|
December 2011, Volume 33, No. 4
|
Original Articles
|
Translation and validation of the COPD Self-Efficacy Scale (CSES) into Chinese version (CSES-Chi)Lap-kin Chiang 蔣立建, Lorna V Ng 吳蓮蓮, Lawrence Fung 馮振威, Raymond Tang 鄧禮文, Wilson WS Tam 談維新 HK Pract 2011;33:139-145 Summary
Objective: To translate and validate a language relevant tool for
evaluating the self-efficacy of Chinese speaking patients suffering from Chronic
Obstructive Pulmonary Disease (COPD) in Hong Kong.
Keywords: Chronic obstructive pulmonary disease, Self-efficacy scale, translation and validation, primary care 摘要
目的: 翻譯和驗證適合香港華人的慢性阻塞性肺病患者自 我效能評估的工具。
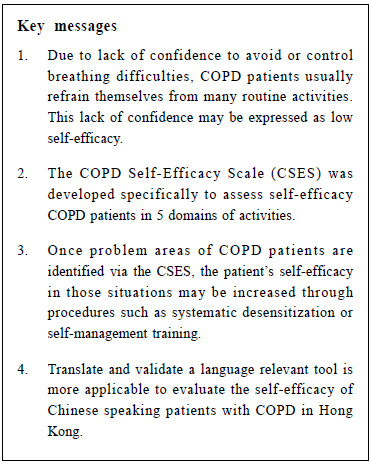
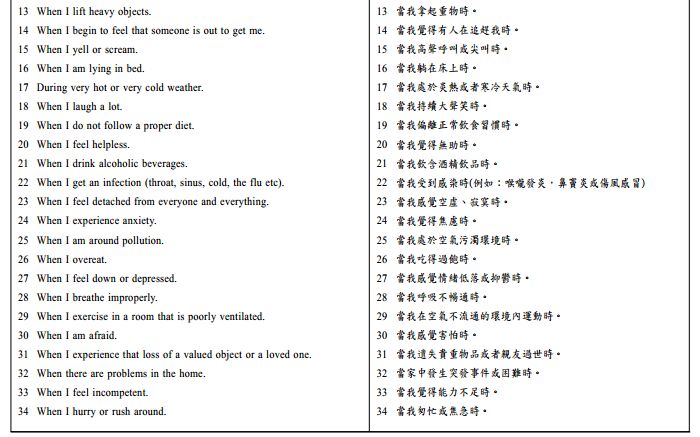
Introduction Chronic obstructive pulmonary disease (COPD), characterized by both lung function impairment and disease exacerbation, promotes a cycle of decline that include dyspnea, reduced exercise endurance, physical inactivity and deconditioning, leading to disease progression and, consequently, to disability, poor health related quality of life, and premature mortality.1 Many individuals with COPD develop a lack of confidence regarding their ability to avoid breathing difficulty while participating in certain activities. This lack of confidence may be expressed as low self-efficacy.2 As a result of low self-efficacy, COPD patients may refrain from many routine activities of daily living.2 COPD Self-Efficacy Scale (CSES) Self-efficacy refers to the personal convictions people have regarding whether or not they feel they can successfully execute particular behaviour in order to produce certain outcomes.3 The CSES was developed specifically for COPD and had shown good test-retest reliability and internal consistency.2 There are 32 items categorized onto 5 domains, namely 'negative affect', 'intense emotional arousal', 'physical exertion', 'weather/environment' and 'behavioural risk factors in CSES'. Once problem areas or activities are identified via the CSES, patient's self-efficacy in those situations may be increased through procedures such as systematic desensitization or self-management training. In addition, the information will provide health care providers with a basis for directing further intervention or be used as monitoring tools in the management of COPD patients. Objective The objective of this study was to translate and validate a language relevant tool for evaluating the self-efficacy scale of Chinese speaking COPD patients in Hong Kong. Methodology Sample size estimation: The primary outcome of the study is the test-retest reliability of the CSES-Chi and we expected a strong correlation between the score at test and retest. According to Cohen's estimation, the sample size for detecting a large effect correlation, i.e. r=0.5, at 5% level of significance and 80% power, is 28.4; hence 30 subjects were recruited. Three-stage approach A three–stage approach was adopted in the development of Chinese COPD Self Efficacy Scale (CSES-Chi). Stage 1 : Forward - backward translation and development of CSES-Chi An expert panel including a doctor, a physiotherapist, a nurse and a COPD patient was established. CSES was first translated into Chinese by one translator. The Chinese version was then back translated into English by a second translator who was blinded to the original English CSES version. Members of the panel were asked to evaluate the language equivalency, language relevancy, and content validity of the Chinese version, CSES-Chi. 5 patients with COPD were invited for pilot testing the draft version of CSESChi. Patient's responses or opinions regarding the CSES-Chi were summarized and reviewed. The CSESChi was finalized after general consensus was achieved within the expert panel. Stage 2: Evaluation of CSES-Chi internal consistency and reliability 30 patients were recruited from a General Outpatient Clinic, based on the following inclusion criteria:
1. Previous diagnosis of COPD; and
Exclusion criteria were:
1. Patients who were wheelchair bound; or
A standardized protocol regarding questionnaires was developed and two research assistants were trained to interview the subjects in a standardized format . The baseline and retest questionnaires were done by different research assistants. Lung function with spirometry, CSES-Chi, self-efficacy for managing shortness of breath, St. George respiratory questionnaire and 6 minutes walking test were used for baseline and interval assessment. The test and retest reliability was assessed by Pearson's correlation coefficient. The Cronbach's alpha was used to evaluate internal consistency. Stage 3: Evaluation of the validity of CSES-Chi Pearson's correlation coefficient test was used to assess the correlation between CSES-Chi and other assessment/questionnaire instruments. COPD definition The diagnosis of COPD was confirmed by spirometry, ± a bronchodilator reversibility test. The severity of the COPD and bronchodilator reversibility were based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines.5
Self-efficacy for managing shortness of breath SEMSOB uses one question to evaluate how confident a patient can keep their shortness of breath from interfering with what they want to do.6 St. George Respiratory Questionnaire (SGRQ) The St. George Respiratory Questionnaire (SGRQ) is designed to measure health impairment in patients with asthma and COPD.7 It is also valid for use in bronchiectasis Six-minutes walking test (6 MWT) The 6-MWT is a practical simple test for the objective evaluation of functional exercise capacity. This test measures the distance that a patient can walk on a flat, hard surface in a 6-minute period.9 The test and retest 6 -MWT were conducted by different physiotherapists according to a standardized protocol. This translation and validation study has been approved by the Clinical Research Ethics Committee, Kowloon West Cluster of Hospital Authority.
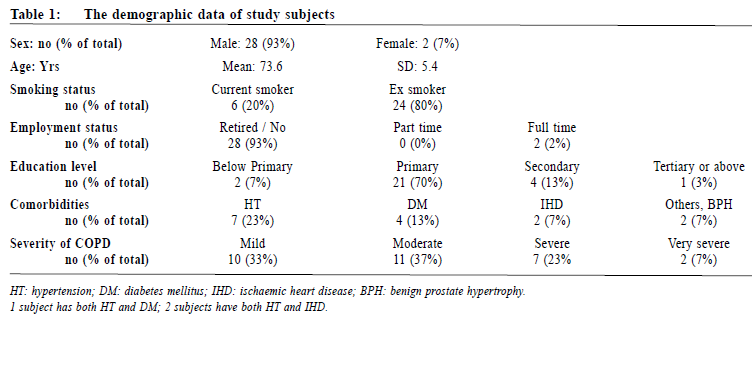
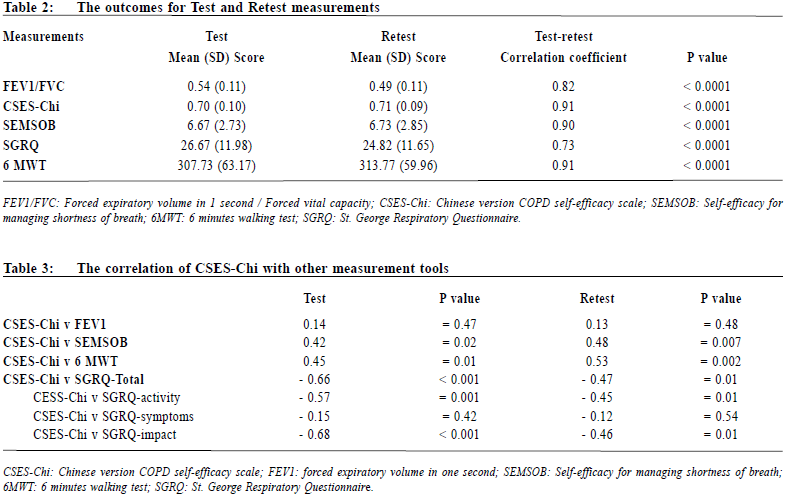
Results 28 male and 2 female patients completed the study. Their demographic data are summarized in Table 1. The mean (SD) age was 73.6 (5.4) years. The number (percentage) of patients with mild, moderate, severe and very severe COPD were 10 (33%), 11 (37%), 7 (23%) and 2 (7%) respectively. Most of them (93%) were retired or unemployed, with low education levels. All patients have a history of tobacco-smoking exposure, with 20% of them still currently smoke. Baseline test and retest results are shown in Table 2. The Pearson correlation coefficient between test and retest ranged from 0.73 to 0.91 (P < 0.0001). CSESChi had a high internal consistency as demonstrated by a Cronbach's alpha of 0.947, and an excellent retest reliability (Intraclass correlation coefficient of 0.9 (95% CI 0.80 to 0.95)). The Pearson product-moment correlation was used to assess the relationship between CSES-Chi and other instruments (Table 3). The CSES-Chi was positively correlated with SEMSOB, with r-values of 0.42 and 0.47 during baseline test and retest respectively. CSESChi was also positively correlated with the 6 minutes walking test, but negatively correlated with St George Respiratory Questionnaire. CSES-Chi did not correlate with lung function or forced expiratory volume in 1 second (FEV1). The pattern of correlation in baseline assessment and retest assessment are similar.
Discussion According to the World Health Organization, COPD will be the fifth commonest disease and the third cause of morbidity in the world by 2020. Currently, COPD is the fifth leading cause of death in Hong Kong.10 According to statistical report from the Hospital Authority, COPD was the cause of 4% of all urgent hospital admission yearly.11 A local study suggested that 9% of those above 70 years of age have COPD.12 Chronic disease management requires a multidisciplinary approach, focusing not only physical aspects, but also psychosocial aspects and quality of life. Low self-efficacy arises when a patient generalizes his or her past experience in certain situations to a similar states or activities. Corrective learning occurs through the individual's successful accomplishments , through individual vicarious experiences, verbal persuasion, or decreased emotionalarousal.3 It is obvious that self-efficacy acts as the mediator between changes in health related quality of life, symptoms and physiological outcomes in patients with COPD after treatment or rehabilitation. The information provided by the CSES may assist the physician, other health care providers or behavior scientist in a number of ways. Firstly, the information may serve to explain why patients engage in some activities but not in others. It is because patient tend to repeat behaviour for which self-efficacy is high and avoid behaviour for which self-efficacy is low.3 Secondly, the information will provide the physician or other health care providers with a basis for directing patients towards activities they believe the patient can perform successfully and be able to perform.2 Thirdly, the CSES would be useful in measuring increases in self-efficacy following an educational or self-management intervention. Most COPD patients are elderly and generally not well educated. They may be unable to understand or comprehend the questions in CSES. Some of the situational description may not be social or cultural relevant . Therefore , a Chinese version is more appropriate for local COPD patients. In our study, all the measurements have good correlation between test and retest assessments. Furthermore, CSES-Chi positively correlated with SEMSOB and 6 minutes walking test as would have been expected. The CSES-Chi was inversely correlated with SGRQ 13, since higher SGRQ scores indicated worse health status. Lung function was not correlated with CSES-Chi, which was also expected since lung function may not fully reflect symptom intensity, function capacity and general well-being.14 Limitation of the study This study evaluated the direct literal translated version of CSES, without additions or deletions to the original questionnaire. It did not evaluate the CSES from a cultural perspective. Only COPD patients in one clinic were recruited, thus reducing this study's generalisability. A population wide study including cultural adaptation processes should be conducted in the future.On average, most patients needed around 20 to 30 minutes to complete the questionnaire, and also need assistance from the research assistant. A simplified version maybe more appropriate for local COPD patients.Another limitation is the fact that the sample size was calculated based on the sample required for evaluating test/retest reliability. As a result, a larger sample size may be required to evaluate the validity of the instrument. Conclusion CSES-Chi is a reliable interviewer-administered clinical assessment tool with good validity for self-efficacy in Chinese speaking patients with COPD in the primary care setting. The validity of CSES-Chi is mediumand which needs further evaluation. Acknowledgment The authors would like to thank all patients who participated in the study. This study was supported by the Tung Wah Group of Hospitals Research Fund.
Lap-kin Chiang,MBChB (HK), MFM (Monash)
Resident General Outpatient Department, Kwong Wah Hospital Lorna Ventura Ng, MRCP(UK), FRACGP, FHKCFP, FHKAM(FM) Sr Medical Officer i/c and Family Medicine Co-ordinator Kwong Wah Hospital Lawrence Fung, Cert. in Physio, MSc (Health Care) Department Manager, Raymond Tang, PDip in Physio, MSc (Pain Medicine) Physiotherapist I, Physiotherapy Department, Kwong Wah Hospital Wilson WS Tam,BSc, MPhil, PhD Research Assistant Professor, School of Public Health & Primary Care, The Chinese University of Hong Kong
Correspondence to :Dr Lap-kin Chiang, General Out-patient Department,
1/F, Tsui Tsin Tong Out-patient Building, Kwong Wah Hospital,
25 Waterloo Road, Kowloon. Hong Kong SAR.
References
|
|