|
June 2011, Volume 33, No. 2
|
Original Articles
|
A pilot follow-up study on the use of a reminder system among patients with unsatisfactory control of diabetes mellitus in a Hong Kong public family medicine clinicKar-fai Lee 李嘉輝, Man-li Chan 陳萬里, Liang Jun 梁峻 HK Pract 2011;33:56-62 Summary
Objective: A pilot follow-up study was designed to evaluate the
use of a reminder system in improving the management of diabetic patients with unsatisfactory
control in a primary health care setting. Such patients were defined as those with
HbA1c level ≥ 9%.
Keywords: Diabetes mellitus, reminder system, suboptimal diabetic control, HbA1c. 摘要
目的: 以試驗性跟進式研究評估在基層醫療環境下,是否可以利用一個提示系統改善糖尿病控制欠佳病人的治療。該等病人為其HbA1c水平在9%或以上。
主要詞彙: 糖尿病,提示系統,控制欠佳,糖化血紅素。 Introduction Diabetes is a very common chronic disease. The worldwide prevalence was estimated to be 2.8% in 2000 and 4.4% by 2030.1 It is higher in developed countries. The total number of people worldwide with diabetes is projected to rise from 171 million in 2000 to 366 million in 2030.1 Diabetes causes about 5% of all deaths globally each year.2 In Hong Kong, the age adjusted prevalence was 7.7% in 1990 and increased to 8.5% in 1995.3 The elderly population (more than 65 years old) has an even higher prevalence.4 It is the ninth commonest cause of deaths in Hong Kong.5 Poor diabetic control is associated with worse health outcome. It was confirmed in a large prospective cohort that increased HbA1c was an independent risk factor for cardiovascular disease. For each 1% increase in HbA1c, the hazard ratio for cardiovascular disease was 1.08.6 Healthcare costs also increase with increasing HbA1c levels.7 Improvement in diabetic control decreases disease burden at the patient and society level. Reminder systems have been used in different ways to improve clinical care of patients. There is a wide variety of clinical reminders. Some target on doctors and some are for patients. It can be patient specific or generalized. The format may be electronic, phone-based or paper-based. Studies showed that reminder systems improved smoking-status documentation,8 vaccination uptake rate,9-11 health screening 12-14 and adherence to medication.15 For diabetes, reminder systems have been used in screening and management processes. A patient and computer reminder system in New Zealand was shown to be effective in increasing screening for diabetes. 16 Doctor-oriented HbA1c tracking tool 17 and real-time reminder protocol 18 are useful to improve management of diabetic patient and reduce complications. Patient-oriented point-of-care computerized diabetes-care reminder system was accepted by both patients and providers and improved the quality of outpatient-care for diabetic patients.19 Computerized reminder systems also help to improve compliance with recommended care by facilitating the documentation of clinical findings and the ordering of recommended procedures.20 Study on the use of reminder system for clinical care of diabetes patients with unsatisfactory control have scarcely been done. Objectives
Method The study was conducted in Tuen Mun Hospital family medicine clinic in 2008. It is a public hospital in New Territories West Cluster of Hong Kong Hospital Authority. The clinic is fully computerized. There are about 600 patients with diabetes mellitus in the clinic. Diabetic complication screening is performed annually and results including HbA1c level are recorded in the computer system. The study was approved by the Tuen Mun Hospital Research Ethics Committee. Subjects Patients with diabetes mellitus attending the author's clinic from 1st November 2006 to 31st October 2007 satisfying the following inclusion criteria were included:
• HbA1c ≥ 9% Study design This was a cohort study. The latest HbA1c level within 1 year before the start of the study (March 2008) were recorded and compared with the HbA1c level within 6 months before the end of the study (June 2009). Intervention An electronic reminder was created in the Hospital Authority Clinical Management System [CMS] by one of the authors who is a family medicine specialist. Content of the reminder was based on the departmental management consensus in March/April 2008. It would pop up on the computer screen every time the patient's record was accessed. It would remind the attending doctor that it was a case of poor diabetic control and suggested several ways to improve glycemic control. They included 1) referring patient to community care centre or dietitian for diabetic health education, 2) referring patient to diabetic centre for initiation of insulin, 3) adjusting drug dosage (oral hypoglycemic agent or insulin) and 4) close monitoring of diabetic control by checking HbA1c half yearly. These four points were generically included in the reminder content. Outcomes The study lasted 1 year. Patients' records were reviewed in June 2009. The primary outcome was the change of HbA1c level. The time period between pre and post intervention HbA1c level checking was about one year. The secondary outcome was doctors' response rate to the reminder and the use of insulin. Patient demographics and duration of diabetes were also collected. Statistical method The change in the HbA1c profile before and after the study was tested with the paired student's T-test. Results 57 patients were recruited. One patient died of cancer. Another patient was referred out because of dementia. 55 patients continued to have follow-up in the clinic at the end of the study. Patients characteristics The patient profile is shown in Figure 1. The average HbA1c at the start of the study was 10.03%.
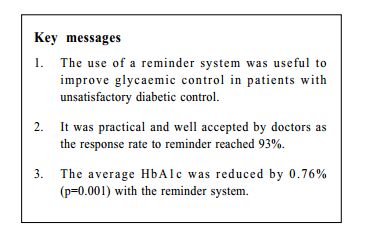
Outcomes Doctors were active in using different tools to improve diabetic control including referral to community resources and diabetic centre, increasing oral hypoglycemic agents or insulin dosage and more frequent checking of HbA1c level (Figure 2). The overall response rate to the reminder reached 93%. (Response was counted if one or more of the reminder recommendations was followed) The average HbA1c was improved by 0.76% from 10.03% to 9.27% at the end of the study (p=0.001) and the 95% confidence interval of HbA1c improvement was 0.35 to 1.17. Fifteen patients (27%) newly received insulin treatment after the study. Forty patients (73%) showed improvement in HbA1c level.
Discussion The reminder system was practical and easily adopted in the author 's clinic. It was convenient to draw a patient list with poor diabetic control in a computerized clinic with data retrieved from the Hospital Authority information technology department. It was also well accepted by doctors as reflected by the high response rate to the reminder. The reminder response rate was high. Previous systematic review showed computer reminders improved adherence to processes of care by a median of 4.2%.21 The doctors were active in using different tools to improve HbA1c control. The authors proposed that the active behavioural pattern was related to the implementation of the reminder system and this in turn contributed to the improvement in HbA1c value in the reminder group. The results were encouraging. Evidence generated from the United Kingdom Prospective Diabetes Study shows that HbA1c reduction results in significantly lower risk of developing macrovascular and microvascular complications.22 The better diabetic control as reflected from the decreased HbA1c should help to decrease health burden on patients and health care cost. Setting up a reminder system involves identification of target patients and input of reminder. This is a time consuming process and may cause difficulties for other family medicine clinics or primary care clinics with a large number of diabetic patients. It could be facilitated with the use of computer system to identify target patients. In the setting of the Hospital Authority clinics, this can be achieved with the help from the information technology department. For clinics using computer system to manage patient record, e.g. Clinic Solution version 6.0 the software can sort out a list of patients with high HbA1c level. The input of reminder could be helped with standardized template and mobilization of other clinic staff, e.g. clerks and nurses. Limitations The small sample size may affect the generalization of the result to other practices. Because of the lack of the control group, the improvement of HbA1c level after the study may not be solely contributed by the reminder system. Conclusion Reminder system is useful to improve diabetic care for those with poor control. It is likely that this kind of system is also useful in the management of other chronic illness, e.g. hypertension and hyperlipidaemia. Family physicians may consider setting up reminder system to improve chronic illness management and it is practical and easy to set up such systems.
Kar-fai Lee, MBBS, FHKCFP, FRACGP, DFM (HKCFP)
Higher Trainee, Man-li Chan, MBChB, FHKCFP, FRACGP, FHKAM (Family Medicine) Associate Consultant, Liang Jun, MBChB (Glasg), MRCGP (UK), FHKAM (Family Medicine) Family Medicine Consultant and Coordinator Department of Family Medicine, Community Care Division, New Territories West Cluster, Hospital Authority. Correspondence to : Dr Kar-fai Lee, Department of Family Medicine, Community Care Division, New Territories West Cluster, Hospital Authority, Hong Kong SAR.
References
|
|