|
March 2009, Volume 31, No. 1
|
Original Articles
|
Frequent attenders in New Territories West Region: their characteristics and workload implicationM K Cheung 張文娟, Y S Ng 吳楊城, C W Lo 盧卓偉, T C Law 羅冬姿, Cynthia S Y Chan 陳兆儀, J Liang 梁峻 HK Pract 2009;31:14-22 Summary
Objective: To examine the characteristics of frequent attenders
(FA) and their impact on workload in a public primary care setting in Hong Kong.
Keywords: Frequent attenders, characteristics, general outpatient clinic 摘要
目的: 研究經常求診者的特徵及其對香港公營基層醫療工作量的影響。
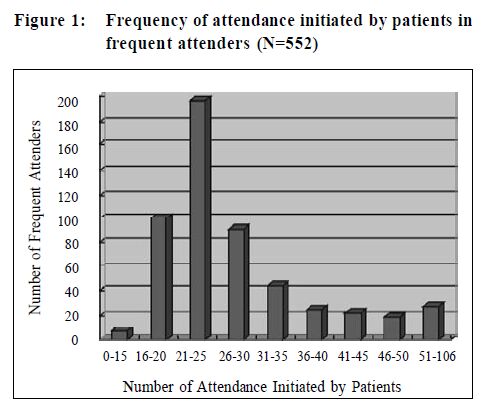
主要詞彙: 經常求診者,特徵,普通科門診。 Background In general practice, it has long been known that a small minority of patients consulted very frequently. This group of patients accounts for a disproportionate number of consultations.1-3 Such patients are referred to as 'frequent attenders' (FAs). There is, as yet, no agreement on the most appropriate method of defining frequent attendance.4 Frequent attenders are variously defined based on a specified number of consultations in a fixed time period (ranging form 5 to 20 in one calendar year);5-6 or a cut-off in the distribution of consultation frequency (for example, the population whose consultation frequency is at the top 3% to 10%).7-9 Frequent attenders consume a large proportion of a general practitioner's workload; one study reported that the top 3% of attenders (in terms of frequency) utilized 15% of a GP's clinical workload.7 Other studies reported that frequent attenders accounted for between one-tenth and one-third of a GP's caseload.9 Certain socio-demographic characteristics of frequent attenders had been identified from previous studies.2,9-12 For instance, females and the elderly were more likely to be frequent attenders.6,9,11 Social class, employment status, and ethnicity had also been linked with frequent attendance.10,12,13 Somatisation, physical and psychiatric morbidity were all important factors in determining frequent attendance.2,14,15 Musculoskeletal, respiratory and digestive disorders were found to be the dominant physical diseases in frequent attenders.16-18 A study found that frequent consultations for those with injuries were considered medically appropriate.19 People with multiple co-morbidities were more likely to see their GPs.20,21 However, these studies were mainly conducted in Western industrialized societies. Some were small studies in discrete geographical locations, whose results may be hard to extrapolate to a wider or different community.9,22 Two local studies in Hong Kong addressing frequent attendance were also limited to a single clinic setting.23,24 In our study, we set out to establish and examine the proportion of frequent attenders who attended the General Outpatient Clinics (GOPCs) of the Hong Kong Hospital Authority New Territories West Cluster (NTWC). We aimed to calculate the proportion of clinical workload generated by these patients, and to identify and characterize such frequent attenders. The null hypothesis was that there was no difference between the characteristics of the frequent attender group and those who were classified as non-frequent attenders. With our findings we hoped to be able to plan our future services to better address the needs of these patients and the disproportional workload generated by them. Methods In March 2007, a retrospective review was conducted in the seven GOPCs in NTWC. NTWC is one of the seven clusters of the Hospital Authority in Hong Kong with a catchment population of around one million. In 2003, these clinics were fully computerized for patient registration, consultation note, prescription and disease registry for each consultation using ICPC (International Classification of Primary Care, second edition). They provided outpatient primary care service to patients with chronic or episodic illnesses. A consultation fee of HK$45 was charged for each entitled patient. This fee was waived in (1) patients on social assistance, (2) those who were government servants, or (3) those who were the serving employees of and entitled subsidiaries of the Hospital Authority. Frequent attenders in our study were defined as patients consulting on more than 20 occasions at GOPCs from March 2006 to Feb 2007. There was no agreement on the most appropriate method of defining frequent attendance, and 20 consultations in a year was the upper limit of frequent attenders in current literature. Only doctor's consultations were included. Visits for non-doctor's activities, such as for dressing or injection were not included. No home visits were provided by the study clinics. Administrative consultations, such as childhood immunization or antenatal care were also excluded. Information including age, gender, marital status, payment status, and the number of doctor's consultations were collected from computerized patient records. A review of individual frequent attender's records was conducted by two investigators. Standard coding sheets were developed and the investigators tried these coding sheets on a pilot number of patients. Outcome measures included demographic data, reason for consultation, and the nature of the problem presented, including sick leave and injury on duty (IOD). Statistical Package for the Social Sciences (SPSS) v15.0 was used for data analysis. Nominal data were analyzed using Pearson's chi-square test. Ordinal data were analyzed using two-tailed t test. Results Workload A total of 552 patients fulfilled the criteria of frequent attenders (FAs), contributing to a total of 15 841 attendances. Since the total number of patients in NTWC GOPCs during the study period was 194 078 and the total number of attendance for the study period was 689 563, FAs constituted 0.28% of patients attending the study clinics, and 2.3% of total attendances in this study period. Among these FAs, two patients attended more than 20 times each. 424 patients attended mainly one single clinic. 126 patients visited two or more clinics, and while their attendance at a single clinic may not be frequent, they had a total attendance of >20 times when adding up all attendances from various clinics. Frequency The overall average number of visits per patient in NTWC GOPCs during the study period was 3.6. The average number of visits for the subgroup of FAs was 29. The average number of visits for the subgroup of non-FAs was 3.5 (Figure 1).
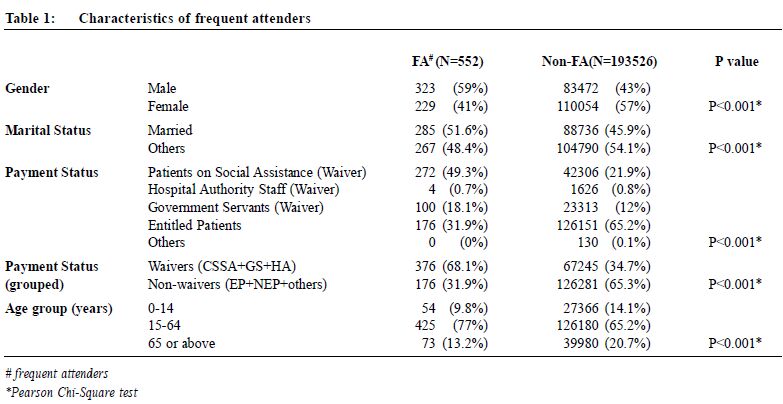
Demographic characteristics of frequent attenders While there was a male predominance in FA, there was a female predominance in non-FA, and this difference was statistically significant (Table 1).
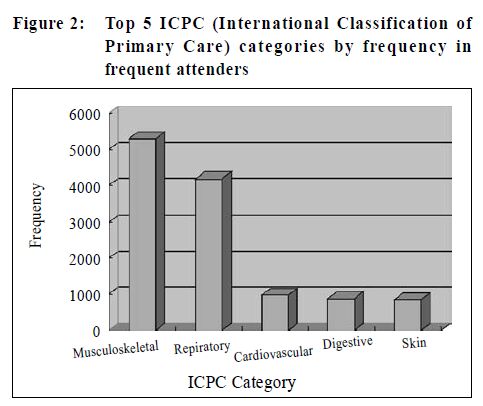
The mean age of FA was 44 years. Dividing patients into paediatrics (0-14 years), young/adult/middle aged (15-65 years) and elderly (>65 years old), there is a young/adult/middle aged predominance for both FAs and non-FAs. However, FAs have a smaller proportion of paediatric and elderly patients, and this difference is statistically significant (Table 1). A total of 68% of FAs were eligible for having their consultation fees waived, this is in contrast to non-FAS who were predominantly paying patients. The difference is statistically significant (Table 1). Presenting symptoms and diagnoses The average number of chief complaints presented by FAs during a consultation was 1.96. The range was from one to nine complaints. 71% of FA presented with more than one complaint. The top five most frequently coded ICPC categories among FAs were musculoskeletal (L), respiratory (R), cardiovascular (K), digestive (D) and skin (S). (Figure 2).
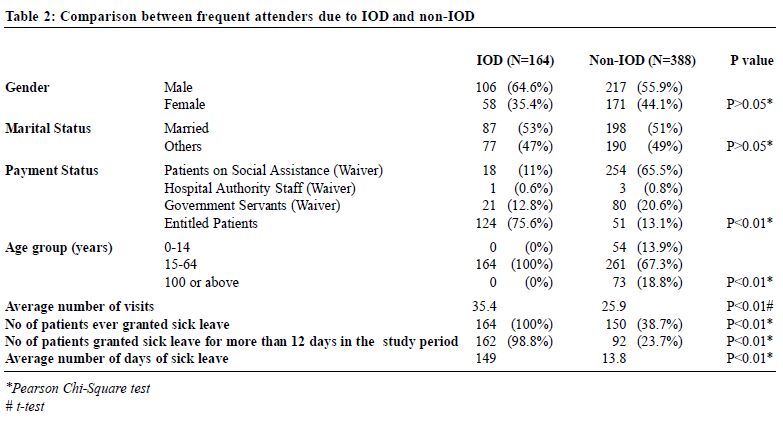
Injury on duty (IOD) vs Non-IOD Among the 522 FAs, 164 attendances were IOD related. Both the IOD group and non-IOD group had a male predominance. None from the IOD group were from the paediatric or elderly group, while only 67.3% of non-IOD group were adults. The difference in age distribution is statistically significant (Table 2). A high proportion of IOD group (75.6%) had to pay for their consultations while the majority of non-IOD group (86.9%) were waivers. This difference is statistically significant (Table 2). The average number of visits by the IOD group and non-IOD was 35.4 and 25.9 respectively, again reaching statistical significance (Table 2).
Issuing of sick leave 314 FAs were issued with sick leave during the study period. Among them, 164 patients were for IOD, 150 patients were for other reasons. 254 patients were given more than 12 days of sick leave. Among these, 162 patients were for IOD, and 92 patients were for non-IOD problems. The average duration of sick leave in the IOD group was statistically significantly longer than in non-IOD group (149.02 days vs. 13.79 days respectively P<0.01) (Table 2). Discussion Workload implication Although frequent attenders only constituted 0.28% of patients in the study period, they contributed to 2.3% of the total attendance. That is, they generated 8.2 times more workload to the clinics than average. This is indeed a significant proportion, and our findings are consistent with the findings of previous studies.9 Characteristics of frequent attenders FA in our study were mainly males, married and middle aged. Their main presentation was musculoskeletal problems. Many of them were on social assistance. We could not find any Western studies looking specifically into the issue of IOD. The inclusion of such group will give a more comprehensive picture, while the exclusion of this group will eliminate the influence exerted by this particular subgroup of FAs. When only non-IOD FAs were considered, male, adult and married FA still predominated. The proportion of patients on social assistance was even higher in non-IOD FAs. These findings are different from those in studies conducted in Western countries in which the majority of FAs were females, single and elderly.7,10,12,25 We believe that such differences are due to a number of factors as discussed below. 1. Disease factors Chronic back pain affecting work and associated IODs are known to be difficult management problems.19 Since these are mainly working-aged males, this may explain why middle-aged males predominated in our study. Previous studies26-30 showed that underlying psychosocial problems were a major contributing factor for frequent attendance. However, psychosocial problems were not prominent in our study. In the other two local studies,24,31 the major diagnoses were also physical illnesses. We speculate that the reason for this phenomenon could be because psychosocial problems may present as somatic complaints, and the busy GOPC doctor may only have time to deal with the physical complaints, without exploring the more complex underlying psychosocial problems. Patients with injury on duty are also common. The most frequent attender had 106 clinic visits in the study year. Indeed, a large proportion of frequent attenders were patients wanting prolonged sick leave, or frequent refill of medications. Some patients frequently visit GOPCs for minor ailments and medications for symptomatic relief. This could be that they do not have adequate knowledge of their symptoms and the appropriate management. Such patients may benefit from efforts to bridge their knowledge gap. 2. Financial factors In Hong Kong, patients attending GOPC are heavily subsidized. If the patient is on social assistance, the token fee is waived. On the other hand, a patient may need to pay several hundred to several thousand dollars per visit if he consults a private doctor. Accident and Emergency Department could be an alternative, but patients now need to pay HK$100 per A&E visit and need to wait for a longer time if their condition is non-urgent. Therefore, patients with frequent attendance may find GOPC an inexpensive location for a consultation. Indeed, half of FAs in our study were on social assistance. Seeking free or relatively inexpensive GOPC service may be the only method of help that they know of, have access to or can afford. 3. System factors at GOPCs In the GOPCs studied, a doctor has to see 84 patients a day. The contact time allowed for each patient is short and the time pressure on the doctor is huge. The doctors may have little time to further explore and then manage the underlying reasons for the frequent attendance. A continuation of symptomatic relief treatment and extension of sick leave may seem to be a more effective option to some of the doctors under this situation. Moreover, most GOPC doctors have to work "on shift" nowadays. That is, on top of day time clinic duties, they need to share evening clinic, Sunday clinic and public holiday clinic duties. Therefore, patients may see different doctors on GOPC visits. As a result, doctor's effort to continuously manage a patient's psychosocial problems may be inadequate. What can be done to help? Several attempts have been made to tackle frequent attendance, and the outcomes are variable. A British study showed that although frequent attenders often have multiple problems, prominently displayed summaries of their history for use by doctors during consultation do not reduce the frequency of consutation.32 An Israeli team set up a multidisciplinary clinic which involved family physicians with training in psychotherapy, senior psychiatrist and medical social workers. They reported that such interventions helped to modify illness behaviour, decreasing costs of medical investigations.27 How one should determine need as compared to demand of consultations is a challenging issue. There is also a possibility that frequent consultations in primary care might have saved more expensive specialist consultations and hospital admissions. Therefore, more detailed assessment of frequent attenders is needed in order to identify potentially modifiable factors contributing to frequent attendance, and to initiate appropriate intervention. A change in the healthcare system, in the setting of GOPC, in the doctor's and patient's behaviour is needed to address the issue of frequent attendance. Specific measures should be developed according to the characteristics and health needs of frequent attenders in the locality. Our study has a number of limitations. Firstly, medical records were used retrospectively for data collection. However, since details of patient's demographic data, consultation, investigations and final diagnosis are generally well recorded in our computer system, we believe that this is not a big problem. Secondly, we used 20 consultations within a year as a cut-off threshold. While this ensures that we isolated a group that was definitely frequent attenders, the characteristics of this group of patients may be different from those in studies which have a lower threshold. Thirdly, as we mainly studied frequent attenders in a public primary care setting in the northwestern region of Hong Kong, the findings cannot be generalized to other primary care settings in other regions. However, the analysis of our FA data is comprehensive, as we included FAs who attended more than one clinic in the same cluster. Conclusion In this study, we found that frequent attenders consumed a 8.2-fold increase in the number of consultations than average. They were mainly middle-aged married males with musculoskeletal problems. IODs were a major reason for the frequent visits. This finding is different from those in Western countries. A number of possible reasons were put forward for this phenomenon. Our study is by far the largest study looking at frequent attendance in the public primary care setting in Hong Kong, but it is only the start of a process to find out and, if possible, modify factors that will influence the use of resources. In response to our findings, we are planning to set up special clinics to provide more comprehensive assessment and intervention for this group of patients. Future directions may also include qualitative studies to seek the reasons behind frequent consultations to establish if the interventions are appropriately targeted. Key messages
M K Cheung, FHKCFP, FHKAM (Family Medicine)
Associate Consultant, Y S Ng, FHKCFP, FHKAM (Family Medicine) Associate Consultant, CW Lo, MBChB Medical Officer, J Liang, FHKCFP, FHKAM (Family Medicine) Consultant Department of Family Medicine, New Territory West Cluster, Hospital Authority. T C Law, FHKCFP FHKAM (Family Medicine) Resident Specialist, Department of Family Medicine, Kowloon Central Cluster, Hospital Authority. Cynthia S Y Chan, LMCHK, MD (Canada), FHKAM (Family Medicine), FRACGP Specialist in Family Medicine Correspondence to : Dr M K Cheung, Yan Oi General Outpatient Clinic, G/F, 6 Tuen Lee Street, Tun Mun, NT, Hong Kong SAR. Email: cheungmk1@ha.org.hk
References
|
|