|
October 2007, Volume 29, No. 10
|
Original Articles
|
Predictive risk factors for complications following fish bone ingestionTak-shun Poon 潘德信, Cheuk-wai Yuen 袁卓煒, Kam-shing Fung 馮錦盛 HK Pract 2007;29:374-379 Summary
Objective: To identify the predictive risk factors for complications
developed in patients presented with fish bone ingestion.
Keywords: Fish bone ingestion, risk factors, complications 摘要
目的: 確認病人誤吞魚骨後產生併發症的危險因素。
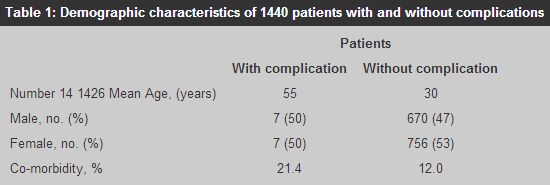
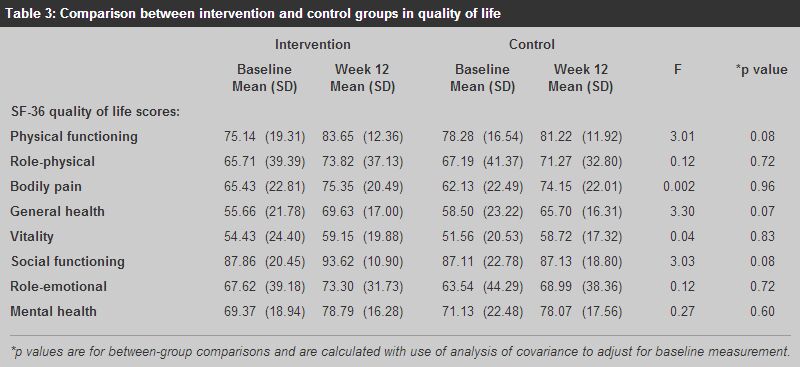
主要詞彙: 誤吞魚骨,危險因素,併發症。 Introduction Fish bone ingestion is a common clinical presentation. More than 600 patients are managed by doctors of our department alone annually. Complications associated with fish bone ingestion are uncommon, but potentially fatal. Oesophageal perforation, retropharyngeal abscess and even aorto-oesophageal fistula had been reported.1 The natural history and complications of fish bone ingestion could be found in various literatures. However, the relationships of risk factors and its development of complications are seldom addressed. Study of the complications encountered may reveal the potential risk factors present and hopefully alert our doctors when managing these patients in the future. Methods Through the Computerized Clinical Data Analysis & Reporting System, patients with a discharge diagnosis of foreign body ingestion between January 2005 and December 2006 were included. Patients with foreign body ingestion other than fish bone were excluded. 1440 consecutive patients were successfully retrieved and studied retrospectively. Demographic data, symptoms, duration of symptoms, co-morbidity, soft tissue lateral neck X-ray findings, endoscopic findings and complication were recorded. Results were expressed as the mean or median (range) for quantitative variables. Univariate and multivariate analysis of clinical data was conducted with SPSS version 13.0 (SPSS Inc., Chicago, IL) software. Analysis of association between complications and risk factors was done with Fischer's exact test and Pearson's chi-square test. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Multivariate logistic regression was performed to analyze the potential risk factors for complications. The factors included in the multivariate model were those that showed a significance level of < 20% in the univariate analysis. P values < 0.05 were statistically significant. Telephone follow-up was arranged if patients refused admission or refused oesophagogastroduodenoscopy (OGD) after admission. Results Of 1440 patients with complaints of fish bone ingestion, 681 (47.3%) were men and 758 (52.7%) were women. The male to female ratio was 1:1.1. The mean age (year) was 32 (Range: 3 years - 82 years old). 210 patients (14.6%) had co-morbidities including hypertension, diabetes, stroke, ischaemic heart disease, asthma and chronic obstructive airway disease. (Table 1) The mean duration of symptoms before consultation was 2.2 days. The 3 commonest symptoms were foreign body sensation in the throat (1296, 90%), pain on swallowing (720, 50%) and blood stained saliva (173, 12%). (Table 2) 605 (42%) patients had their fish bones removed by direct laryngoscopy. X-ray of neck (soft tissue lateral view) was performed in 794 patients (55.1%), in which 119 (15%) were reported positive. X-ray as a diagnostic tool of fish bone ingestion has low sensitivity (31%) but high specificity (91.4%). (Table 3) OGD was performed in 794 patients (55.1%), in which 236 patients (29.7%) had their fish bones successfully retrieved, while remaining 558 patients had negative OGD. Fish bone was most commonly located at oropharynx (62%), followed by valleculae (25%) and pyriform fossa (8%). 41 patients did not undergo OGD, amongst whom 18 (44%) patients refused and 23(52.3%) patients with their symptoms resolved after admission. Telephone follow-up of these patients did not reveal any subsequent morbidity or mortality.
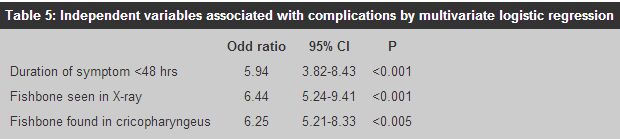
Among 1440 patients with fish bone ingestion, 14 (1.0%) patients developed complications. 12 patients had retropharyngeal abscess and 2 patients had oesophageal perforation. 8 patients required surgical drainage of retropharyngeal abscess. All patients were discharged from hospital uneventfully. The mean hospital stay for complicated patients was 12.2 days. No mortality was reported. Potential risk factors for complicated cases were determined by X2 test or Fisher's exact test. Statistically significant risk factors were: foreign body sensation in throat, co-morbidity, duration of symptoms >48 hours, positive X-ray findings, and fish bone impaction at cricopharyngeus. (Table 4) Multivariate logistic regression was used to further analyse the risk factors. Predictive risk factors significantly associated with complications were: (1) duration of symptoms >48 hours (P<0.001), (2) positive X-ray findings (P<0.001), and (3) fish bone impaction at cricopharyngeus (P<0.005). (Table 5)
Discussion Fish bone ingestion is a frequently encountered clinical entity. It can occur in children, adult and the elderly, regardless of sex. It was reported that fish bones tend to lodge in the oropharynx (posterior tongue, vallecula and tonsil).1 62% of fish bones discovered in our study were found impacted in the oropharynx. Fish bones frequently lodge themselves in the tonsils, but sometimes only a tiny length may project above the surface lining. And with the disturbance of light from laryngoscope, it may be visualized as saliva instead and therefore, fish bone missed is lodged in the tonsillar bed. Most other fish bones tend to be impacted at site of narrowings of the pharyngo-oesophageus. These are the piriform fossa and the post-cricoid regions, particularly at the level of the cricopharyngeus muscles because these are the anatomical narrow regions in the upper gastrointestinal tract.2 Prediction of the presence of fish bones by symptoms alone is unreliable. Of 1296 patients who had foreign body sensation in the throat, 455 patients (35.1%) did not have any fish bones identified by laryngoscopy or OGD. Although most patients give a reliable history of fish bone ingestion and the localization is possible with the patient frequently pointing to the side affected, abrasion and partial tear of oropharynx may often mimic the sensation of fish bone present in the throat. In addition, patient can hardly localize the fish bone in the lower two thirds of oesophagus which is poorly innervated. For fish bones that have passed beyond the post-cricoid region, symptoms are felt in the midline, which makes differentiation even more difficult. At present, plain radiographs are taken for many patients with suspected fish bone ingestion. Of 835 patients who had obtained plain radiography in the study, only 28.9% had positive XR findings. The use of radiography to predict the presence of fish bone is therefore unreliable. In fact, many studies had already shown that in many cases of oropharyngeal foreign bodies, imaging studies have no influence on the management except delaying endoscopy.3 Prospective study of suspected fishbone ingestion by Yoshihiro revealed that the sensitivity and specificity of plain X-ray was 54.8% and 100% respectively,4 while our study was 32% and 91.4% respectively. Our study has identified 3 risk factors that predict the likelihood of complications in patients with fish bone ingestion. They are: (1) delayed presentation of >48 hours, (2) positive X-ray and (3) fish bone impacted at the cricopharyngeus. While it is common sense that the longer the fish bone is present, the more likely that complications will ensue. Previous study reported that when the duration of symptoms increased, the yield of fish bone retrieval decreased.5 Among patients who refused admission or OGD in our study, none developed complications in the absence of further treatment. In addition to the low retrieval rate (31.4%) by OGD, We may justly suspect that most of the fish bones would be dislodged and passed through the gastrointestinal tract eventually. While some cases develop complication, most cases do not. There may be some confounding factors (e.g. like the type of fish ingested or size of fish bone) for development of complications among those who present late and further study is needed to establish its association. While use of X-ray and symptoms have been regarded as unreliable diagnostic tools for fish bone ingestion, our study has identified positive X-ray as a predictive risk factor for developing complications following fish bone ingestion. Although X-ray has low sensitivity, its specificity is remarkable (90-100%).3,4 X-ray, when combined with symptoms can be very useful to guide the steps of direct laryngoscopy and OGD. This is because when a fish bone is present, the site of symptom correlates well with the site of impaction in the X-ray. Therefore, endoscopists should start the examination on the affected side, with special attention to the area the patient is pointing at. In addition, plain radiography is highly specific for fish bone impaction. When the radiograph is positive, endoscopists can place a pair of forceps into the working channel of the endoscope before rather than during the examination. This can reduce the discomfort of the patient and prevent inadvertent dislodgement during subsequent insertion of the forceps into the endoscope. This demonstrates that a combination of symptoms and X-ray findings can shorten the time of endoscopy, its difficulty and reduce any morbidity associated with direct laryngoscopy and OGD. Regarding sites of impaction, fish bones impacted in the cricopharyngeus are commonly associated with difficulties. Dislodgment, lengthy procedure, failure and mucosal tear during endoscopic retrieval are not uncommon.5 Difficulty can be anticipated because cricopharyngeus is an anatomical narrowing in the upper gastrointestinal tract. Its identification as a risk factor for complications in our study has given further support to this observation. Therefore, endoscopy in these conditions should be done with tremendous care and it has been recommended that rigid laryngoesophagoscopy under general anaesthesia should be considered once difficulty is encountered.5 The limitation of this study is that it was a retrospective analysis. The validity of the results may be affected by the accuracy of the X-ray findings, symptoms reported in the records or endoscopic findings. In conclusion, patients with the following 3 risk factors are more likely to have complications after fish bone ingestion: (1) delayed presentation of >48 hours, (2) fish bone seen in X-ray and (3) fish bone impacted in the cricopharyngeus. When managing patients with these risk factors, special attention should be paid to identify and treat the potential complications as early as possible. Key messages
Tak-shun Poon, MBBS (HK), MRCS (Edin)
Resident, Cheuk-wai Yuen, MBCHB (CUHK), MRCS (Edin), FHKCEM Medical Officer Specialist, Kam-shing Fung, MBBS (HK), MRCP (UK), FHKCEM Senior Medical Officer, Accident & Emergency Department, Tseung Kwan O Hospital. Correspondence to : Dr Tak-shun Poon, Accident & Emergency Department, Tseung Kwan O Hospital, Tseung Kwan O, Kowloon, Hong Kong.
References
|
|