|
January 2007, Volume 29, No. 1
|
Update Articles
|
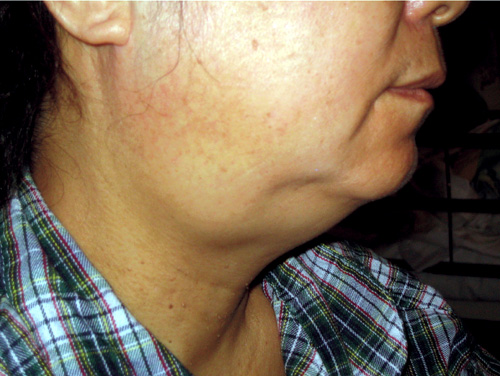
Management approach of salivary gland swellingsSiu-kwan Ng 吳少君, Alexander C Vlantis 屈力行 HK Pract 2007;29:10-15 Summary A salivary gland swelling is an important differential diagnosis that needs to be considered for an upper neck or intra-oral swelling. Important non-neoplastic causes include infection, obstructive duct disease, cysts and Sjoo02gren's syndrome. Neoplasms of parotid glands are usually benign whereas those of sublingual and minor salivary glands are often malignant. Most salivary neoplasms require surgical excision for definitive diagnosis and treatment. 摘要 唾液腺腫脹是重要的上頸部或口腔內腫瘤的鑒別診斷之一。 主要的非腫瘤性病因包括感染、唾液腺管道阻塞、囊 腫和Sjoo02gren氏綜合症。腮腺瘤通常為良性, 而舌下線和小唾液體瘤常為惡性。大多數唾液腺瘤需要外科切除才能確診和徹底治療。 Introduction There are 3 pairs of major salivary glands, namely the parotid, submandibular and sublingual glands. In addition, there are hundreds of minor salivary glands situated in the mucosal lining of the upper aerodigestive tract. Salivary gland diseases usually present as a swelling of the affected gland. This article offers an overview of the management of patients with salivary gland swellings. Location of salivary gland swellings A salivary gland swelling can present in a variety of locations, depending on the salivary gland affected. A swelling that arises in the parotid (Figure 1) or submandibular gland (Figure 2) usually presents as an upper neck mass. A swelling of a minor salivary gland or sublingual gland typically presents as an intra-oral swelling. However, minor salivary gland tumours can sometimes occur in other areas of the upper aerodigestive tract including the nasal cavity, paranasal sinuses and larynx. Figure 1 shows a small parotid tumour in the region of the parotid tail. When a lump occurs in this region, the differential diagnosis must include a mass of parotid origin. Parotid tumours can be sizeable at times (Figure 3).
Figure 1: Small parotid tumour
Figure 2: Submandibular swelling
Figure 3: Big parotid tumour Intraoral salivary gland swellings Salivary extravasation / retention cysts and neoplasms are the 2 main causes of intraoral salivary swellings.
Salivary retention cysts and the more commonly occurring extravasation cysts are due to minor salivary gland duct obstruction and leakage of saliva from damaged ducts respectively. They are commonly situated in the buccal mucosa near the lips and in the floor of the mouth. When they occur in the floor of the mouth, they are termed a ranula, which is a bluish semitranslucent cyst which resembles the belly of a frog (Figure 4). The treatment for them is either simple excision or marsupialization. Ranulas are prone to recur, and when this happens, the cyst together with the sublingual gland should be excised. Less commonly, sublingual and minor salivary gland neoplasms present as firm intraoral swellings. Although malignant minor salivary gland tumours can occur in any part of the upper aerodigestive tract, they are most often located on the palate1. Nevertheless, minor salivary gland neoplasms are uncommon and the clinician should differentiate them from the more common palatal condition known as torus palatini (Figure 5). This is a common benign condition of the hard palate which is central, bony hard lined by normal smooth mucosa and varies greatly in size. However, they do not require active treatment unless large enough to cause problems e.g. denture problems or recurrent ulceration of the overlying mucosa during eating, in which cases they are surgically removed.
Figure 4: Ranula
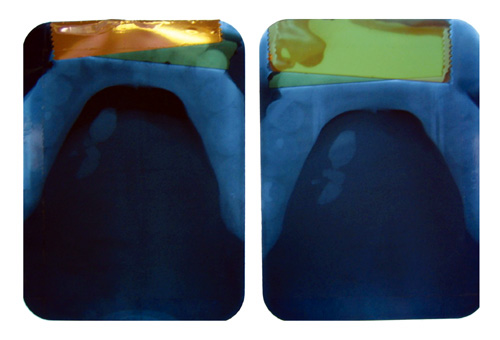
Figure 5: Torus palatini A bulge or medial displacement in the lateral oropharyngeal wall may be due to a tumour of the deep lobe of the parotid gland. The diagnosis of an intraoral salivary extravasation / retention cyst is usually obvious and straightforward. For other swellings, a biopsy is usually simple to perform and reliably establishes the diagnosis. Treatment is according to the diagnosis. A biopsy of the floor of the mouth or oropharynx should be made by a relevant specialist due to the proximity of vital structures such as the lingual nerve and internal carotid artery. Salivary gland swellings presenting as a neck mass When a salivary gland swelling presents as a neck mass, a different approach is adopted instead of a direct incisional biopsy, which is either unnecessary or may even jeopardize subsequent treatment. Bilateral diffuse salivary gland swellings are often related to alcoholism or diabetes. Other causes of salivary gland swellings can be broadly categorized as non-neoplastic or neoplastic. Non-neoplastic salivary gland swellings Important non-neoplastic lesions include infection, obstructive duct disease, Sjgren's syndrome and salivary gland cysts. Infection- parotitis Parotitis is the commonest presentation of salivary gland infections. While viral parotitis is commonly caused by mumps, it can also be caused by other viruses such as echo- and coxsackie viruses. Therefore, life-long immunity to mumps infection does not preclude a person from developing parotitis again. Patients with parotitis should be treated adequately for pain, dehydration and poor oral hygiene. Bacterial parotitis mostly occurs in dehydrated and debilitated patients with poor oral hygiene. It usually results from an ascending staphylococcal infection of the parotid duct. The most common pathogens are Staphylococcus aureus and anaerobic bacteria.2 The clinical features include a painful and tender parotid swelling, fever and trismus due to spasm of nearby muscles such as the masseter, temporalis and pterygoids. Pus may be expressed from the parotid papilla by light pressure on the parotid gland. The patient should be actively rehydrated and given intravenous antibiotics. A high-calorie liquid oral supplement may be given if a normal diet cannot be tolerated due to pain. The general measures for viral parotitis should also apply. An abscess should be suspected if a patient has a severe swelling or does not respond to medical treatment. In the case of a suspected abscess, imaging is necessary to confirm the diagnosis and to assist in planning the surgical drainage if necessary. Obstructive salivary ductal diseases- salivary duct stones Obstruction to the outflow of saliva is usually due to intraductal stones although it can also be due to duct strictures and kinks.3, 4 Salivary duct stones are most commonly found in Wharton's duct (i.e. the submandibular duct) as submandibular gland saliva is more alkaline and viscous than parotid saliva. Other contributing factors include an ascending course of the submandibular duct, a dependent submandibular gland, a wide lumen and a tight orifice.5 Nevertheless, stones can also occur in the parotid duct. Typical clinical symptoms include a recurrent swelling of the affected gland due to obstruction of the salivary outflow, which may be precipitated by food and is associated with distension, discomfort and pain. The swelling is intermittent, lasting for a few hours to a day, but will persist if it is complicated by a bacterial infection. A submandibular duct stone is often palpable in the floor of mouth due to its hard consistency and superficial position. While most stones of the submandibular duct are visible on plain X-ray (Figure 6), most parotid duct stones are radiolucent. Computerized tomographic (CT) scans and ultrasonography demonstrate sialoliths (i.e. salivary stones) in a high percentage of cases. Some investigators advocate fast T2-weighted magnetic resonance imaging (MRI) with thin slice sections as a non-invasive technique to evaluate the ductal architecture of salivary glands and to identify stones.5 In some centres, MRI has replaced conventional sialography.
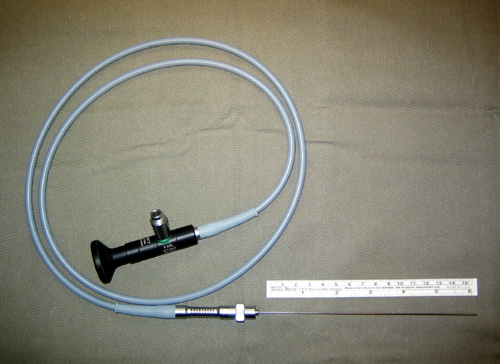
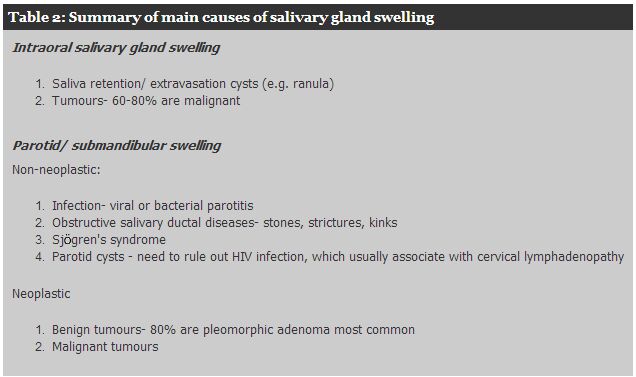
Figure 6: Submandibular stones shown on plain X-ray Submandibular stones situated close to the duct opening can be removed by incising the duct transorally. For stones located more posteriorly and deeper, the conventional treatment is surgical excision of the affected submandibular gland. As technology advances and endoscopes become thinner, intraluminal endoscopic removal of stones using thin semi-rigid endoscopes i.e. the sialendoscopes (Figures 7, 8) have been reported with excellent results.3, 6 This technique is gaining popularity in other parts of the world and is particularly valuable in treating parotid stones in those patients who fail conservative treatment and where the conventional treatment of a parotidectomy is a major operation which is associated with a high risk of facial nerve injury due to adhesions after repeated bouts of infection.
Figure 7: Sialendoscope
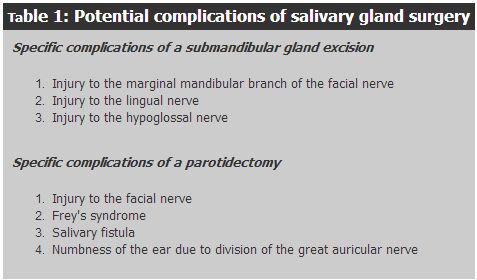
Figure 8: Sialendoscope inserted into a sheath with a working channel Sjgren's syndrome Sjgren's syndrome is an autoimmune condition that may be associated with other connective tissue diseases such as rheumatoid arthritis. The well-known symptoms of this syndrome are dry eyes, a dry mouth and a parotid salivary gland swelling. The diagnosis is established clinically, serologically (measuring anti-Sjoo02gren's Syndrome antibodies A and B, SS-A and SS-B) and histologically (a labial biopsy shows peri-ductal lymphocyte infiltration of minor salivary glands). Apart from the physical discomfort, a patient with Sjoo02gren's syndrome is at a higher risk of developing a lymphoma than the normal population. Parotid cysts In clinical practice, the commonest cause of a clinically detectable cystic swelling of the parotid gland is a Warthin's tumour, although other tumours including mucoepidermoid carcinoma may also be cystic. A Warthin's tumour is most commonly found in elderly males and is bilateral in 10% of cases. It can be readily differentiated from a true simple cyst by ultrasonography. When multiple true cysts involve one or both parotid glands, HIV infection must be considered and needs to be excluded. HIV related parotid cysts are lymphoepithelial cysts and usually associated with cervical lymphadenopathy. Neoplastic salivary gland swellings The rate of malignancy of tumours of the salivary glands varies according to the gland. Although most salivary gland tumours (about 80%) occur in the parotid gland, the rate of malignancy of parotid tumours is about 20%, of submandibular gland tumours about 50% and of sublingual or minor salivary glands about 60-80%.7 Salivary gland neoplasms usually present as a solid, focal and painless mass. Features of malignancy include rapid growth, fixation of the mass, infiltration of surrounding nerves (e.g. facial nerve palsy) and enlarged regional lymph nodes. These signs often occur in advanced tumours and are usually absent in early lesions that are more commonly seen in daily clinical practice. The clinical examination is not sensitive enough to make a reliable distinction between benign and malignant tumours. A useful diagnostic tool is ultrasonography, which is non-invasive and relatively cheap. It confirms the intra-salivary location of a mass and also guides fine needle aspiration. CT scan or MRI may be required in larger lesions to define the anatomical relationship of the tumour and gland with surrounding structures and for surgical planning. Although fine needle aspiration cytology (FNAc) is usually done routinely, most salivary gland tumours, with the exception of lymphomas, need to be excised even if the FNAc is reported as benign. There are a number of reasons for this. Firstly, FNAc is not 100% accurate, and the accuracy varies according to the experience of the cytopathologist.8 Secondly, the commonest benign tumour is a pleomorphic adenoma which has the potential to undergo malignant transformation in a long-standing case. Thirdly, many patients may also want the tumour removed for cosmetic reasons. Despite the drawbacks, FNAc is still useful and usually forms part of the diagnostic work-up. There are 2 main reasons for this. Firstly, non-neoplastic lesions can sometimes be confidently diagnosed e.g. TB. In these cases, surgery can be avoided altogether and patients treated accordingly. Secondly, if cytology does diagnose a malignancy, which is highly specific,8-10 it helps in the surgical planning and enhances better pre-operative counselling. The issue of possibly sacrificing surrounding structures to obtain an oncological clearance can then also be discussed with the patient. The aim of surgery is to achieve an en-bloc removal of the tumour with a cuff of surrounding normal salivary gland tissue. The rationale lies in the fact that the definitive diagnosis is made after the surgery. Furthermore, a pleomorphic adenoma, which is the commonest salivary gland tumour, lacks a complete capsule and tumour can project through dehiscences as small bosselations. Therefore, the recurrence rate can be high after simple enucleation, and revision surgery can be very difficult with a significantly higher risk of facial nerve damage. It follows that submandibular gland tumours are treated by submandibular gland excision and parotid gland tumours usually require at least a partial parotidectomy with identification of the facial nerve. The potential surgical complications of a submandibular gland excision or parotidectomy are listed in Table 1. In experienced hands, the risk of major complications is low. Frey's syndrome probably deserves some elaboration. This refers to a condition whereby patients who underwent parotidectomy develop skin erythema and sweating of the ipsilateral parotid area during eating. It is a result of misrouting of regenerated cholinergic secretomotor fibers that normally supply the parotid parenchyma to overlying cutaneous glands. It is a common side effect of a parotidectomy and may occur in over 50% of patients.11 Nevertheless, the majority of patients have mild symptoms and do not need active treatment. For other cases, topical anticholinergics can be prescribed. For significantly symptomatic cases, intradermal Botoxrrrrr injection can be given into the affected skin. It is well tolerated and has a high success rate with a long duration of action.12, 13 In Laccourreye's series, the 1-, 2-, and 3-year actuarial estimate for symptomatic recurrent gustatory sweating was 27%, 63%, and 92%, respectively. For those who have recurrent symptoms, the severity was always reduced when compared to the severity at the initial presentation. Furthermore, re-injection of botulinum toxin type A remains an option.13 Table 2 summarizes the main causes of salivary gland swelling.
Conclusion The variety of salivary gland diseases is wide. The commonest causes include infections, duct stones and neoplasms. By taking a careful history and performing a thorough physical examination, supplemented with ultrasonography when necessary, the clinician can make an accurate diagnosis in the majority of cases. Key messages
Siu-kwan Ng, MBChB, FHKAM(ORL)
Associate Consultant, Division of Otorhinolaryngology, Department of Surgery, Prince of Wales Hospital. Alexander C Vlantis, MBBCh, FCS(SA)ORL Associate Professor, Division of Otorhinolaryngology, Department of Surgery, The Chinese University of Hong Kong. Correspondence to : Dr Siu-kwan Ng, Division of Otorhinolaryngology, Department of Surgery, Prince of Wales Hospital, Shatin, N.T., Hong Kong.
References
|
|