|
September 2013, Volume 35, No. 3
|
Update Articles
|
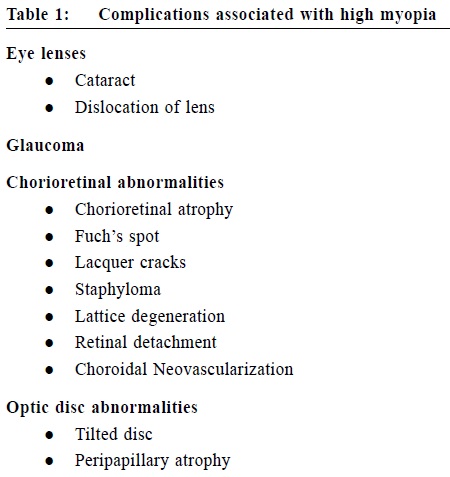
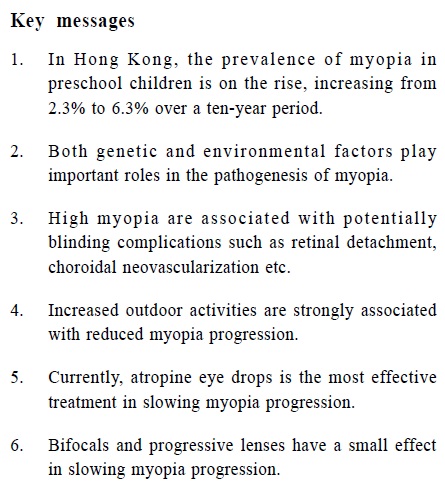
An update on the interventions and strategies in preventing myopia progressionMadeline KM Kwok 郭家雯, Jason CS Yam 任卓昇, See-mei Lee 李詩眉, Alvin L Young 楊樂旼 HK Pract 2013;35:91-96 Summary Myopia is a prevalent eye disease in Hong Kong. Its exact aetiology remains unclear, but genetics and environmental factors are believed to play an important role. High myopia is an important public health issue, because it can be associated with potentially blinding complications such as glaucoma, retinal detachment and choroidal neovascularisation. Increased outdoor activities are strongly associated with reduced progression. Among all the treatment options, atropine eye drops is the most effective therapy. The treatment-associated side effects can be reduced by using a lower concentration of atropine eye drops. Bifocals or progressive lenses also have some small effects. 摘要 近視是香港常見的眼疾,其成因不明,但相信遺傳和環境是重要的因素。 深近視是一項重要的公共衛生議題, 因為它與青光眼、視網膜脫落、脈絡膜新生血管等潛在致盲併發症有關。增加戶外活動與延緩近視加深有密切關係。 在所有治療方案中,阿托品滴眼液的效果最為顯著。與其治療相關的副作用,可以降低滴眼液濃度來減少。 雙焦眼鏡或漸進式眼鏡也對延緩近視加深稍有作用。 Introduction Myopia (near- or short-sightedness) is one of the commonest human eye diseases and often has its onset during childhood. It is defined as a refractive state where light rays entering the eye focus in front of, rather than, on the retina. In East Asia, myopia has become a major health issue due to its increasingly high prevalence rates.1 In Hong Kong, the prevalence of myopia in preschool children is on the rise, increasing significantly from 2.3% to 6.3% over a ten-year period.2 Family physicians are often approahed by anxious parents for advice regarding their children's myopia. There is a confusing array of management options available in the market and on the internet. The purpose of this article is to review evidence on available interventions and strategies, facilitating family physicians to provide the appropriate advice to patients and their families. Definitions & biologic basis Myopia can be divided anatomically into axial and refractive, or clinically into simple (or school) and pathological (or degenerative). In anatomical terms, axial myopia is a result of an elongated eyeball. Refractive myopia is further subdivided into (i) index myopia where there is/are variation(s) in the refractive index (-ices) of one or more ocular media, and (ii) curvature myopia where there is/are exaggerated curvature(s) of one or more surface(s) of the eye, especially the cornea. Clinically, simple myopia normally refers to those with myopia ranging from 0 to 6 dioptres (D). Locally, in Hong Kong, 1D is conventionally referred as 100 ‘degrees' in the optical shops while pathological myopia refers to those with myopia of greater than 8D. At birth, most babies are slightly hyperopic. In the first two years of life, this hyperopia gradually decreases in an active process called emmetropization of the eye. After that, the cornea stabilises but myopia can continue to progress as the eyeball lengthens over the next two decades.3,4 Myopia generally develops in early and middle childhood but can well progress into the late teenage years or even young adulthood.5 A recent study in Chinese eyes have demonstrated that children's refractive error at the age of 11 years were already similar to their parents and the estimated myopia in these children by the age of 18 would be up to 2.0D more severe than their parents.6 Pathogenesis Despite a long history of scientific research and significant interest in the causes of myopia in the past three or more decades, the exact aetiology remains to be elucidated. There are, however, many postulated theories, with genetics and environmental factors being the two most studied. The genetic theory for myopia is based on familial clustering. Sibling risk ratios are high in myopia and even higher for pathological myopia.7 However, sibling similarities may also be contributed by exposure to the same myopigenic environmental factors.8 It is also consistently found that children with myopic parents have a higher prevalence of myopia but the relative risk varies substantially. In areas where the prevalence of myopia is high, such as East Asia, the relative risk is found to be lower.9 Several recent reviews suggested a list of genes to be associated with myopia. In syndromic high myopia, the participation of genes involved in scleral extracellular matrix is a common feature. However, for non-syndromic high myopia, a large number of chromosomal localizations have been reported but few specific genes have been identified. At present, the number of genes associated with variation in refractive error among school myopia account for only a small proportion of the variations.10 Thus, school myopia is faced with a mismatch between the high heritability defined in twin studies and defined associated allelic variations, a common problem in complex disease genetics known as missing heritability.11 All these findings imply genetics to be only one of the many contributions to myopia development. The importance of environmental risk factors for myopia development stems from animal experiments. Human observational studies have also consistently demonstrated an association between myopia and education level, number of years of schooling and school results.12 In addition, the role of accommodation to myopia development has been a long-debated and controversial issue over the past century. Some studies demonstrated an association between the duration of near work and myopia while others showed weak evidence to support a significant effect of near work to induce myopia.5,11 These conflicting results led to the postulation that sub-optimal accommodation during near work, known as accommodative lag, creates hyperopic defocus on the retina, which in turn stimulates axial elongation of the eyeball. However, the literature has yet to prove whether myopia is a cause or result of accommodative lag. Complications of myopia Myopia is associated with pre-senile cataract and glaucoma, though the pathology of these associations remains unclear. In addition, pathological myopia is associated with characteristic degenerative changes of the sclera, retinal pigment epithelium and choroid, and is a major cause of visual impairment. The degenerative changes are principally thought to be related to mechanical stretching of the involved tissue as the eyeball lengthens. Table 1 shows a list of the possible complications associated with high myopia.
In the urban centres of East Asian countries, the overall prevalence of myopia and pathological myopia in children of school-leaving age are now several times higher than those in the older cohorts.12-14 The increased prevalence of pathological myopia will become a major public health and economic burden, as a result of the resulting rise in related complications. Interventions A) Outdoor activities Many studies have reported a protective effect of increased time spent on any outdoor activity against myopia development.15-17 Lower myopia was consistently found in children who have increased time spent outdoors. The true biological explanation for this protection remains to be elucidated. Some postulated mechanisms include light intensity, dopamine release and vitamin D.15 These hypotheses require further systematic testing in future studies. B) Pharmacological Atropine eye drops Atropine is a non-selective muscarinic receptor antagonist and is now the most commonly used drug in slowing myopia progression. The postulated mechanism includes inhibition of accommodation, biochemical remodelling of sclera, and increase ultraviolet exposure secondary to pupil dilatation.18 The Atropine in the Treatment of Myopia Study (ATOM) was a randomised, double-masked, placebo-controlled trial involving 400 Singapore children.19 This study showed that the instillation of 1% atropine eye drops nightly in 1 eye over a 2-year period significantly reduced myopia progression by 77% (0.28D vs. 1.2D in control vs. atropine groups). Axial length elongation was also significantly reduced with this regimen (0.38+0.38 mm vs. -0.02+0.35 mm in control vs. atropine groups). However, discontinuation of treatment was shown to cause a partial rebound effect. This regimen was also shown to reduce myopia progression significantly by 35% over a 3-year period (2 year atropine treatment followed by one year no treatment).20 The main side effects of atropine include photophobia due to mydriasis and decreased near vision due to cycloplegia. As a result, patients on treatment were required to wear photochromatic, progressive additional lenses. No systemic side effect related to atropine was reported but postulated side effects include dry eye, dry mouth, dry throat, flushed skin, constipation and difficulty with micturition. Other ocular side effects such as allergic conjunctivitis and eyelid contact dermatitis are relatively uncommon. There was no significant retinal dysfunction 3 months after cessation of the eye drops. The ocular side effects mentioned above prohibited wide adoption of atropine use internationally. However, recent trials with lower doses of atropine (e.g. 0.5%, 0.1%, 0.01%) were associated with fewer side effects and demonstrate significant reduction of myopia progression.18 This led to a resurgence of its interest in Hong Kong. In view of the current evidence, atropine eye drops remain the most popular treatment option chosen by general ophthalmologists and paediatric ophthalmologists in both the public and private sector to retard myopia progression. Before starting treatment, the parents need to be well-informed of evidence of the therapy and the associated side effects. A good doctor-parent rapport and parental commitment are the key factors for treatment compliance. Currently, the predominant commercially available topical atropine in Hong Kong has a concentration of 1%. Patients are instructed to instil the eye drop once nightly to both eyes and are monitored every 4-monthly. Combined photochromatic and progressive glasses are prescribed daily for these patients to prevent ultraviolet-light damage to retina and to improve near vision. Pirenzepine 2% Eye Gel Pirenzepine 2% gel is a selective M1 / M4 antagonist which produces less mydriasisand cycloplegia than atropine. Twice daily application can reduce myopia progression by 50% over 12 months.21 A common side effect is allergic conjunctivitis, which can occur in up to 50% of patients. Other ocular side effects and systemic side effects are uncommon. However, pirenzepine 2% eye gel is not yet commercially available for use. Thus this treatment is not available in Hong Kong. C) Optical Under-correction with spectacles Based on animal studies, emmetropization was shown to be an active process, mediated by optical defocus. These studies suggested that placement of a positive lens in front of the eye causes myopic defocus, which in turn slows axial elongation and thickens the choroid. Conversely, placement of a negative lens in front of the eye causes hyperopic defocus and accelerates axial elongation and thins out the choroid.22 It was thus speculated that full-correction of myopia in children could promote axial elongation, thus myopia progression. However, studies comparing myopia progression in fullyand under-corrected myopic children with spectacles or single vision lenses (SVL) have produced conflicting results. And so this therapy is not a common practice by ophthalmologists in Hong Kong. Bifocals or progressive addition lenses Bifocal or progressive addition lenses have two or more distinct optical powers. They are commonly used in people with presbyopia such that their vision is not jeopardised with reduced accommodation. The rationale for using bifocal or progressive addition lenses to correct myopia in children was based on the benefit of reducing defective accommodative effort, which was speculated to improve retinal image quality in those with high accommodative lag. This was thought to prevent potential aberrant eye growth. In a 30-month randomised controlled trial (RCT) involving 82 children with near point esophoria, the use of bifocals to correct myopia was found to have a small but significant benefit in retarding myopia progression.26 RCTs on the use of progressive addition lenses to correct myopia suggested either no effect on myopia retardation or a minor but significant effect in the first year only.27,28 Based on these findings, it is concluded that the use of bifocals or progressive lenses to correct myopic children has little effect (-0.50D at most) on myopia retardation and this effect is probably too modest to warrant a change from the use of single vision lenses to bifocals or progressive lenses. This therapy is a common practice by optometrists in Hong Kong. D) Use of various types of contact lenses The rationale for using contact lenses (CL) to correct myopia stems from the beliefs that they can flatten the cornea, retard axial elongation and reinforce the sclera, which was postulated to in turn retard myopia progression. A RCT of 175 children showed that the use of soft CL did not have any significant effect in retarding myopia progression when compared with spectacle use.29 The use of rigid gas permeable (RGP) CL in a small, non-randomised trial demonstrated reduction in myopia progression when compared with spectacle wear but the effects were accounted for by corneal flattening only.30 Conversely, a large RCT involving 428 children failed to show any significant benefit with the use of RGP CL when compared with spectacles in myopia retardation.31 Orthokeratology lenses (OKL) is a type of RGP CL that temporarily reshapes the cornea. It differs from other CLs in that it is commonly worn at bedtime and removed upon awakening. It is particularly appealing to parents who want their children to be spectacle-free during the day. In addition, its use was postulated to have an effect on myopia retardation from peripheral myopia defocus, which acts as a signal to dampen eye growth and axial elongation. Many studies on OKL were carried out but few if any to date have definitively demonstrated the reduction in myopia progression to be permanent.32,33 The hypothesised permanent benefits with the use of OKL in myopia retardation have yet to be proven scientifically. Unfortunately, complications, some of which are serious and blinding (such as recurrent corneal erosion, infective keratitis, induced corneal astigmatism, corneal pigmentation) are associated with its use.34-36 This is a common practice by optometrists and some private ophthalmologists in Hong Kong. This therapy is not available in the public sector. However, the authors cautioned that the risks associated with OKL must be carefully weighed against the possible benefits. Parents should be counselled adequately and made aware of these potentially blinding complications that may arise from its use. Immediate medical advice should be sought when there is any symptom of keratitis, such as pain, redness, and blurring of vision. Conclusions Myopia in children is a rising threat in Hong Kong. High or pathological myopia gives rise to potentially blinding complications that will be a burden to the health care system as well as the economy. To date, the only interventions that had been shown to be of scientific benefit are increasing outdoor activities and the use of topical atropine and pirenzepine. Myopia correction using bifocal or progressive addition lenses were also found to reduce myopia progression; unfortunately, effects were only temporary and at most modest. Other strategies including the use of CL revealed equivocal or only temporary effects in myopia retardation. In order to stem the tide of this potential myopic ‘epidemic', perhaps we too may ask our Hong Kong families and schools to consider the Singaporean Health Promotion Board motto: ‘‘Keep Myopia at Bay, Go Outdoors and Play!'
Madeline KM Kwok, MBChB, MRCS(Ed), FCOphthHK, FHKAM(Ophth)
Resident Hong Kong Eye Hospital Jason CS Yam, MBBS, MPH, FRCS(Ed), FHKAM(Ophth) Assistant Professor Department of Ophthalmology and Visual Sciences, The Chinese University of Hong Kong, Prince of Wales Hospital & Alice Ho Miu Ling Nethersole Hospital See-mei Lee,, MB BCh BAO, DPD, DFM Private Practitioner Dr George Medical Clinics Alvin L Young, FRCS (Irel), FCOphthHK, FRCOphth, FHKAM (Ophth) Chief of Service and Cluster Coordinator Department of Ophthalmology and Visual Sciences, The Chinese University of Hong Kong, Prince of Wales Hospital & Alice Ho Miu Ling Nethersole Hospital Correspondence to : Dr Alvin L Young, Chief of Service and Cluster Coordinator, Department of Ophthalmology and Visual Sciences, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, Hong Kong. SAR Email: youngla@ha.org.hk
References
|
|