%) were followed by hospital specialists, but 74 (95.8%) would like to be followed by their own FPs. There were 563 (43.8%) patients who did not know their HB status and were also not vaccinated. Only 234 (18.2%) had HB vaccination. Office test for HBsAg and HBeAg HBsAg was tested for 633 (49.3%) patients: 60 (9.5%) were positive and 573 negative. Though all 78 patients with history of being "carriers" were invited for the test, only 26 (33.3%) agreed and six of them turned out to be HBsAg negative (Table 1). The two previous HBsAg-ve patients who had tested positive by the Kit had not been vaccinated.
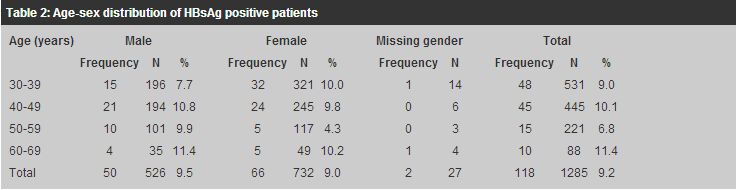
Records of HBeAg were available in 631 patients: six (1.0%) positive and 625 negative. Five HBeAg+ve patients were "new cases"; only one from the three previously known to be HBeAg+ve remained so. Of the 633 patients tested, 11 had previous vaccination (one turned out to be HBsAg+ve). Of those 622 without vaccination, 59 (9.5%) were tested HBsAg+ve with one being also HBeAg+ve. Follow-up blood test We recalled 148 (11.5%) patients for serological testing and 105 (70.9% response rate) returned (39 refused and 4 could not be contacted). Of these 105, 42 had history of being "carriers" and 26 without history but tested HBsAg positive by the Rapid Diagnostic Kit. Of these 68 potential true-CHB, blood tests confirmed that 62 were HBsAg+ve and six HBeAg+ve. Six patients with history of positive HBsAg were shown to be HBsAg-ve. All those tested HBsAg+ve by the Rapid Diagnostic Kit were also positive by the repeated serological test. ALT was done in 65 previously HBsAg+ve patients; seven were above the upper limit of normal (52IU/L) and two above 100IU/L. Except one pregnant female aged 35, all 66 AFP done were within normal range for the laboratory (0.70 - 12.70ng/mL). Estimated prevalence of CHB Because not all the 1285 recruited patients had follow-up serological tests, we assume that people of the following categories have true CHB: (a) those with history of positive HBsAge but not tested again, (b) those HBsAg positive by the Rapid Diagnostic Kit but not tested again, and (c) those tested serologically positive. The overall rate of CHB in this pilot study was thus 118/1285 (or 9.2% of the recruited sample, 95% confidence interval (CI): 7.6% - 10.8%). Complete age-sex data were available for 1258 patients (Table 2), showing a rate of 9.5% for males and 9.0% for females.
Of the 118 CHB, 76 (64.4%) were born in Hong Kong, 38 (32.2%) in Mainland China, 3 (2.5%) in South East Asia, and one elsewhere. Fisher's Exact Test shows no significant difference between Hong Kong born and non-Hong Kong born as a risk to CHB. HB e-Antigen negative patients
Serological test for HBeAg was done in 68 CHB patients. Six (8.8%, 95% CI: 2.1%
- 15.6%) were confirmed to be e-antigen positive. The HBeAg+ve patients were younger
(mean age Discussion This study recruited 1285 patients aged between 30 to 69 years from a convenient sample of local private FPs. Only 46.3% patients had known HB status by either themselves or FPs, and FPs knew the status in less than 20% of their patients. Of those 43.8% (563) patients who did not know their hepatitis B status and had not been vaccinated, 36 were later tested HBsAg+ve by the Rapid Diagnostic Kit. Since the six-month follow-up laboratory tests showed no false positives for the Kit, these patients were likely to be true CHB. FPs should enquire more about their patients' HB status and advise immunisation accordingly. We successfully recalled 42 of the 78 patients known as "carriers" for repeated serological tests after six months and six (14.3%) were found to be HBsAg negative. Some patients might have been incorrectly labelled as CHB (the "carriers"), or wrongly informed. Patients are sometimes labelled as "carriers" after one serological test, without re-testung six months later. It is often assumed that adults in Southern Asia have been infected with HBV early in their life14,15 and hence HBsAg+ve adults are assumed to have CHB without serological confirmation. Another possibility is that some HBsAg+ve patients have seroconversion later in their life but there are no data on the rate in Hong Kong. As 14.3% of the "carriers" in this study were HBsAg-ve on serological re-test, care should be taken to distinguish between HBsAg+ve and CHB in reading reports on the prevalence of HB. It is often mis-quoted that among Hong Kong population "9.5% are carriers" of HB.16 This prevalence was based on a study in 1978-1979 involving 15660 blood donors (aged 16-40 years) and hospital in-patients (non-liver diseases, 345 aged below 16 and 329 aged above 40 years).17 However, the prevalence was not that of "carriers" but HBsAg+ve patients as the HB status was not repeated and the study was not done in a general population. The estimated prevalence of CHB in this study is 9.2% (95% CI: 7.6% - 10.8%). This is close to the prevalence of positive HBsAg previously reported in Hong Kong.2,10 The rate is likely to be an over-estimation. The assumption that those with HBsAg+ve history were true CHB was an over-assumption, as 14.3% of the recalled patients from this group turned out to be HBsAg-ve. If we assume that same proportion of 78 patients known to be previously HBsAg+ve but not re-tested would turn out to be negative, the estimated number of CHB in our sample would be 8.3% (95% CI: 6.8% - 9.8%). The estimated prevalence is thus between 8.3% and 9.2%. It must be emphasised that these estimations are extrapolated from data limited by sampling and attrition (follow-up) bias in this study. This study is not meant to be a proper prevalence study but serves as a guide for future research or working hypothesis - a purpose of a pilot study. This study, in contrast to most other studies, found similar prevalence of HBsAg in both sexes and we find this perplexing. A survey in 1997 of 5500 adults in the community by the United Christian Nethersole Community Health Service found that 9.3% males and 9.1% females aged 45-54 were HBsAg+ve (personal communication, also in South China Morning Post 27 Feb 1998). The majority of our recruited patients were in the similar age group. It is often postulated that immigrants from Mainland China keep the prevalence of CHB in Hong Kong higher than expected. In a survey of pregnant women attending antenatal clinics in Hong Kong, the prevalence of positive HBsAg was significantly higher in those from Mainland China than the local born.18 The present study however does not show any difference in birthplace among patients of CHB. The prevalence of positive HBeAg in CHB from this study (8.8%) is far below those reported from hospital liver clinics (54% and 31%) and from blood donors (47.5%, aged 16-40 years).10 The difference may be due to the different age groups of patients, the tendency of liver clinics to follow patients with serious liver diseases or newly detected CHB patients and to the possibility that young blood donors 20 years ago might have been infected in their early adulthood. This study recruits only nine HBeAg+ve patients and this sample size is too small for valid statistical analysis e.g., the higher ALT levels in HBeAg+ve patients relative to their counterparts. Many drugs and herbs raise the serum ALT and it was uncertain whether our sampled patients were currently on drugs/herbs. The significance of mildly elevated ALT in HBeAg-ve patients needs further study. In view of the relatively low prevalence of e-antigen and absence of active liver dysfunction (ALT less than twice upper limit of normal), most CHB patients could be followed outside hospitals. Limitations of this pilot study The response rate (16%) from FPs in this study is very low and the convenient sample could cause bias. It could be argued that the recruited physicians and patients in this study might not truly represent all the family practices in Hong Kong. To obtain better estimate of prevalence, a sample size of 8600 patients is required to find 770 CHB patients of whom 100 would be HBeAg+ve. This estimation assumes 100% follow-up rate though this is unlikely. Our study could recall only 71% patients for free laboratory tests. The response rate does not only affect the estimated sample size of future studies but also constitute a source of bias that needs to be minimised. The study did not have enough resource to test the HBV-DNA levels on the CHB patients. The viral activity thus could not be fully assessed. In future studies, it is more desirable to have HBV-DNA tested. Conclusion FPs should promote more HB immunisation, as 43.8% of their patients have not been vaccinated and they know the HB status of only 19.5% patients. Some patients of "known carriers" may not have true CHB. CHB patients in family practice have 8.8% prevalence of positive HBeAg and the liver enzymes are mostly within normal limits. They might require just observation rather than aggressive management. Acknowledgement We thank GlaxoWellcome for organising the seminar for FPs and sponsored the Rapid Diagnostic Kits for this study. We also thank the following FPs for their hard work in collecting data: Drs Chan Suen Ho Mark, Chan Yuk Ng Patrick, Cheng Kin Keung William, Cheung Kit Ying, Fong Yuk Fai Ben, Lau Tin Kay Peter, Liu Ka Ling, Ma Ping Kwan Danny, Cameron Tallach, Tang Kuen Yan Alfred, Tsang Hon Keung Andrew, Wong Nai Ming, Wong Ping Leung, Wong Wing Sang Bernard, Yeung Shou Fong Annie. The study was supported by Direct Grant #2001.1.060 from The Chinese University of Hong Kong. Key messages
Y T Wun, MBBS, MPhil, MD, FHKAM(Fam Med)
Former Associate Professor, Department of Community and Family Medicine, The Chinese University of Hong Kong. J A Dickinson, MBBS, PhD, CCFP, FRACGP Professor of Family Medicine, University of Calgary, Alberta, Canada. (Former Professor of Family Medicine, Department of Community and Family Medicine, The Chinese University of Hong Kong) Correspondence to : Dr Y T Wun, Research Committee, The Hong Kong College of Family Physicians, Room 701, 99 Wong Chuk Hang Road, Aberdeen, Hong Kong.
References
|
|