June 2010, Vol 32, No. 2 |
Original Articles
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Geriatric patients with minimal head injury-should we have a different approach?Ronnie Chi-wing Lo羅志榮, Man-ho Ng吳民豪 HK Pract 2010;32:67-74 Summary Objective: To review the outcome of current practice on geriatric patients with minimal head injury and to identify risk factors for significant brain injury. Design: Retrospective review. Subjects: Elderly patients aged 65 years or older with minimal head injury presented to an emergency department of a district hospital over a 1-year period. Main outcome measures: Initial management, patients’flow and adverse outcomes were accounted. Risk factors for significant intracrainial injuries were analyzed. Results: A total of 267 patients consisted of 289 episodes were included. 4 cases out of 54 CTs performed resulted in significant intracranial injures. No head injury related death was recorded. Only one required neurosurgical intervention. 127 skull X rays performed revealed no definite fracture. 144 episodes employed neurological observation, only 2 reported neurological deterioration which were non-neurosurgical. Extreme age, ill pre-morbid health, lower pre-morbid GCS, and significant visible external injuries, had stronger associations with significant brain injuries. Conclusion: The risk of intracranial injury for elderly patients with minimal head injury, although small, is still much higher than the younger counterparts. Those regarded as high risk should be evaluated with CT brain scans after initial assessment, whereas those with low risk could be safely discharged. Keywords: Minimal head injury, geriatric patients, CT brain scan, neurological observation, significant brain injury 摘要 目的:探討目前頭部受輕度創傷老年病人的治療習慣,辨別導致腦部損傷的因素。 設計:回顧式調查。 對象:一所地區醫院急症室在一年以來因頭部受輕度創傷就診的六十五歲或以上老年病人。 主要測量內容:初步治療,病人診療流程和不利結果。分析嚴重顱內受傷的相關因素。 結果:共計267名病人就診289次。在54次電腦掃描中,4次顯示嚴重顱內受傷。沒有因頭部受傷導致死亡的記錄,只有一例需要接受神經外科手術。在127張頭顱X光片中,沒有明確的骨折報告。在144次神經系統觀察中,只有2人在觀察期內惡化,原因與腦神經問題無關。高齡、健康狀況欠佳、受傷前格拉斯哥昏迷指數較低及明顯外傷,與嚴重腦部損傷有較強關連。 結論:因輕度頭部受傷而導致嚴重顱內傷害的老年病人之危險性雖低,仍遠高於年輕者。高危病人經初步治療後應接受腦部電腦掃描,而低危者則可安心出院。 主要詞彙:頭部輕度受傷,老年病人,腦部電腦掃描,神經觀察,嚴重腦部受傷 Introduction Head injury in the elderly is commonly encountered in our daily practice. In 2006, every 1 in 8 persons in Hong Kong was 65 years or older.1 The vast majority of head injuries present with initial benign presentation with apparent trivial mechanism. Such minimal head injury (MHI), is characterized with no change in conscious level, vomiting, amnesia, seizure or neurological deficit.2, 3 This type of injury is not without risk when occurring in the elderly. Increasing age is clearly associated with a higher risk of intracranial pathology.3-20 The geriatric brain is more susceptible to injury, following physiological changes in ageing including the increased space between brain and skull.18 The risk of shearing and tearing of bridging vessels is increased. More space for accumulation of blood is allowed without increasing intracranial pressure (ICP), hence the classical symptoms may not be present. Moreover, elderly people have higher incidence of syncope and falls that can lead to trauma to the head.19 They also more often have underlying medical conditions resulting in diminished cardiopulmonary reserve, further contributing to an adverse outcome.21 Despite the high incidence of MHI in the elderly and potential risks of significant brain injuries, there is currently no standardized guideline in managing these patients. The initial management, including the use of computer tomography (CT) brain scan, skull X-ray (SXR), neurological observation, and timing of discharge, varies from physician to physician, and from hospital to hospital. Existing studies3, 4, 14, 17, 20 and guidelines5, 7-12, 22 only concentrate on minor or mild head injuries, which are based on the general population, patients presenting with a score of 13 or 14 on the Glasgow Coma Scale (GCS), and those with GCS 15 with some degree of loss of conscious or amnesia. None specifically looks into minimal head injuries in the geriatric subset of patients. We conducted a retrospective study of elderly patients with MHI presenting to an emergency department. The objectives were: first, to review the outcome of current practice on geriatric patients with MHI, in particular looking into the usefulness of immediate CT brain scan and neurological observation; and second, to identify risk factors for significant brain injury which necessitate immediate CT brain scan. Methods A retrospective study was conducted by reviewing the medical records of elderly patients who presented to a district accident and emergency department (AED) over a one year period. The AED serves a population of over 400,000 with an annual attendance of around 100,000 patients. All patients, aged 65 or above, with MHI of less than 6 hours of onset, without coagulopathy and intoxication, presenting to our AED from 1st January 2006 to 31st December 2006 were included. MHI was defined as:
Coagulopathy was defined as:
Intoxication was defined as:
Patients were excluded when their head injury was more than just minimal, or presented after six hours of onset, on anticoagulation treatment, intoxicated, and those with records poorly documented or illegible medical notes. Medical records for all head injury cases were retrieved by using the Hospital Authority’s (HA) Clinical Data Analysis and Reporting System (CDARS). Records having the following ICD-9 diagnosis codes were included:
Such comprehensive entries aimed at maximizing the retrieval of head injury cases. All retrieved cases were subjected to review for inclusion or exclusion under the HA’s Electronic Patient Record (ePR) system, including their AED charts, laboratory and radiological findings, observation ward notes, and discharge summaries for admitted cases. The medical notes of all deaths and re-attendance within 30 days after head injury within all HA hospitals were also reviewed. Re-attendance not related to head injury was excluded. These patients, after their initial assessment with or without SXR, either received immediate plain CT brain scans, were put on neurological observation, or were discharged immediately with post-injury advice given. Allocation of patients into any of the above 3 groups was purely at the discretion of the attending physicians. Based on normal routine, when patients were put on neurological observation, their GCS, pupil status, limb power and sensation, and general status were documented hourly for 4 to 6 hours, with or without extended observation 4-hourly for further 12 to 24 hours. Patients with deterioration of the above parameters during the observation period were subjected to CT brain scans. When patients were discharged, they (and their accompanying persons) were advised to return when they experienced signs of increasing ICP such as impaired consciousness or cognition, repeated vomiting, seizure, and limb weakness. Data on initial management (including CT brain scans, SXR and neurological observations), patients' flow or disposal, and adverse outcomes were collected. Adverse outcomes included the rate of significant intracranial injury, mortality within 30 days (both head injury and non-head injury related), head injury related re-attendance within 30 days, the need for neurosurgical intervention (such as craniotomy and burr hole), and the need for intubation. For risk factor analysis, the clinical variables between those with and those without significant brain injuries were compared, including age, sex, pre-morbid activity of daily living (ADL)a, triage category, past major illnessb, mobilityc, use of PAI, significant visible external injuriesd, pre-morbid GCS, and mechanism of head injury. Significant brain injury was defined as significant abnormality on a positive CT scan. Positive CT scan was one that demonstrated an acute pathological state in the skull or brain attributable to head injury,23 including vault or basilar fractures, epidural, subdural, intracerebral haematomas, contusions, intraventricular haemorrhage, and pneumocephalus. Facial fractures and extracranial soft tissue injuries were excluded. CT abnormalities were considered insignificant7 when i) solitary contusion less than 5mm in diameter, ii) localized subarachnoid blood less than 1mm thick, iii) smear subdural haematoma less than 4mm thick, iv) isolated pneumocephaly, and v) closed depressed skull fracture not through the inner table. Chi-square test and 1-sided Fisher’s exact test, SPSS 12 for Windows, were used for statistical analysis.
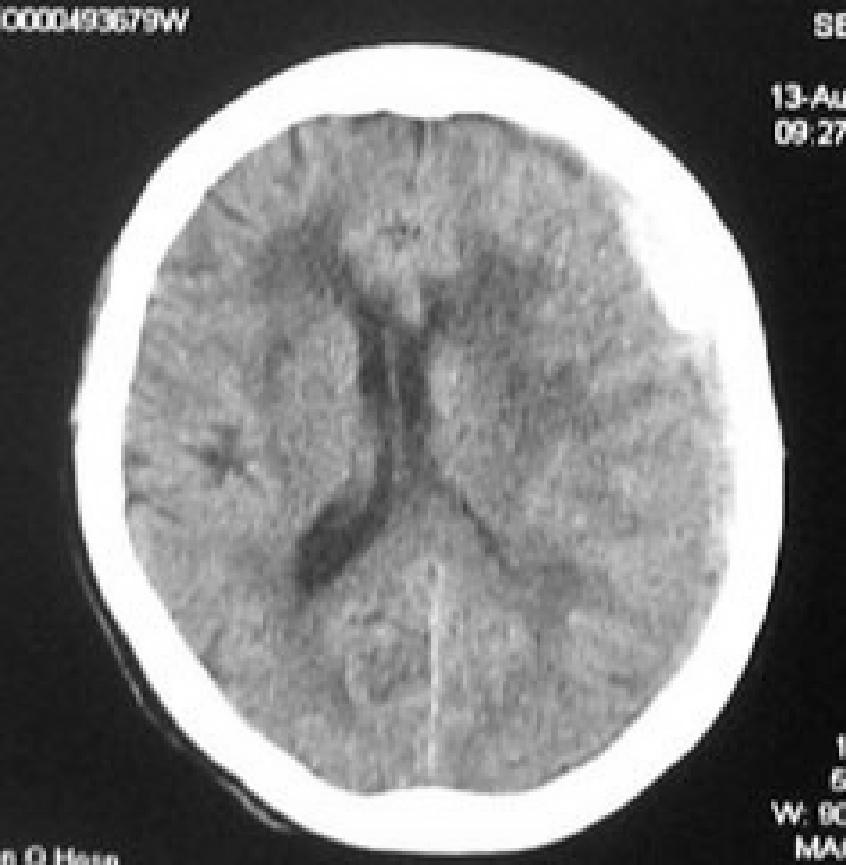
Results Over the 1-year study period, 267 patients were included, accounting for 289 AED attendances (16 patients had 2 to 4 episodes of MHI within the 1-year period). 42 received immediate CT brain scans; 123 were initially neurologically observed (including 9 admitted to other wards due to concurrent illnesses with neurological observation continued), and 124 were discharged shortly after initial assessment. 127 SXRs were performed. No definite fractures were reported, but 3 were reported as suspicious. These 3 were proven negative on subsequent CT brain scans. 54 CT brain scans in total were performed. 42 were performed immediately, with 4 cases showing significant brain injuries. 8 were performed during neurological observation and 4 during re-attendance, none of which reported brain injury. The overall positive CT rate was 7.4%. Neurological observation was employed in 144 episodes, including 123 receiving initial neurological observation and 21 after an immediate CT with negative findings. 8 CTs for those receiving initial neurological observation did not demonstrate any brain injury. Altogether 2 reported neurological deterioration of non-neurosurgical causes. Excluding the 19 immediately admitted cases, 118 out of 125 cases (94.4%) could be discharged from the observation ward, with the mean AED stay of 13 hours. 7 cases were transferred from the observation ward to the medical wards due to concurrent medical conditions, namely confusion (n=2), atrial fibrillation (n=1), anaemia (n=2), hypoglycaemia (n=1), and worsening of renal failure (n=1). In terms of adverse outcomes, 4 cases sustained significant brain injuries, only one with left subdural haemorrhage requiring burr hole drainage (Figure 1, Table 1). None required intubation. 6 deaths occurred within 30 days, none of which were related to head injury. The causes of deaths included terminal cancer (n=2), cerebral vascular event (n=2), ischaemic heart disease (n=1) and suicide (n=1). 6 head-injury related re-attendance within 30 days were relatively minor, including post-concussion syndrome (n=4), gaped wound (n=1), and more apparent periorbital bruising (n=1). The clinical variables of the above 4 cases with significant brain injuries were compared with those without significant brain injuries (Table 2). Age 85 or above, pre-morbid GCS 13 or lower, and significant visible external injuries had strong associations with a significant brain injury. At least 2 of such 3 variables were present in these 4 cases. Suffering at least three major medical illnesses tend to contribute to significant brain injury, but was marginally short from being statistically significant. Those determined to be of triage category 3 or above, dependent in terms of activities of daily living, and poor mobility showed weak association with significant brain injury. No association was noted between significant brain injury and gender, use of PAI, and mechanism of injury. Figure 1: Images showing significant brain injuries (left: left subdural haematoma required operation, right: right cerebral contusion managed conservatively)
Table 1: Summary of clinical variables and outcomes of the significant brain injury cases
Legend: PMI - past medical illness (number indicates the number of major medical illness), ADL - activity of daily living, PD - partial dependent, I - independent, D - dependent, PAI - platelet aggregating inhibitor, GCS - premorbid Glasgow coma scale, Mech - mechanism, lac - laceration, (Y) - significant visible external injury, (N) - insignificant visible external injury, SDH - subdural haemorrhage, MLS - midline shift, NS OT- neurosurgical operation, Rehab - rehabilitation, Med - medical, Surg - surgical, rpt - repeat, F/U - follow-up, OPD - out-patient department (please kindly tidy up those underlined in red into one line) Table 2: Odd ratios of the clinical variables
Discussion Although MHI is commonly encountered in the elderly, there is no agreed guideline specifically addressing its management. Elderly with MHI can have significant pathology with a deceptive benign presentation and completely normal physical examination.13,24 Talked and deteriorated after head trauma is not uncommon and the outcome is particularly poor in the elderly.15,16 From our study, 4 out of 289 episodes presented with an apparent MHI ended up in significant brain injuries. Although the rate for significant brain injury was low (1.4%), such a rate was still much higher than young adult counterparts. Fabbri et al.20 had shown that only 1 out of 1676 MHI patients below 60 years had intracranial lesions (0.06%). Elderly with MHI is therefore not without risk and should be more cautiously managed. If local current guidelines for MHI were applied,22 which suggested that patients could be safely discharged after initial assessments, these 4 patients would be missed. The same result would occur if the NICE (National Institute of Clinical Excellence) recommendation5 was applied, which suggested that patients with one of the risk factors (age 65 or above, coagulopathy, or dangerous mechanism of injury) should at least have had an instance of loss of consciousness or amnesia, before receiving CT brain scans. Therefore, the threshold for having CT for elderly patients with MHI should be lower. There have already been a number of rules for CT9-12 which regarded old age as one of the risk factors for considering a CT in the setting of mild head injury. Whether such consideration should be extended to MHI is still debatable. The overall adverse outcomes in this study are relatively minor, despite the fact that the MHI subgroup is more prone to have severe brain injury with poor outcomes. No head-injury related 30-day mortality and significant 30-day morbidity were reported. Despite the fact that 4 cases resulted in significant brain injuries (positive CT rate of 7.4%, overall significant brain injury rate of 1.4%), only one required neurosurgical intervention (0.35%). This is comparable to many studies on mild head injury, in which neurosurgical interventions were required in 0.3 to 7% despite CT abnormalities in 6.5 to 38.9%.9-12, 17, 20, 23, 25 Stronger associations for significant brain injuries were demonstrated in 4 variables, namely extreme age, ill pre-morbid health, more apparent external injuries, and lower pre-morbid GCS. At least 2 of such variables were present in those significantly brain injured patients. More serious consideration for offering CT brain scans should be given to those patients with more than one of any of such 4 risk factors present. Contrary to our belief, the use of PAI was not shown to be a risk factor for brain injury. Studies on risk of significant brain injuries with PAI use had been inconclusive.26, 27 SXR were of no additional value in terms of screening or assisting in making diagnosis for significant brain injury. None of the SXRs revealed definite skull fracture. Those with significant brain injuries did not require SXR. Many studies or guidelines3, 5, 7, 8, 23, 25 already disregarded its use. The majority of patients with skull fractures did not develop complications and intracranial bleeding was not necessarily associated with skull fracture.3 The value of neurological observation is doubtful in terms of detecting significant brain injuries. No delayed intracranial injuries were detected whenever patients stayed in observation ward, being admitted, put on observation after normal initial CT finding, or received delay CT after a certain period of observation. In fact, observation ward stay is more useful in discovering underlying illness that may contribute to head injury. Out of the 125 observation ward cases, 7 required medical admissions due to concurrent medical illnesses, including 2 who deteriorated neurologically. 94.4% could be discharged with an average AED stay of 13 hours. If these patients were discharged immediately after initial assessment, with the assumption that the observation ward stay occupied three quarters of the total AED stay, up to 1150 working hours could be saved without harmful effect. Delayed intracranial haemorrhage after normal initial CT brains scans was extremely rare23, 28-33 and hospital admissions for neurological observation after normal initial CT brain scans were proven useless.28-31 The use of CT brain scan as a triage tool for admission was safe32, 33 and cost effective.34-36 Moreover neurological observation was labour intensive when properly performed as recommended in the NICE guidelines.5 Livingston et al.30 showed that less than half of the patients with mild head injuries admitted had proper documentation of neurological observations, and the frequency of observations was insufficient to detect early neurological deterioration from 1 to 8 hours after injury. Furthermore, delayed presentation of intracranial haemorrhage in elderly patients with MHI usually occurs after weeks rather than hours after initial injury.37-39 Short stay neurological observation, practically for 4 to 24 hours, probably adds little value in brain injury detection. In order to improve diagnostic efficacy and better utilize resources for patients presenting with MHI, immediate CT brain scans for high risk cases might be the future direction. The functions of neurological observation and SXR are doubtful in stratifying the risk of significant brain injuries. Observation ward stay seems only useful in detecting concurrent illnesses that might have precipitated the head injury. In order to evaluate the risk of significant brain injuries, a scoring system based on the previously mentioned risk factors should be constructed. Risk factors having stronger associations with significant brain injury can be put on a heavier weighting. CT brain scans should only be recommended if a certain score is achieved. This can potentially save a large amount of observation hours as well as X-rays in return for a small increase in CT brain scans utilization, hence saving overall costs. Those regarded as low risk, which represent the majority, can be safely discharged after careful initial assessments without any imaging. Therefore the majority of elderly patients with MHI can be manageable in the primary care setting. The key for managing these patients is to identify the high risk group requiring hospital care and definitive neuroimaging. In this study, extreme age, ill pre-morbid health, more apparent external injuries, and lower pre-morbid GCS were associated with higher risks. However, risk factor determination required validation of all clinical variables with larger scale prospective studies and in different settings. Undiagnosed intracranial injuries should be kept to minimum. Limitations Our study had several limitations. The retrospective design might result in missing data in the study variables. The small sample size, especially the number of cases with significant brain injuries, made the statistical analysis of risk factors less reliable. This can only be improved with a longer study period, or conducting a multi-centre trial. Cases could be missed if diagnoses were not entered or inappropriately entered. A few potential cases were excluded just because of poor documentation. Head injury related re-attendance, hence late adverse outcome, could be missed if patients seek medical attention in the private sector for neurological deterioration. The choice of management could be biased, such that different physicians might have different beliefs and might handle similar scenarios differently. Conclusion The risk of intracranial injury for elderly patients presenting with minimal head injury, although small, is still much higher than their younger counterparts and can easily be overlooked. Conventional management for this subgroup of patients may miss significant brain injuries, the number of which may not be small. More liberal use of CT brain scans should be considered if the patients are regarded as high risk after initial assessments. Conversely, those regarded as low risk can be safely discharged without any imaging or observation. Key messages
Ronnie Chi-wing Lo, MBBS (Syd), MRCS (Edin) Man-ho Ng, MBBS (HK), FACEM, FHKCEM, FHKAM (Emergency Medicine) Correspondence to: Dr Ronnie Lo, Accident and Emergency Department, Tseung Kwan O Hospital, Tseung Kwan O, NT, Hong Kong SAR. References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||