|
March 2009, Volume 31, No. 1
|
Original Articles
|
The Family Medicine Specialist Surgical Clinic - a new project to benefit the patient, hospital specialist, family physicians and the private sector in the communityKin-wai Chan 陳建偉, Peter T K Ng 吳子敬, Ching Chan 陳貞, Ching-luen Ng 吳清聯, Yuk-kwan Yiu 姚玉筠 HK Pract 2009,31:24-29 Summary
Objective: To study the outcome of the Family Medicine Specialist
Surgical Clinic (FMSC) at the Ha Kwai Chung GOPC in addressing the problem of long
waiting time of the Specialist Out-patient Department Surgical Unit.
Keywords: Family medicine specialist clinic, surgery, endoscopy, haemorrhoid rubber band ligation 摘要
目的: 在下葵涌GOPC內設立家庭醫學專家外科門診(FMSC),以縮短專科門診SOPD病人的等候時間。
主要詞彙: 家庭醫學專家門診,外科,內窺鏡檢查,痔瘡,皮圈套扎。 Introduction Heavy workload and a long waiting time have always been a problem for the Hong Kong Government Hospital Authority's Specialist Outpatient Department (SOPD), especially its surgical unit, in Hong Kong's public health sector. In May 2006, the median waiting time for a first appointment for non-urgent cases in the various specialty units of the SOPD was more than 30 weeks. For the surgery unit at the SOPD, the waiting time was 34 weeks.1 The worst situation was noted in the case of its gastro-intestinal (GI) team, whose waiting was 134 weeks. In response to this situation, the Department of Family Medicine at the Kowloon West Cluster of the Hospital Authority and the Department of Surgery at the Princess Margaret Hospital piloted a Family Medicine Specialist Surgical Clinic (FMSC) in Ha Kwai Chung General Outpatient Clinic (GOPC) in August 2007 to address the issue. Patients having upper or lower gastro-intestinal (GI) symptoms and referred to the Princess Margaret Hospital Surgical SOPD were screened by two surgical consultants of the hospital. Cases that belonged to Category 3 (non-urgent referrals), which had an average waiting time of 129 weeks, were triaged to the Family Medicine Specialist Surgery Clinic and were managed by family physicians. The main purpose of the FMSC was to reduce the number of patients presenting with upper and lower GI symptoms referred to the Surgical SOPD at the local public hospital. To fulfill this role, the FMSC had access to specialised equipments and expertise to handle simple office investigations and interventions, e.g. the rigid and flexible sigmoidoscopes, as well as to do haemorrhoid rubber band ligation. The FMSC also had special arrangements with the public hospital to be allowed direct access to certain investigations such as oesophageogastroduodenoscopy (OGD), ultrasound scan (USG) and Barium (Ba) enema examinations. In the FMSC, patients can also have the option to be referred to the outside private sector for earlier investigations. Objectives In this study, we set out to analyze the outcome of the patients managed in the Family Medicine Specialist Surgical Clinic (FMSC) and find out the effectiveness of this FMSC model:
Methodology A cross-sectional study on:
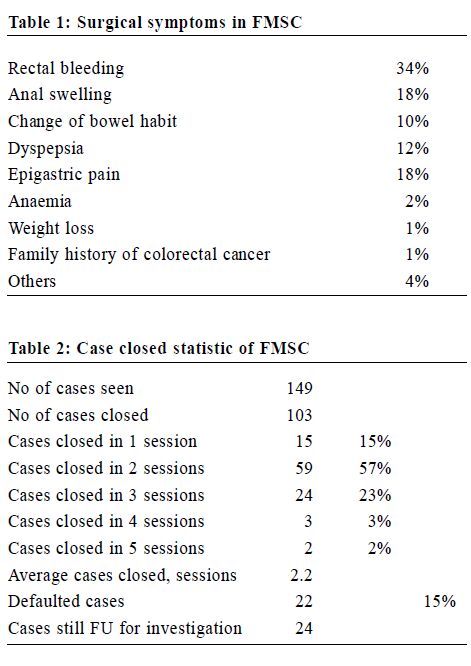
Patient outcome and satisfaction of the patients were analyzed by electronic patient records review and questionnaires respectively. (See Appendix 1) Results 1) From Aug 2007 to Jan 2008, 160 patients were triaged to the FMSC. 11 patients (7%) defaulted the first appointment and 149 patients (93%) were managed in the FMSC clinic. The average waiting time of the FMSC was around 4 weeks. 48 cases presented with upper GI symptoms, 97 cases with lower GI symptoms and 4 cases with both upper and lower GI symptoms. (Table 1 & Table 2)
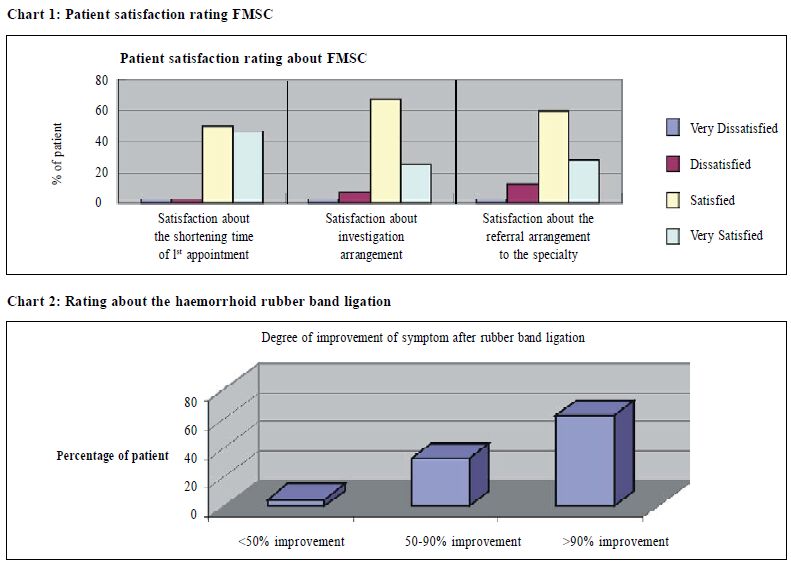
2) 83.2 % of patients were managed by the FMSC without need for a SOPD referral. The most common problems that patients had were per rectal bleeding, haemorrhoid and dyspepsia. For patients who presented with fresh rectal bleeding, rigid or flexible sigmoidoscopy was performed to rule out distal lower GI malignancy. We also performed rubber band ligation on 50 suitable haemorrhoid cases. 3) Cases suspicious of malignancy were referred to the hospital specialist in the public or private sector for colonoscopy, Ba enema or ultrasound investigations. All patients needing referrals to SOPD were offered the option of investigations in the private or the public sector. A total of 79 investigations were performed, of which 35 (44%) were done in the public sector and 44 (56%) cases in the private sector. Of those with upper GI symptoms, 35% of patients chose to have investigations in the public sector. Of those with lower GI symptoms, 13% opted for public. 4) 3 colorectal cancers and 5 neoplastic polyps were detected. Other surgical lesions like big or external haemorrhoids were also detected which were not suitable for curative treatment in the FMSC clinic. These cases made up 16.8 % of total patients, requiring referrals to the hospital specialist for further management. 5) 103 cases (69%) could be closed in the FMSC clinic after an average of 2.2 consultations. Among these, 49 (33%) were followed up by the community general out-patients or private clinics after case closed. 22 cases in FMSC defaulted follow up and 24 cases were still being followed up in the FMSC mainly because of the long waiting time for investigation to be done in the public sector. A questionnaire was performed to survey the patients' satisfaction about the FMSC in terms of shortening of waiting time, arrangement of private investigations, referral for secondary care, and procedure performance such as haemorrhoid rubber band ligation.(Chart 1 & Chart 2) The questionnaires survey was performed via telephone in March 2008. 61 patients replied with a 41% response rate.
Discussion Owing to escalating public demand, the traditional referral method for surgical illness has overloaded the public surgical Specialist Outpatient Department (Diagram 1), resulting in a long waiting time for surgical outpatient appointments for those with non-urgent surgical conditions. The FMSC demonstrated a new model of referral: a bi-directional referral pattern (Diagram 2). The FMSC coordinated across the boundary partnership between primary and secondary health-care system as well as resources from the public and private sectors.
In developed countries like USA and UK, family physicians with special interest often perform endoscopy in the hospital or even in their offices. This results in an increase in patient satisfaction because patients can and often prefer to stay with their own family physicians. The doctor-patient relationship is strengthened and the patients gain more confidence with their family physicians.2 The FMSC can perform simple investigation procedures e.g. OGD, rigid or flexible sigmoidoscopy, and simple interventions e.g. haemorrhoid rubber band ligation, polypectomy and lesion biopsy. This will enhance the role of FMSC as a good gate keeper in the management and investigation of simple surgical diseases. For cases that require further investigations e.g. USG, colonoscopy or Ba enema, the FMSC could provide alternatives for the patient to choose from between obtaining investigations sooner in the private sector or through referral to the public sector if there were financial constraints. The investigation rate in the public sector was found to be quite reasonable: upper GI investigation rate was 35%, compared with the previously published result of 38.7% and 60% respectively in 2005 & 2007 in the Hong Kong Practitioner.3,4 The lower GI investigation rate for those using public resources was even lower (13%). This reinforces the belief that FMSC was a good platform for a public-private interface in terms of investigation and secondary care. The FMSC also has an important role in maintaining continuity of patient care. For patients who have completed all the relevant investigations and/or treatment, the FMSC would then refer them back to the community level, either public or private, for continuing follow up and monitoring of their progress. Three cases of cancer and five of neoplastic polyps were detected during the study period. This finding showed that even when cases were triaged as Category 3 (non urgent), some important diseases could still be missed using the traditional triage system. The FMSC had an important role as a safety net in the early detection of such cases. The affected patients would then be referred to the relevant specialty for early treatment, instead of having to wait for the normal hospital surgical Specialist Outpatient Clinic appointment. To assure diagnostic accuracy and procedural safety (such as endoscopy), proper training is mandatory. Our FMSC clinic was staffed by senior family medicine doctors who have had previous surgical experience. For example, they would have had experience in the surgical specialty and had performed at least 50 rigid sigmoidoscopies under supervision before they were deemed capable of managing a patient independently. For other flexible endoscopic procedures, we had a session for endoscopy (OGD and flexible sigmoidoscopy) training per week in the hospital. The procedures were performed by family medicine doctors under the supervision of surgical specialists. In the case of any important suspicious findings detected during the procedure, the hospital surgeon would take over the case and transfer him/her directly to the surgical ward or clinic for the start of early intervention. To generalize this model to the whole family medicine specialty, support from the Hong Kong College of Family Physicians can be made through collaboration with other specialties (e.g. the Hong Kong College of Surgeons) in designing a training certificate or diploma programme, concentrating on the management of common surgical diseases encountered in primary care, and endoscopic procedures that can be performed in the community. Conclusion The FMSC clinic can benefit patients by providing a safety net for the early diagnosis of malignant and pre-malignant disease. It can also relieve the hospital specialists' workload, enhance family physician's role in performing surgical endoscopy and treatment procedures as well as providing a platform in promoting public/private partnership. If health-care policy makers can consider generalizing this model of service into different specialties, family medicine doctors can play an important role in the Health-care Reform. They can provide a good coordinated interface between primary and secondary health-care as well as between the private and the public sectors. Key messages
Appendix 1
Kin-wai Chan, MBChB (CUHK), MRCS (Edin), FRACGP, FHKCFP
Medical Officer, Ching Chan, BN, MBA Advance Practice Nurse, Ching-luen Ng, MBBS(HK), FRACGP, FHKCFP, FHKAM (Family Medicine) Associate Consultant, Yuk-kwan Yiu, MBBS (HK), FRACGP, FHKCFP, FHKAM (Family Medicine) Chief of Service Department of Family Medicine & Primary Health Care, Kowloon West Cluster, Hospital Authority. Peter T K Ng, MBBS (HK), MFM (Clin) (Monash), DPD (Wales) Medical Officer, General Outpatient Clinic, Kwong Wah Hospital. Correspondence to : Dr Kin-wai Chan, Cheung Sha Wan General Outpatient Clinic, Cheung Sha Wan, Kowloon, Hong Kong SAR.
References
|
|