|
December 2011, Volume 33, No. 4
|
Original Articles
|
Usefulness in using portable overnight pulse oximeter for screening obstructive sleep apnea in adult patients in primary health care settingLap - kin Chiang 蔣立建, Peter TK Ng 吳子敬, Cheuk - Wai Kam 金卓慧, Lorna V Ng 吳蓮蓮, Chak - Yan Wong 黃澤仁, Kwok-sang Yee易國生, Hoi - Nam Tse 謝海南, Albert Lee 李大拔 HK Pract 2011;33:146-152 Summary
Objective: 1. To test the usefulness of using portable overnight
pulse oximeter for obstructive sleep apnea screening in primary health care. 2.
To assess the diagnostic accuracy of using portable overnight pulse oximeter for
obstructive sleep apnea screening in primary health care.
Keywords: Obstructive sleep apnea, portable overnight pulse oximeter, primary health care 摘要
目的: 1.測試基層醫療使用便攜式通宵脈搏血氧儀篩選阻塞性睡眠窒息症的效用。2.評估基層醫療便攜式通宵脈搏血氧儀診斷阻塞性睡眠窒息症的準確度。
Introduction Obstructive sleep apnea (OSA) is a condition characterized by disordered breathing during sleep. Prevalence of OSA is estimated to be between 4-8%.1,2 Cardiovascular 3-8 and neuropsychologicalmorbidities 9 and increased risk of motor vehicleaccidents 10,11 have been demonstrated in patients with untreated obstructive sleep apnea. Overnight full channel polysomnography (PSG) performed in a sleep laboratory remains the gold standard diagnostic test. However, PSG is time consuming, costly and requires expertise for interpretation.12 According to Young's study, 82% of men and 93% of women have undiagnosed moderate to severe sleep apnea.13 Based on the estimated prevalence of sleep apnea, the cost of full PSG to diagnose all suspected cases would be prohibitive.12 A vast number of patients present to primary health care for subjective daytime sleepiness, frequent snoring at night or other symptoms suggestive of obstructive sleep apnea. A conservative estimate of the "at risk" population who might be expected to be referred for assessment is at least twice the prevalence (13%) of moderate sleep apnea.14 Due to limitation of clinical assessment and lack of diagnostic test, the usual practice for primary health care physicians is to refer patients to a respiratory physician or sleep centre for confirmation test. According to Flemons et al, the waiting time for sleep service in five countries range from 2 to 60 months.14 There is a need for a simpler and cheaper screening test that can be implemented in primary care. Methodology Objective
1. To test the usefulness of using portable overnight pulse oximeter for obstructive
sleep apnea screening in primary health care.
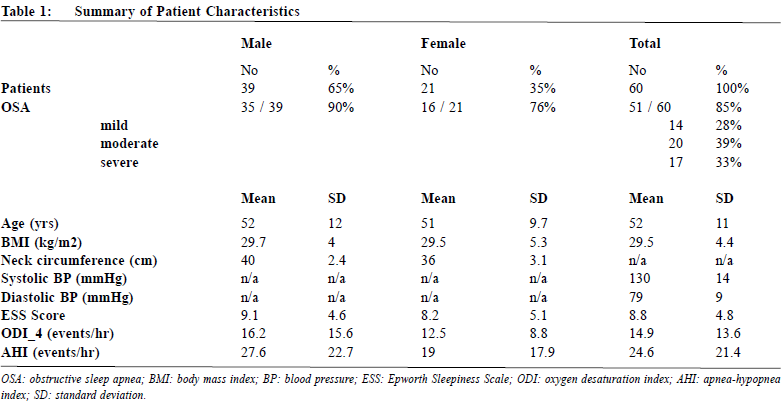
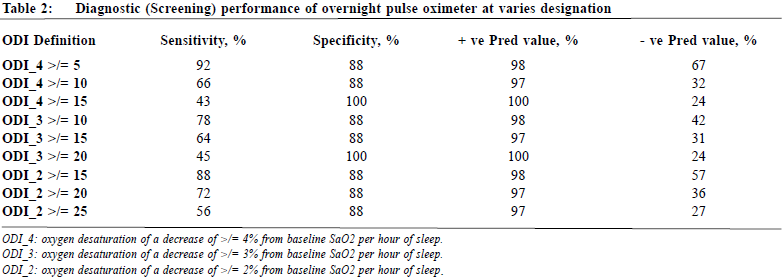
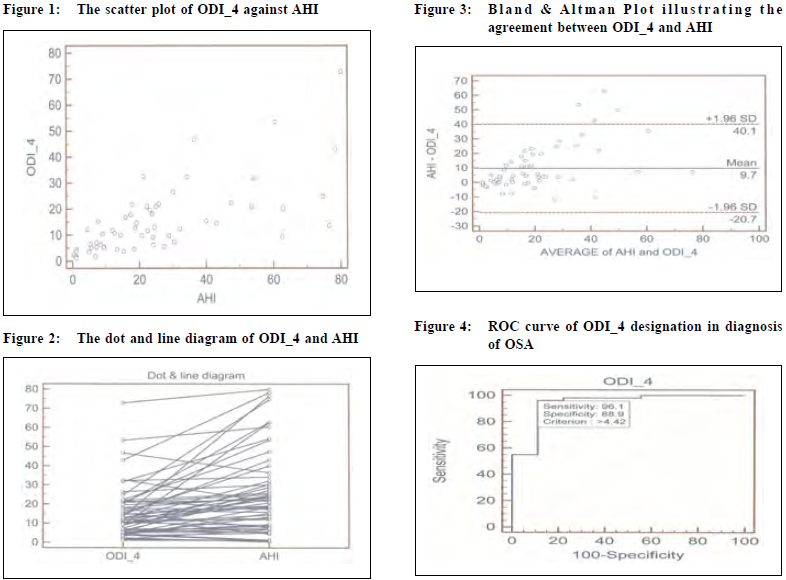
Study population 60 consecutive patients aged from 18 to 75 years old attending a general outpatient clinic, with one or more of the following criteria were recruited: body mass index (BMI) > 25kg/m2; neck circumference > 16 inches for women, > 17 inches for men; poorly controlled hypertension (note 1); poorly controlled type 2 diabetes mellitus (note 2); congestive heart failure; cardiac arrhythmia; erectile dysfunction of undetermined aetiology; subjective daytime sleepiness or excessive snoring at sleep. Exclusion criteria include: haemoglobin < 10 g/l; poor tissue perfusion (such as Raynaud's disease), nail vanish, fungal infection of nails; chronic obstructive pulmonary disease (COPD);or difficult to co-operate (such as dementia). Study design In this prospective study, overnight pulse oximetry was arranged for patients attending a general outpatient clinic with suspected OSA after a focused assessment (including history, physical examination and use of the Epworth Sleepiness Scale). All study patients were then referred to a Sleep Study Centre for at-home overnight PSG. This study was approved by the Clinical Research Ethics Committee, Kowloon West Cluster of the Hospital Authority. Measurement Polysomnography PSG was arranged by the sleep centre about 2 to 4 weeks after the overnight pulse oximetry, and was performed in patients' own home. All PSG data were recorded by a computerized polysomnographic system (Alice 5, Philips). These included standardized montage: two channel electroencephalograms (EEG), electro-oculograms (EOG), submental and leg electromyograms (EMG), electrocardiography (ECG), airflow measurement by thermistor, thoraco-abdominal movements measured by inductive plethysmography, and SaO2 with pulse oximeter. Portable overnight pulse oximeter The Konica Minolta Pulsox - 300i portable overnight pulse oximeter was used for this study. Pulse rate and SaO2 value were continuously measured overnight and stored in the oximeter. Recorded data were then transferred to a computer for processing and analysis. The SaO2 analysis, pulse rate analysis, oxygen desaturation index (ODI: number of oxygen desaturation events per hour of measurement time) and pulse disorder index (pulse rises events per hour of measurement time) were generated in the report. Event definition For both PSG and overnight pulse oximetry, apneas, hypopneas, apnea-hypopnea index, oxygen desaturation and oxygen desaturation index were defined according to standard criteria. The PSG apnea-hypopnea index (AHI) was considered as the diagnostic definition for OSA, where OSA severity is categorized as mild (AHI = 5 to 14 events/hr), moderate (AHI = 15 to 30 events/hr), and severe (AHI > 30 events/hr).15,16 Oxygen desaturation was defined as a decrease of ≥ 4% from baseline SaO2.15 Oxygen desaturation index (ODI_4) was used as screening diagnostic criteria in this study. Subjects who had sleep disordered breath events associated with 5 or more oxygen desaturation events of the peripheral artery of 4% or greater per hour (ODI_4 ≥ 5/hr) was defined as screening positive. Statistical analysis Continuous variables were described as mean and standard deviation (SD). The correlation and agreement between ODI and PSG derived AHI in the diagnosis of obstructive sleep apnea were assessed using Pearson's product-moment correlation coefficient and Bland- Altman plots.17 Overnight pulse oximetry was used as the test and polysomnography as the gold standard for the correct classification of OSA and non-OSA patients. The number of true-positive (TP), false-positive (FP), true-negative (TN) and false-negative (FN) were then determined. Sensitivity (TP/[TP+FN]), specificity (TN/[TN+FP]) and positive (TP/[TP+FP]) and negative predictive values (TN/[TN+FN]) were calculated. A receiver operating characteristic (ROC) curve was constructed for reviewing the comparative course of sensitivity and 1-specificity at different thresholds. Quality assurance All computer generated overnight pulse oximetry and polysomnography would be verified by respiratory specialist to ensure validity and quality. PSG was performed by trained technician from Celki Medical Company, which provided sleep study equipment and support to sleep study centres under the Hospital Authority of Hong Kong. Results Patient characteristics 60 consecutive patients (21 females and 39 males) were successfully recruited from November 2009 to June 2010. Table 1 summarizes the patients' characteristics, anthropomorphic measurements, overnight pulse oximetry and PSG results. Correlation and agreement between overnight pulse oximetry and polysomnography OSA was diagnosed by PSG in 51 patients, with a mean AHI of 24.6 events/hr (SD = 21.4 events/hr). The number (%) of mild, moderate and severe OSA were 14 (28%), 20 (39%) and 17 (33%) respectively. The mean overnight pulse oximetry derived ODI_4 was 14.9 events/hr (SD = 13.6 events/hr). Both scatter plot (Figure 1) and dot and line diagram demonstrated (Figure 2) a linear relationship between ODI_4 and AHI. Pearson's correlation coefficient for ODI_4 and PSG derived AHI was 0.7 (P < 0.0001). The mean and 1.96 SD of the difference between ODI_4 and AHI was 9.7 events/hr and 30.4 events/hr. The Bland & Altman Plot is illustrated in Figure 3. Most dots lied between the +/- 1.96 SD of the mean difference line. Diagnostic (Screening) performance of overnight pulse oximetry The diagnostic performance of overnight pulse oximetry at various designation were tabulated in Table 2. A receiver operating characteristic (ROC) curve of ODI_4 in the diagnosis of OSA was shown in Figure 4. Based on ROC curve of ODI_4, the best cut off criterion is 4.42 events/hr, with a sensitivity and specificity of 96.1% and 88.9% respectively. Using case designation criteria of ≥ 5 events/hr for ODI_4, the sensitivity and specificity for OSA diagnosis are 92% and 88% respectively.
Discussion To be an effective screening tool for OSA, overnight pulse oximetry must be able to screen out patients with all levels of disease severity and be able to rule out patients without disease in a manner that is less expensive than current diagnostic procedures. We investigated the usefulness of overnight pulse oximetry as a screening tool for OSA by comparing diagnostic performance directly with PSG. According to review paper by Nikolaus et al, there was broad range of sensitivity and specificity value for pulse oximetry as a screening tool for sleep-disordered breathing, the value for sensitivity ranged from 31 to 98% while specificity ranged from 41 to 100%.15 In our study, ODI _ 4 and AHI had a good correlation. Nevertheless, ODI is globally less than AHI, the reasons for which are unclear. Decreased sleep efficiency may decrease the ODI since it is derived from the total probe-on time and not total sleep time.18 Furthermore, technical limitations may impair the detection of hypopneaic changes. The typical cyclical drop in SaO2 in patients with OSA lags 45 to 60 seconds behind a respiratory event and should be accurately detected at this measurement speed.19 For screening purpose, one chooses a high sensitivity in order not to falsely exclude from further investigation patients having the disease in question. For treatment decisions, one chooses a higher specificity in order not to inflict investigation or treatment on patients without the disease. There is no uniform definition for a normal or abnormal oxygen desaturation index (ODI).15 In Stradling JR 20, Kripke DF et al 21 studies, the threshold for an abnormal ODI is either ≥ 5 desaturation per hour. Using this designation in our study, the sensitivity, specificity, positive predictive value and negative predictive value are 92%, 88%, 98% and 67% respectively. The results support the implication of overnight pulse oximetry as the screening tool for OSA for selected population in the primary health care. Epworth Sleepiness Scale (ESS) is a validated method of assessing the likelihood of falling asleep in a variety of situations.22 Although the correlation between ESS and OSA severity is relatively weak, ESS is the best available tool to guide the clinician as to the patients' perception of his/her sleepiness.23,24 Continuous positive airway pressure (CPAP) functions as a pneumatic splint to maintain upper airway patency through all phases of sleep breathing. CPAP has been established as the treatment of OSA with the firmest evidence base.25 American Academy of Sleep Medicine (AASM) recommended CPAP as the standard treatment of moderate to severe OSA and self-reported sleepiness, while it is the optional treatment for mild OSA, improving quality of life or as an adjunctive therapy to lower blood pressure in hypertensive patients with OSA.16 Key messages
1. OSA is common with an estimated prevalence between 4 - 8% of the population.
Oximetry alone is often used as the first screening tool for obstructive sleep apnea due to the universal availability of cheap recording pulse oximeters.26 In Japan, overnight pulse oximetry had been used for OSA screening for workers in transport, construction, retail and security companies. The study concluded that the simplicity of the sleep apnea syndrome screening by overnight pulse oximetry makes it easy to use for screening of workers, and this method was highly effective in detecting individuals with severe sleep apnea syndrome for whom continuous positive airway pressure (CPAP) therapy was indicated.27 Based on current available evidences or recommendations and results from this study, it is suggested that CPAP might be initiated to selected patients if he or she has OSA associated symptoms and overnight pulse oximetry confirmed OSA of at least moderate severity. This clinical pathway may reduce the harm associated with OSA when diagnosis is delayed due to prolonged waiting time. Further studies should be conducted to assess the feasibility, safety and outcome of initiating CPAP for patients in the primary health care setting. Key Conclusion In a selected adult primary care population who are at risk for OSA, overnight pulse oximetry shows good correlation with PSG and has good performance as a screening tool for the diagnosis of OSA. Acknowledgment This study was funded by the Hong Kong College of Family Physicians Research Fellowship award 2009. Authors would like to thank the Hong Kong College of Family Physicians for providing generous support to research in the primary care.
Lap-kin Chiang, MBChB (HK), MFM (Monash)
Resident Peter TK Ng, MBBS (HK), MFM (Monash), FHKCFP, FRACGP Medical Officer Cheuk-wai Kam, LMCHK, MFM (CUHK) Medical Officer Lorna Ventura Ng, LMCHK, MPH (CUHK), FHKCFP, FHKAM (Fam Med) Senior Medical Officer i/c General Outpatient Department, Kwong Wah Hospital Chak-yen Wong, MBBS, FHKAM (Resp Med) Retired Senior Medical Officer Chest and TB Unit, Wong Tai Sin Hospital Kwok-sang Yee, MBChB, FHKAM (Resp Med) Consultant Hoi-nam Tse, MBChB, FHKAM (Resp Med) Resident Specialist Department of Medical and Geriatrics, Kwong Wah Hospital Albert Lee, MD, FFPH(UK), FHKCFP , FHKAM(Fam Med) Professor (Clinical) School of Public Health and Primary Care, The Chinese University of Hong Kong Correspondence to : Dr Lap-kin Chiang, General Outpatient Department, 1/F, Tsui Tsin Tong Outpatient Building, Kwong Wah Hospital, 25 Waterloo Road, Mongkok, Kowloon. Hong Kong SAR.
References
|
|