|
November 2005, Volume 27, No. 11
|
Update Articles
|
|
Medical Rehabilitation Update: Using metered-dose inhaler in chronic obstructive pulmonary diseaseHo-Pui So 蘇浩培 HK Pract 2005;27:411-415 Summary Metered-dose inhaler is frequently prescribed to clients with chronic obstructive pulmonary disease. The use of spacer device is the preferred method and larger spacer works better. The technique of inhalation is discussed alongside with evidence in supporting the advice. 摘要 定劑量吸入器是慢性阻塞性肺病患者的常用處方。在使用時輔以助吸器更為可取, 而較大的助吸器會有更佳效果。本文論述噴霧劑吸入的使用要訣, 並以研究證據支持各項建議。 Introduction Bronchodilators like salbutamol (Ventolin) and ipratropium (Atrovent) are frequently prescribed to patients with chronic obstructive pulmonary disease (COPD). The inhaled form is preferred to oral or parenteral medications as systemic side effects are lower. The inhaled drug is commonly delivered via metered-dose inhaler (MDI) with the help of a spacer. Inhaled steroid is also recommended in stages III and IV COPD accordingly to the GOLD Report1 of WHO. In order to optimise the drug particles reaching the airway, some procedures on delivering the drug should be followed. This article aims at highlighting the practice points in the manoeuvre and whenever available, supporting the advice with evidence from original research papers. As many clients with COPD are elderly, some compromise in the technique may be necessary and the alternatives will also be discussed. Background information Inside a canister, the drug is suspended in liquid propellant under pressure, and with each actuation, the suspended drug in the metering chamber of the canister is released with the vaporised propellant. The drug is released in fine particles and the optimal respirable range of particle size to reach airways is 6.8 - 3.1 mm. Even smaller particles (< 3.1 mm) tend to suspend in air and reach alveoli and larger particles be centrifuged and deposited in mouth and throat. The formation of particles involves creating surface areas and energy is required to overcome the surface tension. The role of the propellant is to deliver the energy, and the production of finer particles requires more energy input. The propellant used was Chlorofluorocarbon (CFC) and it damages the ozone layer of the atmosphere. In 1987, the Montreal Protocol, an international treaty signed by more than 150 countries, was initiated to phase out worldwide CFC usage. The United Nations Environment Programme proposed a complete ban on CFC MDIs by 2005. Many proprietary products are shifting to Hydrofluoroalkane (HFA) and generics may follow suit. Frequently, a spacer is prescribed with MDI to smooth coordination between actuation and inhalation. The spacer2 also reduces oropharyngeal deposition of drug. In addition, the extra space allows deceleration and evaporation of particles, resulting in a higher proportion of respirable particles. In human studies, the plasma levels of drug measured after inhalation and in the first 20 minutes reflect absorption through the lung. Subsequent levels are affected by gastrointestinal absorption. In other studies, artificial lung is employed with multistage liquid impinger (MSLI) and particles < 6.8 mm are referred to stages 3 and 4 in MSLI. Evidence based advice and discussion Practice tips 1
MDI containing drug in suspension must be shaken before use to resuspend the drug. In one study,3 not shaking the MDI before use reduced the total dose by 25.5%, and the respirable dose by 35.7%. For a new MDI, discard the first two actuations, as the dose may be subnormal. Practice tips 2
Multiple actuations of the MDI into spacer decrease the amount of respirable drug recovered. This is because of agglomeration of particles increasing their size, displacement of aerosol out of the spacer or onto the spacer walls, or the electrostatic attraction of particles to the spacer and between each other. In a study4 of CFC MDI with MSLI, the total dose of salbutamol recovered (mg) per 100 mg actuations via Volumatic spacer was 62.1 for 1 actuation, 49.7 for 2 actuations and 22.7 for 5 actuations. Practice tips 3
In a study3 of salbutamol MDI using MSLI, two actuations separated by one second only reduced the respirable dose (particles < 6.8 mm) by 15.8%, while four rapid actuations reduced the respirable dose by 18.2%. This is due to adiabatic cooling of the metering chamber. Practice tips 4
In a study5 with healthy volunteers, single puff of salbutamol with delay of 20s from a Volumatic spacer resulted in a considerable decrease in the delivery of salbutamol to the lungs with considerable lower plasma level. For maximal concentration, this amounted to a 1.80 fold greater lung bioavailability for single puffs without delay (5.11 ng/ml) than for single puffs with a 20 second delay (2.92 ng/ml). In another study6 using different spacers and drugs, all samples had a lower recovery of drug after a delay between MDI actuation and sampling. In an MSLI experiment, the drug half-life was 15s for beclomethasone, 8 - 10s for salmeterol and 8 - 9s for fluticasone. In practice, ask patient to breathe in and out normally, and close lips around mouthpiece of spacer. After breathing out as far as comfortable, actuate the MDI and breathe in steadily and deeply through the mouth. Hold breath for 5 - 10 seconds. If patient cannot hold breath, breathe in slowly and deeply through mouth for 2 more times. Practice tips 5
In a study7 with MSLI, the electrostatic charge in plastic spacers limited the delivery of drug (salbutamol), and the charge could be reduced by soaking the spacer in household detergent. In another study,5 a detergent washed spacer performed as well as the specific anti-static lining spacer. Practice tips 6
In a study8 on disodium cromoglycate and salbutamol using MSLI, large volume spacers such as Nebuhaler (750 ml) and Volumatic (700 ml) delivered significantly more drugs than the smaller spacers tested like Aerochamber (145 ml) and Aerosol Cloud Enhancer (ACE, 160 ml). As percentages of 5 mg nominal dose of disodium cromoglycate, the recovered particles (< 5 mm) were 10.4, 3.0, 2.8 for Nebuhaler, Aerochamber and Aerosol Cloud Enhancer respectively. For the 100 mg dose of salbutamol, the corresponding percentages (< 5 mm) were 54.3 and 20.0 for Volumatic and Aerochamber. In volunteers9 using the early lung absorption profile (0 - 20 mins), for the administration of the same nominal dose, the large volume spacers (Nebuhaler and Volumatic) delivered more salbutamol than the MDI (HFA Airomir) alone. The plasma salbutamol peak and average values (ng/ml) were 8.87, 8.09 for Nebuhaler; 6.54, 5.83 for Volumatic and 4.37, 3.90 for Airomir MDI respectively. Practice tips 7
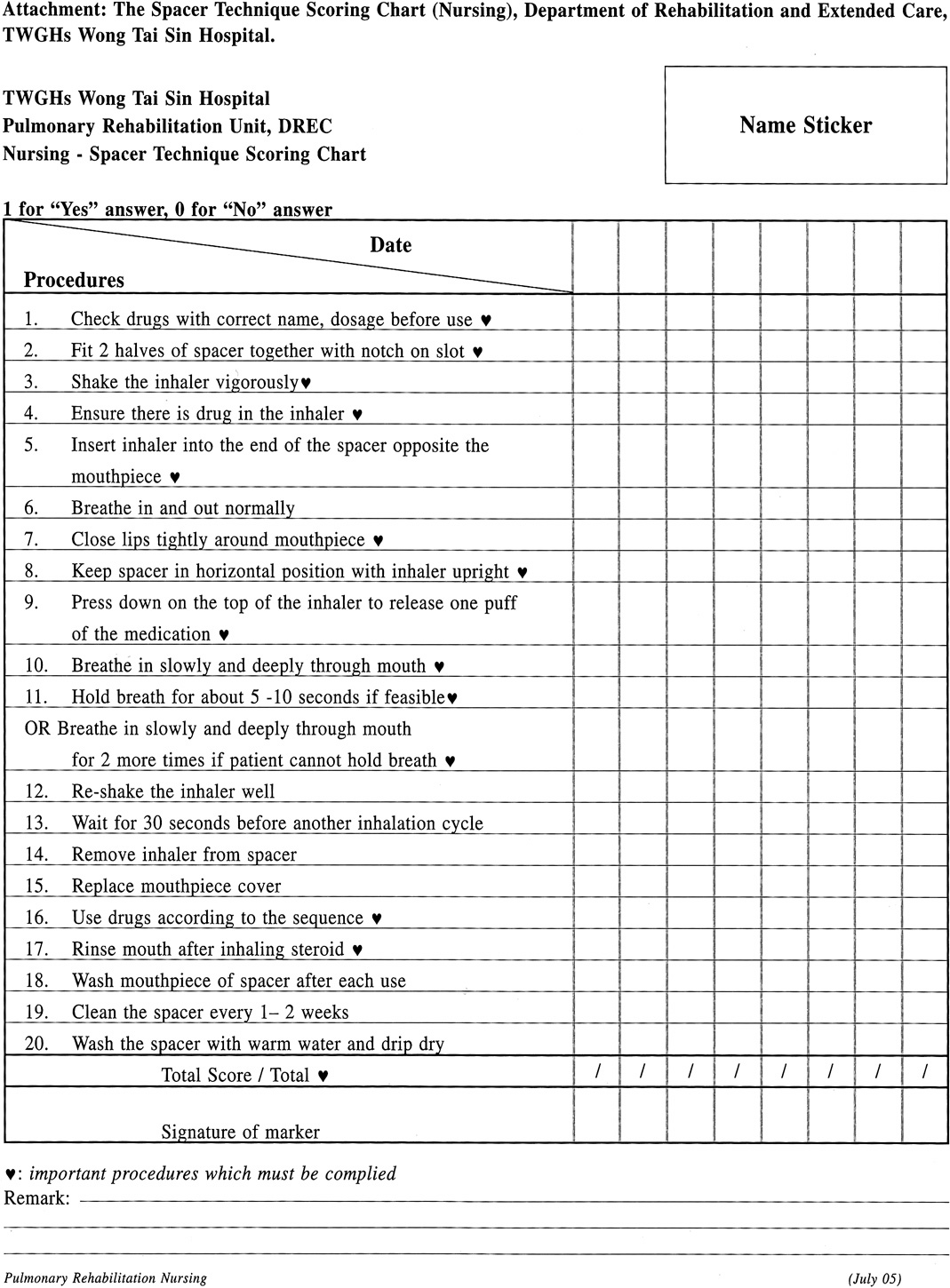
In a study10 with salbutamol, the HFA formulation delivered more drug than the CFC formulation when used with either the large or small spacers. This may be because less drug is deposited in the spacer from the HFA formulation, which is emitted from the MDI at a slower speed and occupies a small volume. Conclusion In patients with COPD who are mainly elderly and largely sedentary, it is best to use the spacer and choose large volume ones to maximize the drug delivery. In patients with mild symptoms, the medication compliance may not be all that important and convenience may be an important consideration. In difficult situations, there are also other drug delivery devices distinct from MDI, and are more handy to use. Though they usually carry higher costs, they are viable alternatives in special situations. Attachment: The Spacer Technique Scoring Chart (Nursing), Department of Rehabilitation and Extended Care, TWGHs Wong Tai Sin Hospital. Key messages
Ho-Pui So, MBBS(HK), MSc (Respiratory Medicine) (Lond), FHKCP, FHKAM (Medicine)
Consultant-in-Charge, Department of Rehabilitation and Extended Care,TWGHs Wong Tai Sin Hospital. Correspondence to : Dr Ho-Pui So, Department of Rehabilitation and Extended Care, TWGHs Wong Tai Sin Hospital, 124 Shatin Pass Road, Kowloon.
References
|
||