|
March 2013, Volume 35, No. 1
|
Original Articles
|
A survey on Type II diabetes mellitus patients' understanding of methods of monitoring diabetes control and their preferencesKin-wai Chan 陳建偉, Sau-nga Fu 傅秀雅, Ming-pong Yiu 姚銘邦, Yuk-kwan Yiu 姚玉筠 HK Pract 2013;35:12-20 Summary
Objective: To explore patients' knowledge, attitudes and preferences
about the different monitoring methods in diabetes control.
Keywords: Diabetes mellitus, monitoring, patient's knowledge 摘要
目的: 本研究旨在探討糖尿病人對糖尿病不同監測方法的認知,和對普通科門診採用不同監測方法的個人態度和取向。
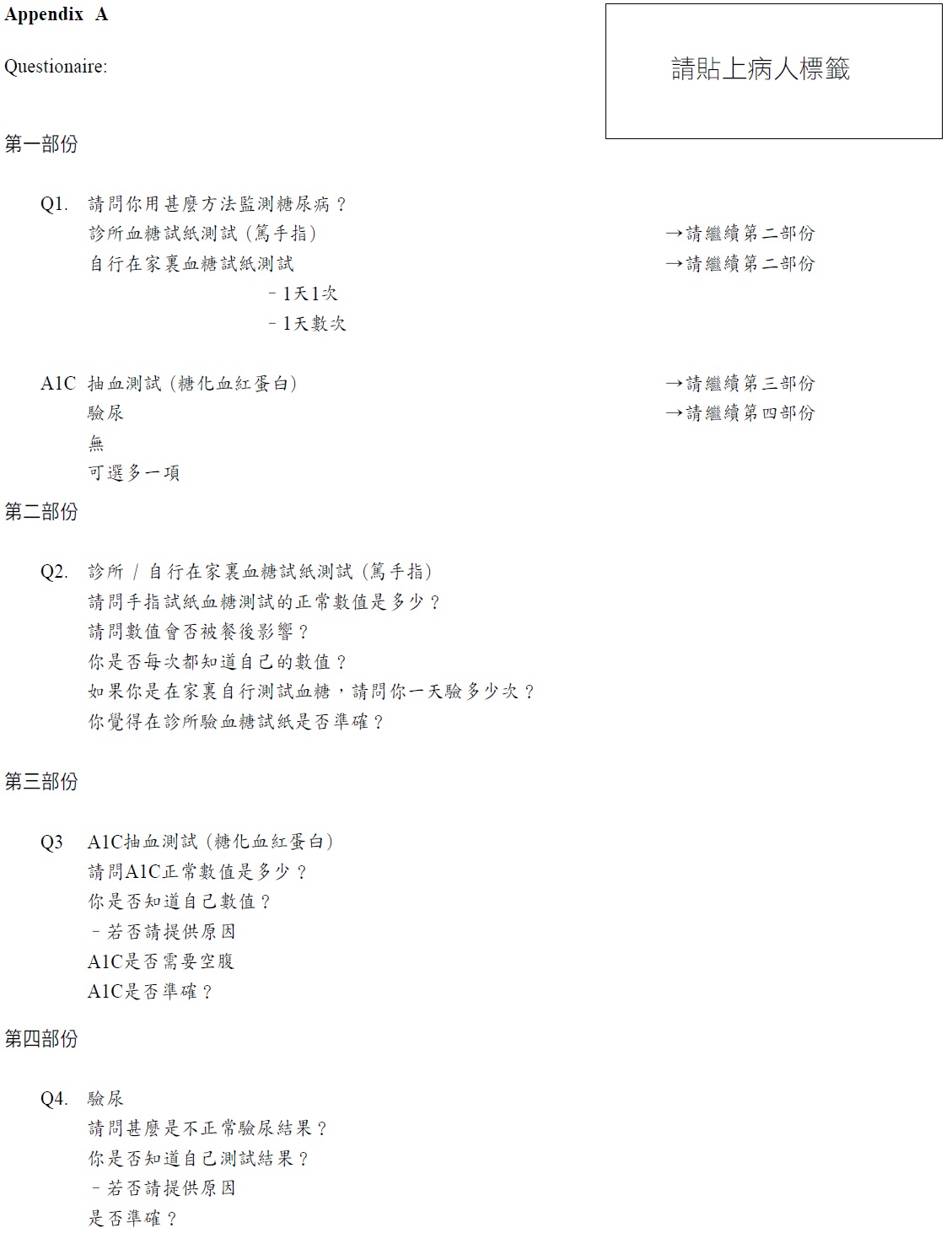
主要詞彙: 糖尿病,監測,病人認知 Introduction Type II Diabetes Mellitus (DM) is a common disease in primary care setting. From a recent Hong Kong morbidity survey, it is the second most common chronic illness of attendance. Satisfactory glycaemic control including HbA1C less than 7% and optimal sugar profile is associated with a decrease in morbidity and mortality.1 The gold standard of monitoring DM control in Type II DM patient is by measuring the HbA1C level.2 Continuous home monitoring of blood sugar level in a full profile is also useful in monitoring DM control, especially in Type I DM.3 However, in the general outpatient clinic, the usual practice is to measure capillary blood sugar (once only) before the doctor consultation during follow up. This capillary blood sugar checking is not done at a certain fixed time, e.g. fasting or post-prandial. There is no study saying that checking the capillary sugar once is a valid method in monitoring DM control.4 Apart from the fact that there is no evidence that checking capillary blood sugar once is useful in monitoring diabetes control, there is another drawback that it may adversely affect the management of our Type II DM patients. For example, many DM patients mix up the value of capillary blood sugar and the HbA1C level. Some patients think that checking the capillary blood sugar value once in the clinic is enough and refuse taking blood for HbA1C. Some patients manipulate the capillary blood sugar value by skipping their meal before the follow up. Since there has been little literature that had studied patient's knowledge and its influence on glycaemic control5, we would like to explore our GOPC patients' knowledge about the different monitoring method in DM control and also about their personal attitude and preference towards the different m Objectives We explored patients' knowledge about the different monitoring methods in DM control and the gold standard monitoring method by HbA1C. Method We used questionnaire survey as the approach to collect our patients' knowledge about their knowledge and preferences. Since there was no similar survey study before nor similar questionnaire available in the literature, we used a focus group to collect the patients' ideas and beliefs to generate a questionnaire. Formation of a focus group and generation of the questionnaire
The focus group was formed under the guidance of a sociologist acting as a moderator
to generate a questionnaire. 8 patients from our 4 GOPCs were selected, with 2 patients
from the following 4 types of patients below, representing patients having different
levels of baseline DM control:
The reason to select different levels of HbA1C and DM control was because we believed that patients with different DM control levels would have different knowledge about DM control and so they were recruited into the focus group. They were encouraged to talk to one another, asking questions, exchanging ideas and beliefs, and commenting on each other's experience and point of view. The whole focus group interview was video recorded. The video was reviewed and transcribed. Some common ideas and questions, unique experience, wrong beliefs and unexpected points of view about the DM monitoring method were noted. By using these information, a questionnaire was generated. The questionnaire was field tested by a small pilot study of 10 patients to check their understanding of the questions. The questions were reviewed according to the field test result to ensure the patients understood all the questions in the questionnaire. Population studied The population we used was the number of Type II DM patients having regular follow-ups in the 4 general outpatient clinics: the Robert Black GOPC (2800), Ha Kwai Chung GOPC (1300), Tung Chung GOPC (970) and Caritas Medical Centre GOPC (1020) correspondingly. The total number of patients followed up in all 4 clinics amounted to 7090. Sampling, case selection and randomisation The sample size was calculated using a 95% confidence level with a confidence interval of 5. The sample sizes were calculated to be 338, 297, 322 and 279 for Robert Black GOPC, Ha Kwai Chung GOPC, Tung Chung GOPC and Caritas Medical Centre GOPC correspondingly. Total number sampled was 1236, which constituted 17% of the total number of diabetes patients being followed up in these 4 clinics. A research assistant would select from Type II Diabetes patients randomly in the waiting area of the clinic and help them to complete the questionnaires after getting their consent. All the sampled patients were successfully recruited within one month's time and they all completed the questionnaire. (See Appendix A) Results A total of 1236 patients were recruited and completed the questionnaire. The average age of the sampled patients was 67 years old and the male to female ratio was 47:53. 1212 patients (98%) had capillary blood sugar monitoring done before their consultation in the clinic. 349 patients (28%) had self-monitoring capillary blood sugar done at home, but most of these were measured in a random manner without a full profile. 1074 patients (87%) had regular HbA1C monitoring. 781 patients (63%) had urine sugar monitoring. Only 33 patients (3%) did not have any DM monitoring by any method. (Figure 1).
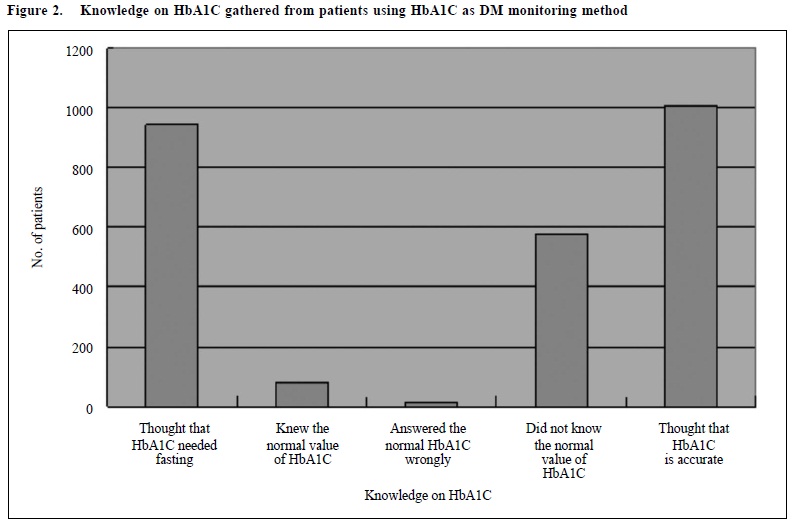
Among the 1074 patients who were regularly taking HbA1C for DM monitoring, only 79 patients (7.4%) knew the correct normal value of the HbA1C. 414 patients (38.5%) answered the normal HbA1C value wrongly and 581 patients (54%) did not know the normal value or did not give an answer. 944 patients (77.9%) had a wrong concept that checking HbA1C needed fasting. Only 24 patients (2%) thought that HbA1C was not accurate. Most of them, 1010 patients (94%), tought that HbA1C monitoring was an accurate method in DM monitoring. (Figure 2)
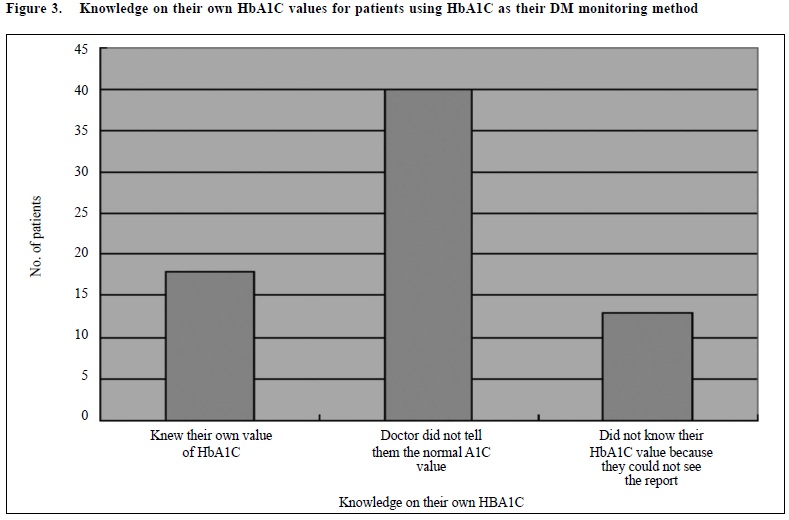
Concerning the knowledge of their own HbA1C values, only 18 patients knew their own HbA1C results and 6 patients could remember their own HbA1C results. The rest of them could not remember or did not know or could not answer what their HbA1C were. 40 of them explained that it was because the doctor did not tell and 13 patients explained that it was because they themselves could not have access to or see the report of the HbA1C value. (Figure 3)
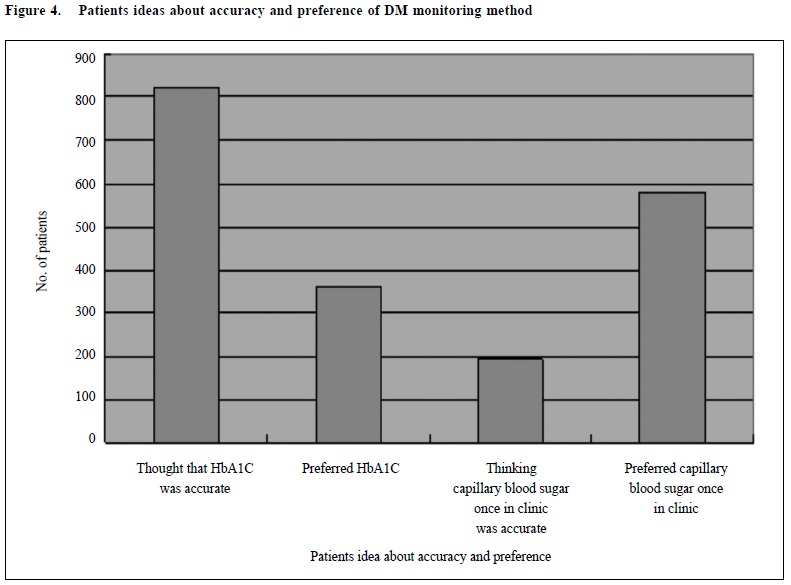
Concerning patient's idea about the most accurate DM monitoring method, most of the patients, 822 patients (67%) thought that HbA1C was the most accurate one, and only 196 patients (16%) thought that checking capillary blood sugar before consultation was the most accurate method. However when asking the patients which DM monitoring method was the most preferred one, surprisingly, most of the patients, 582 patients (47%), preferred capillary blood glucose monitoring and only 364 patients (29%) preferred HbA1C monitoring. (Figure 4)
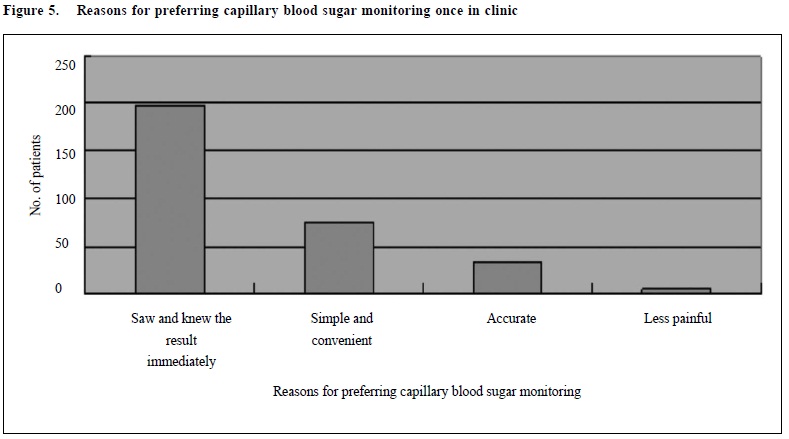
307 among these 582 patients (53%) gave reasons why they preferred capillary blood glucose monitoring more than other DM monitoring methods; most of them, 199 patients (64.8%), preferred it because it was quick to know the result. 76 patients (38.8%) thought that it was simple or convenient. 32 patients (16.1%) thought that it was accurate and 5 of them thought that it was less painful compared to blood taking. (Figure 5)
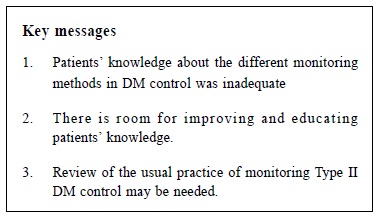
Lastly, 364 patients preferred HbA1C monitoring; most of them, 219 patients (60.2%), said they preferred it because it was accurate. Discussion From this study, we noticed that the most preferred methods of DM monitoring for Type II diabetes patients in our GOPCs were checking capillary blood sugar before the consultation and the HbA1C monitoring. Most of the patients had both monitoring methods during the follow-up. The monitoring method using capillary blood sugar before the consultation is more common than using HbA1C in our GOPCs. This finding reflects the situation that although measuring HbA1C is the gold standard in DM monitoring, it is not the most popular DM monitoring method in the GOPCs. Even though knowing that HbA1C monitoring is the more accurate monitoring method compared to checking capillary sugar once before the consultation, more patients preferred checking capillary blood sugar once before the consultation. It was because the test was quick, simple and less painful method and they could see and know the result immediately. Patients' knowledge about normal value of HbA1C still has room for improvement too. The patients did not know their own HbA1C value was probably because the result was not immediately available after blood taking. Another reason may be due to the patient forgetting to ask the doctor about their own HbA1C value during the follow-up or the doctor did not clearly explain the HbA1C value to the patient. Conclusions In this study, we discovered that there is still room for improvement on the patients' knowledge about DM monitoring methods in the Type II DM patients in our GOPCs. Patients' knowledge about the gold standard method of DM monitoring for Type II DM patients, the HbA1C, is not adequate. The existing method by checking capillary sugar during the follow up is still the most preferred method chosen by the DM patients. However there is no evidence that this method can help us to monitor the DM control of our DM patients. Keeping this usual practice in the clinic may mislead our patients about the gold standard DM monitoring method using HbA1C. As a result, we may need to review whether we should continue the usual practice of checking capillary sugar just once before the consultation. In addition we should provide more education about the HbA1C and encourage them to know and remember the normal and their own HbA1C value. From our research findings, patients preferred capillary blood sugar monitoring because it was simple and convenient and they could know the result immediately. Using capillary blood and measuring the A1C value in the clinic by using a simple kit may be a good method instead of taking venous blood and sending the blood to the laboratory. It may improve the patients' attitude and preference on HbA1C monitoring, and in turn improve patients' compliance and DM monitoing.
Kin-wai Chan, MBChB, MRCS, MDM, FHKAM (Family Medicine)
Associate Consultant Sau-nga Fu, MBBS, MFM (CUHK), FHKAM (Family Medicine) Associate Consultant Ming-pong Yiu, MBBS, FHKAM (Family Medicine) Associate Consultant Yuk-kwan Yiu, MBBS, FHKAM (Family Medicine) Chief of Service Department of Family Medicine and Primary Health Care, Kowloon West Cluster Hospital Authority Correspondence to : Dr Chan Kin Wai, The Lady Trench General Outpatient Clinic, 213 Sha Tsui Road, Tsuen Wan, New Territories, HKSAR.
References
|
|