|
June 2011, Volume 33, No. 2
|
Original Articles
|
Review of vitamin B12 deficiencymanagement in a family medicine clinicMan-kei Lee 李文基, Pak-kin Wong 黃柏鍵, Kenny Kung 龔敬樂, Augustine Lam 林璨 HK Pract 2011;33:64-71 Summary
Objective: To review the current practice for patients diagnosed
with vitamin B12 deficiency in a family medicine clinic.
Keywords: Diabetes mellitus, reminder system, suboptimal diabetic control, HbA1c. 摘要
目的: 審閱現時家庭醫學診所診斷為治療維生素B12缺乏症患者的治療現狀。
主要詞彙: 維生素B12, 基層醫療, 惡性貧血。 Introduction Vitamin B12 is essential in DNA synthesis and neurological functions. Vitamin B12 deficiency will result in haematological, neurological and psychiatric defects.1 We frequently encounter patients diagnosed with vitamin B12 deficiency. Depending on the defining criteria, the prevalence of B12 deficiency among the elderly can be up to 43%.2 Although low serum B12 level is the obvious and commonest diagnostic criteria for B12 deficiency, other tests like methylmalonic acid (MMA) and homocysteine (HCY) levels may be more sensitive in diagnosis.3,4 There are diverse causes of vitamin B12 deficiency. Some can be easily elicited from history such as vegetarian diet, metformin use and post-gastrectomy status. Others like pernicious anaemia do need investigation for confirmation. Anti-intrinsic factor antibody (Anti-IF) and anti-parietal cell antibody (Anti-PA) are commonly used for diagnosis. Traditionally, doctors preferred to prescribe parenteral replacement of vitamin B12. Traditional teaching states that vitamin B12 can only be combined with intrinsic factor for absorption. In fact, vitamin B12 can be absorbed directly by diffusion without the need for intrinsic factor. However due to its inconvenience and substantial workload to health care workers, more doctors turn to oral vitamin B12 supplement. Studies had shown the comparable effectiveness of oral supplement.5 In view of the diversity in diagnosis, investigation for and management of B12 deficiency in our local setting, a review of the current practice for patients diagnosed with B12 deficiency was performed with a focus on the followings:
1) how doctors defined patients as having vitamin B12 deficiency Method This was a retrospective non-interventional study performed in the Family Medicine Training Centre (FMTC) at the Prince of Wales Hospital. The FMTC receives patient referrals from other PWH specialties including internal medicine for continuation of care. It also functions as a triage clinic and receives new case patient referrals from the Emergency Department or General Outpatient Clinics for more sophisticated investigation and management. All patients attending the FMTC and prescribed with either oral or intramuscular vitamin B12 during the period from 1st January 2008 to 31st December 2008 were included. Patients were identified through the Clinical Data Analysis and Reporting System (CDARS) of the Hong Kong Hospital Authority. Patients were included if both pre and post-treatment serum B12 level were available (the dates of which may be outside the study period), and if B12 had been prescribed continuously for at least three consecutive visits. Computer clinical records of included patients were reviewed. Apart from patient demographics, the following specific information were collected:
• past history of gastrectomy or significant gastric disease Results During the study period, 192 patients had been prescribed with any form of vitamin B12. Twenty-two patients were excluded as not fulfilling the inclusion criteria as above. The remaining 170 patients had been diagnosed with vitamin B12 deficiency either in FMTC or by other specialties prior to their referral to our centre. Figure 1 outlines the study population's demographics. The majority were elderly with a mean age of 72.8. There was a slight female preponderance. Cardiovascular problems were among the commonest disease entities. The top five concomitant diseases were hypertension, diabetes mellitus, hyperlipidaemia, stroke and ischaemic heart disease.
Reason of B12 checking In 47.6% of patients, testing was performed as screening among diabetics taking metformin. Normocytic anaemia, dementia and limb numbness were the less common reasons. Other less documented symptoms related to B12 deficiency included gastrectomy, limb weakness, muscle pain, dizziness, tiredness, vertigo, psychosis and being a vegetarian. Diagnosis of vitamin B12 deficiency The mean baseline serum vitamin B12 level at diagnosis was 146.3pmol/L. In 22 cases (13% of total) and 8 cases (5% of total), baseline levels were greater than 179pmol/L (lab cut-off) and 200pmol/L (traditional arbitrary cut-off) respectively (Figure 2). The highest baseline vitamin B12 level was 448pmol/L. A patient complained of limb numbness and was taken in and given a trial. Subsequently the patient had much improvement of his symptom and vitamin B12 was continuously prescribed. Another case was a vegetarian with baseline level 313pmol/L. Vitamin B12 was prescribed as anticipatory supplementation.
B12 Supplementation – oral vs parenteral Figure 3 shows the case distribution and flow in respect of their route of vitamin B12 supplement. 73% and 27% were initially put on oral route and parenteral supplementation respectively. Among those on oral supplementation initially, 4% were changed to the parenteral route. Among those on parenteral supplementation initially, 35% were changed to the oral route. (The average B12 levels were 577pmol/L and 467pmol/L respectively when treatment changed from parenteral to oral). The reasons for changes are documented in Table 1.
The vitamin B12 dose for all patients receiving the intramuscular route was the standard 1000mcg cyanocobalamin per injection. However, there were variations with regards to whether a loading regime was used or not, and the frequency of injection. For the oral drug regime, the average daily dose was 175mcg. The most frequently prescribed regime was 100mcg bd. Baseline vitamin B12 level was significantly lower in the intramuscular injection group than the oral supplement group (118.2 and 156.8pmol/L respectively). Only injection was started for patients with vitamin B12 level less than 60 pmol/L while only oral vitamin B12 was started for those with levels greater than 200pmol/L (Table 1 and Figure 2). For those with a baseline level less than 200pmol/L, oral supplementation was comparable to injection with at least 90% cases attaining levels greater than 200pmol/L. Both routes achieved significant increases in B12 level (222.6 and 489 respectively) (Table 2).
Causes of B12 deficiency The commonest causes of vitamin B12 deficiency identified were metformin related, followed by pernicious anaemia and diet related to insufficient meat intake. There were also five post partial gastrectomy patients and four vegetarians (Table 1). In 52% (89) of patients, either one or both of anti-IF and anti-PA were checked (Table 3). Subsequently 21 patients were diagnosed with pernicious anaemia. Among the 21 cases of pernicious anaemia, only 10 cases were more likely to have a true diagnosis of pernicious anaemia (anti-IF greater than 20 RU/ml) (lab cut-off). Traditionally speaking, parenteral route was the option of choice for pernicious anaemia. However, in our study, three patients were prescribed with oral vitamin B12 and with a significant mean vitamin B12 increase of 294 pmol/L (Table 4). Similarly for the five gastrectomy cases, three were given oral supplements and resulted in significant mean vitamin B12 rise of 313pmol/L (Table 4).
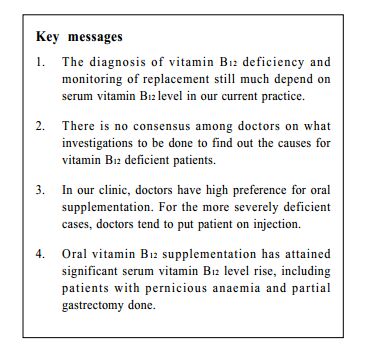
Indicator of successful replacement During our review, we noted that most patients were monitored with vitamin B12 level as indicator of successful replacement. Doctors seldom adjusted the vitamin B12 doses according to initial reasons of checking, e.g. Haemoglobin level or Mean cell corpuscular level. Discussion Definition of vitamin B12 deficiency Many studies had shown that serum vitamin B12 level alone was not sensitive for diagnosing functional vitamin B12 deficiency.6,7 Other markers like typical symptoms and mean cell corpuscular volume (MCV) have supportive roles. However, MCV can also be insensitive as elevated MCV do have other causes and MCV level can be low if there is concomitant iron deficiency. Serum homocysteine (HCY) and methymalonic acid (MMA) levels are more sensitive markers.3,4 However in our clinic, we are still using serum vitamin B12 level alone. Besides cost and limited access to HCY and MMA tests, doctors may also be unaware of these tests. Besides vitamin B12 level, doctors are also using therapeutic trial as test for deficiency. This is the reason why a large part of our cases do have their baseline B12 level higher than our lab cut-off of 179pmol/L. The case with highest B12 level of 448pmol/L is one of the examples. The patient presented with limb numbness and the trial of vitamin B12 did help. Though some may argue for the placebo effect, studies did show that patients with subacute combined degeneration of the spinal cord can have normal serum vitamin B12 level with numbness as the usual first presentation, while recovery in 3 months after supplementation can be expected.3,8 Investigation of the cause of vitamin B12 deficiency Metformin-induced There is no guideline on routine screening of metformin users for vitamin B12 deficiency. However, the prevalence of vitamin B12 deficiency among metformin users was quoted to be 30% in a study.9 In our clinic, putting metformin users in is the most common reason for vitamin B12 level checking since diabetes patients constitute a large pool in our clinic. One local study had shown that the duration and dose of metformin were the most significant risk factors for vitamin B12 deficiency.10 Doctors tend to check vitamin B12 level as screening with low threshold of supplementation, aiming at anticipatory deficiency rather than treatment itself Pernicious anaemia Pernicious anaemia (PA) accounts for 80% cases of megaloblastic anaemia due to impaired absorption of vitamin B12.11 Absorption occurs in the terminal ileum and requires intrinsic factor, secreted from gastric parietal cells, for transport across the intestinal mucosa. Pernicious anaemia, resulting from intrinsic factor deficiency, is believed to be an autoimmune disease, either due to autoimmunity against gastric parietal cells or autoimmunity against intrinsic factor itself. The appropriate testing strategy for diagnosing pernicious anaemia using gastric parietal cell and/or intrinsic factor antibodies is controversial. Circulating gastric parietal cell antibodies are detected in about 90% of patients with pernicious anaemia 12 and are considered as the end stage of type A chronic atrophic gastritis.13 Antibodies to intrinsic factor are seen in 50-70% of patients and are viewed as a more specific marker.14 In other words, presence of anti-IF is virtually diagnostic of pernicious anaemia. Interestingly, a recent local study also showed that there were certain characteristic differences between intrinsic factor antibody (IFA) positive and IFA negative PA patients.15 The latter group was likely to be heterogeneous and might include patients with nonimmune mediated causes of vitamin B12 deficiency. In our clinic, about half of the patients were not screened for pernicious anaemia (81 out of 170). This was probably due to the presence of obvious cause of vitamin B12 deficiency in individual patient (metformin use, vegetarian, etc). Proton pump inhibitor induced Some studies have demonstrated a causal relationship between acid lowering therapy such as proton-pump inhibitors (PPI) and vitamin B12 deficiency.16,17 Acid lowering therapy had not been assigned to be a cause of vitamin B12 deficiency among patients in this study, although 27 patients were on long term famotidine and 2 were on PPI. Proposed reasons included doctors' unawareness of this causal relationship or uncertainty on the duration of use before a significant reduction in vitamin B12 level. During our review, we noted that doctors did not have a consensus on how further they should investigate for the cause of vitamin B12 deficiency. Even being relatively non-invasive, only 89 patients (52% of total) had their autoantibody levels checked. It was likely that there were undiagnosed cases of pernicious anaemia in this subgroup. No local or international guidelines currently exist to guide frontline doctors on the management of patients suspected to have B12 deficiency. There is also no guidance for doctors if patients are known to have health behaviours that are prone for deficiencies, or receiving deficiency prone interventions. It seems logical for those with obvious causes (such as vegetarians or post-gastrectomy patients) not to require testing. However, it is difficult to ascertain whether non-strict vegetarians, those on metformin or acid suppressing therapy have pernicious anaemia related B12 deficiency without formal autoantibody testing. Further analysis is needed in order to define the cost effectiveness of different clinical approaches. Oral vs. parenteral routes of vitamin B12 replacement In a Cochrane review of 108 participants,5 evidence suggested that high oral doses of B12 (1000 mcg and 2000 mcg) could be as effective as intramuscular administration in achieving haematological and neurological responses.5,18,19 At least 63 of these patients were having malabsorption problems like pernicious anaemia or ileal resection. In another dose-finding trial 20 which recruited 120 patients, it compared several oral doses ranging from 2.5 to 1000mcg per day. It used MMA (reflecting the tissue level of vitamin B12) for calculation and concluded that the minimal effective oral dose should be 500mcg per day. With doses from 2.5mcg to 500mcg, there was significant improvement in serum B12 proportional to the doses but the effect to MMA was just not optimal. In our review, oral vitamin B12 supplement was effective in raising vitamin B12 level. Indeed, the oral route was comparable to the injection route with at least 90% of cases attaining levels greater than 200pmol/L. Their mean increases were also significant (222.6 pmol/L and 489 pmol/L respectively). Nevertheless, the mean daily dose in this study was only 175mcg. Therefore, we may not be optimally treating our patients with such low dose of oral vitamin B12 supplementation even with good serum B12 level rise. If we take into account serum B12 level only, the effectiveness of oral route surprisingly also applies to our pernicious anaemia and partial gastrectomy cases. Although the diagnosis of pernicious anaemia was only supported by antibody checking without haematologcal or endoscopic confirmation in most cases, we can divide our cases into definite or probable pernicious anaemia cases similar to a previous local study.21 Those with positive intrinsic factor antibody are defined as definitely having pernicious anaemia, while those with positive parietal cell antibody are defined as possible pernicious anaemia. By this definition, 10 patients with definite pernicious anaemia were included in this study (Table 4). Three of these received oral vitamin B12 and all three experienced a significant rise in vitamin B12 level (294pmol/L). One previous study showed that 68% of patients with partial gastrectomy had vitamin B12 deficiency,22 suggesting that partial gastrectomy was actually a cause of the deficiency. Three patients with partial gastrectomy in this study were on oral vitamin B12 (Table 4) and a significant rise in their mean serum B12 level was observed (up to 313pmol/L). In a study performed in primary care setting in Canada, questionnaires and interviews were performed on 133 patients to assess their views on oral vitamin B12. It was noted 73% patients were willing to try oral vitamin B12 supplement. Patients thought that the frequent visits and travel costs were barriers to vitamin B12 injections.23 Indication of successful replacement In this review, we noted that most doctors were looking at vitamin B12 level rise as the outcome for successful replacement, rather than the initial complaints, haematological disturbances or the more specific HCY and MMA. More resources and doctor education would be needed before HCY or MMA could be considered for use as diagnosis and monitoring. Oral form of vitamin B12 does have better patient tolerability and less staff burden on injection. Further studies on feasibility of oral vitamin B12 with regard to clinical response should be performed. Limitation of this study This is a review study performed in a family medicine clinic inside a hospital setting. The reasons for checking B12 and associated disease pattern may deviate from that in primary care setting. For example, the causes for B12 deficiency like metformin induced or gastrectomy may not be that prevalent in general practice. Clinical notes interpretation for reason of checking vitamin B12 level or the causes of deficiency may be prone to reviewer bias. Further prospective multi-centered studies within a primary care setting need to be conducted in order to obtain more generalized results. Conclusion Vitamin B12 deficiency is not an uncommon condition in primary care setting. Moreover, pernicious anaemia may be under-diagnosed when there are other possible concomitant causes. Even among those with pernicious anaemia, oral supplementation may be effective in restoring vitamin B12 level, although minority of patients may still be under-treated due to suboptimal doses. Future studies will be needed to help setting up guidelines so that front-line doctors can manage patients in a more effective manner.
Man-kei Lee, MBChB (CUHK), Dip Med (CUHK), FHKCFP, FRACGP
Resident in Family Medicine, Pak-kin Wong, MBBS (HK), Dip Med (CUHK), DCH (Ireland) Resident in Family Medicine, Kenny Kung, MFM (Monash), MRCGP (UK), FHKCFP, FHKAM (Fam Med) Associate Consultant in Family Medicine, Augustine Lam, FRACGP, FHKCFP, FHKAM (Fam Med) Chief of Service in Family Medicine Department of Family Medicine, New Territories East Cluster, Hospital Authority Correspondence to : Dr Man-kei Lee, Family Medicine Training Centre, Prince of Wales Hospital, Shatin, Hong Kong SAR.
References
|
|