June 2014, Volume 36, No. 2 |
Discussion Paper
|
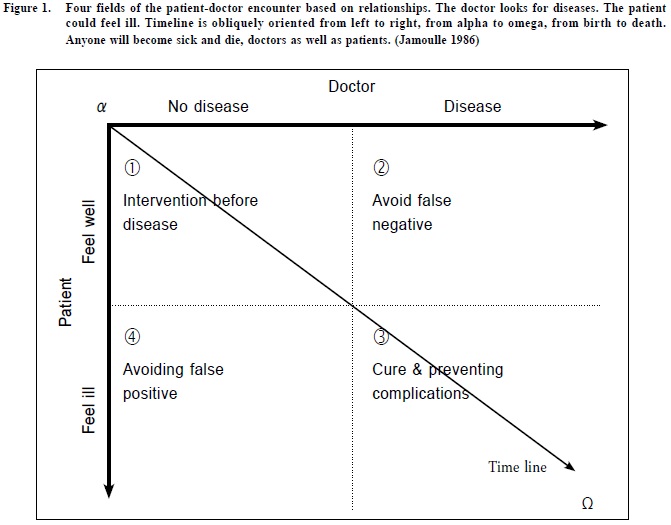
The four duties of family doctors: quaternary prevention – first, do no harmM Jamoulle HK Pract 2014;36:72-77 This short article is a revised and updated version of a keynote to the annual congress of The Portuguese Association of General Practice/Family Medicine (APMGF), Covilhã, Portugal; September 2013. Summary Clinical prevent ion has been organised in a chronological manner since the middle of the 20th century. A paradigm shift from a chronological to a relationship-based preventive pattern of care offers new insight into the practice of doctors, and brings to light the concept of quaternary prevention, a critical look at medical activities with an emphasis on the need not to harm. Quaternary prevention addresses the fundamental question of what constitutes too much or too little medicine. It is the fourth form of disease prevention, but also the fourth frame of action for family doctors. New definitions of prevention published in the Wonca Dictionary of Family Medicine offer a structured way to discuss the activities of family doctors, including ethical considerations on the patient-doctor encounter. 摘要 從20世紀中期開始,疾病預防是按疾病的發展過程分類。(包括三階段:1. 預防疾病萌生;2. 在病徵出現前及早診斷及3. 在治療和康復期間預防併發症和後遺症發生。)由以往「時序」模式轉為基於醫患「關係」模式分類可引伸對醫務工作的更深入了解,和帶出「第四類預防」的概念。(第四類疾病預防是避免因醫生態度、醫療過程或信息傳遞,不經意地令病人產生或增加對患病的憂慮和恐懼。)這裡需要以不損害病人為宗旨,客觀地、批判地檢視病人的各種醫療程序和需要。它涉及到過份醫療介入或處理不足的基本問題。這第四類疾病預防的領域也是家庭醫生在日常工作上需要自覺和自律的範疇。最新刊登在<<Wonca(世界家庭醫生組織)家庭醫學詞典>>的「預防」定義,提供了討論家庭醫生工怍,包括醫患間道德考慮的切實途徑。 Background: always too much wrong medical practice From the 1950s onwards, the sheer amount of medical specialties, pathologies and technologies has inexorably increased. The Diagnostic and Statistical Manual of Mental Disorders has recently published its fifth edition1 and now lists more than 350 “conditions”. It is well known that some new conditions have been added under the pressure of powerful pharmaceutical lobbies.2 The general idea is: we are all sick, and we are all somewhat crazy.3 More importantly than the simple number of diseases, the change from asymptomatic conditions and risks to diseases4, as well as indirect pressure on medical doctors5-7, have had an impact on the way the management of medical activities has mutated. Hypertension, hyperglycaemia, hypercholesterolaemia and being overweight are usually asymptomatic conditions. Patients do not perceive themselves to be ill, until a Good Samaritan comes along to tell them that they are. Lipid reducers are now seen as more protective than the Sacramental bread, and represent the biggest share of our collective insurance expenditure. We know that we have to treat 1,000 patients with hyperlipidaemia for five years in order to avoid only 18 severe cardiovascular events.8 Disease mongering (the creation of new diseases) also summons psychological manipulation9 by using the same techniques to market diseases as than those already used for brands.10 Such techniques are referred to as “branding condition”. The statistical thresholds of biological markers are computed with population data, which are consequently inadequately applicable to a single patient11,12 in a context of institutional corruption.13,14 Therefore, we can conclude that we stray away from intensive medicalisation as announced by Illich15 and explained by Conrad16, and are getting closer to “dys-medicalisation”, or wrong medicine. Since norms and regulations are identified by committees of experts, which are tightly linked with pharmaceutical and technological companies behind well-hidden doors17-20, entire fields of medicine are over-practiced. Some disease categories are flourishing under such circumstances. Osteoporosis, menopause, erectile dysfunction or social phobia21 are examples of such fabricated markets.22 Big Pharma is not the only player to blame for this disaster. Post-war period screening programmes have vastly expanded, notwithstanding their good intentions and the fury to abide by “Prevention is better than to cure”. The systematic application of evidence-based medicine is now challenging this paradigm. A textbook example is preventive mammography, which leads to the overdiagnosis of cancer23, and makes practitioners doubtful about the best course of action to adopt for their patients.24 These mammograms command doctors to go a step further in the process of informed decision making.25 The same can be said about flu vaccination26 or the HPV vaccine27 while mass prostate cancer screening is not recommended anymore.28 Furthermore, emotional discomfort and psychosocial distress could be quickly medicalised under vague diagnoses, which are nothing more than the admittance of medical limitations and poorlyframed evidence. There is now documented literature on MEDLINE indexed under useless keywords such as “non-disease disease29,30”, somatisation and functional somatic syndrome31, which yield articles with a plethora of statistical thresholds and arbitrarily-determined rates which are now the norm to create a market. Dealing with clinical prevention From communicable diseases to managed care: the mainstream of general practitioners Clinical prevent ion could be considered as managing a certain care process over time in a patient’s life. The overemphasis of clinical prevention is a fairly recent phenomenon. The over-development of the prevention concept is a result of the extensive use of the diagnosis concept. Until the beginning of the 20th century, prevention was a time based practice purely related to public health, and dealt with the understanding and control of communicable diseases.32 Prevention, time and disease-centred care The term primary prevention was coined in the late 1940s by Leavell & Clark33 and was used to describe “measures applicable to a particular disease, or group of diseases, in order to intercept the causes of disease before they involve man”. Secondary prevention consists of a set of measures used for early detection and prompt intervention to control a problem or disease and minimise their consequences, while tertiary prevention focuses on the reduction of further complications of an existing disease or problem, through treatment and rehabilitation34 but this distribution has been blamed for inconsistencies.35 Prevention, relationships and patient-centred care In 1986, the author has proposed crossing science and conscience to establish four distinct nebulae36 based on patient doctor relationship. The term ‘nebula’ is used because the limits between health and illness, and between health and disease, are not clearly defined. Science determines whether or not a disease is present, most often a sharp distinction, while patients make a distinction between feeling sick and well on progressive or fuzzy basis. When creating four boxes based on the relationship between provider and patient, one immediately notices that the disease development timeline is obliquely oriented from left to right, from birth to death. Anyone will become sick and die, doctors as well as patients. (Figure 1 from alpha to omega)
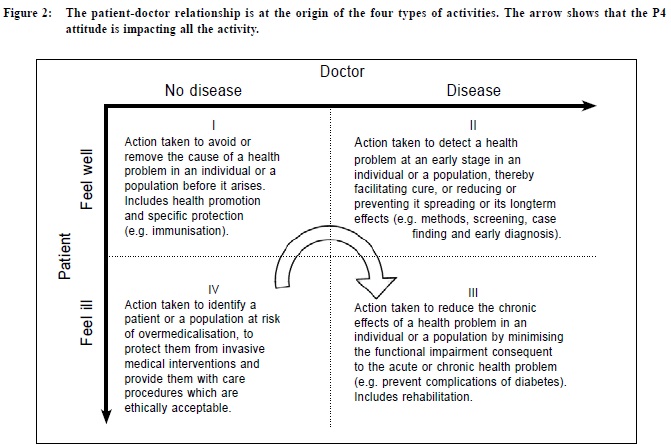
If the patient is in good health, or feels healthy, and their doctor cannot find anything wrong with them, it forms the perfect context to adopt a primary preventive attitude such as immunisation or health education. The objective of screenings and secondary prevention is to discover an illness among individuals who feel healthy, such as cancer screening or STD testing. Once patients and physicians mutually realise the presence of a problematic health condition, they move to the curative field. Diabetes, high blood pressure, Lyme disease, positive Chagass serology and cardiopathy must, of course, be treated. A critical eye is then cast on the medical act itself, and complications need to be avoided. Moreover, these long-term illnesses will lead to a new phase in which the doctor will suggest rehabilitation. A reduction of complications, in addition to rehabilitation, defines tertiary prevention. The fourth type of prevention is the least intuitive. The patient feels sick, the doctor is asked to find the problem. Doctors are supposed to detect false positive cases. But they are also prone to create false positives by lack of attention, lack of listening, lack of knowledge, inadvertence, anxiety, defensive behaviour or interest. Any uncontrolled or unconscious medical act could throw the patient into the fourth field. It is not rare that the usual consultations encompass most often actions in more than one field at a time in a context of comorbidity.37 And so the fourth field emerges. The patient is scared and suffers, but science is of no help. It is a field of disbelief and often of scorn. It is often the result of fears being medicalised. It is why we have Monday-morning invasions of people complaining about their heart because they came across a website or watched a television programme on cardio-pathologies the previous evening, women who have cancerophobia as a result of all the messages they hear on breast cancer, and ‘normal’ patients pathologising everything that deviates from ‘normality’. It is clear that the medical practice can be the cause of serious issues, whatever the sector: primary, secondary or tertiary. This relational view fits perfectly within the Wonca definitions of prevention The first three forms of prevention were defined in 1995 by the Wonca International Classification Committee in the Glossary of Family Practice.38 These 3 definitions are perfectly adapted to the field they qualify. It is now evident that the need for a fourth definition of prevention is of interest to primary care. Using the other definitions as models, the author has proposed the following definition at a meeting of the Wonca International Classification Committee in Hong Kong in 199539: “Action taken to identify a patient or a population at risk of over-medicalisation, to protect them from invasive medical interventions, and provide them with care procedures which are ethically acceptable.” This definition was adopted by the Wonca International Classification Committee during its Durham meeting in 1999 and has been published in the Wonca Dictionary for General Practice / Family Practice.40 When placed in the four-fold table, the definitions - including the fourth one - fit perfectly (Figure 2). This table is particularly effective when teaching prevention to students. They never forget the contents of the boxes.
One could read the boxes forgetting the term ‘prevention’ and considering the four fields to be a doctor’s fields of actions, whereby the third one is curative with a focus on complications and on the rehabilitation process. The table reflects the duties of the general practitioner throughout a patient’s life. This is the basis of integrated care, which recommends mixing curative care with preventive care. It is normal practice for a general practitioner / family physician to care for angina (Field III), to ask about the patient’s smoking habits (Field I), to measure the sugar level because the patient is diabetic (Field III), to inquire if she had a Pap smear this year (Field II), and, at the same time, help her overcome her anxieties by listening to her attentively (Field IV). Quaternary prevention: A field of intervention Quaternary prevention, based on relationships, includes scrutinising all the continuous interventions doctors make to treat their patients, as well as controlling their own anxiety and lack of knowledge. In this sense, applying evidence-based medicine (EBM) guidelines belongs in the fourth field. The quaternary field is where patients and doctors are lost. To avoid being trapped in this field, measures are needed. Medical students have to be taught how to deal with a patient's concerns and how to control their own doubts. Doctors have to implement quality assurance measures, learn how to apply EBM guidelines, and identify disease mongering. They also have to learn that sometimes, even though it may be difficult, it is better to do nothing rather than to pursue useless investigations trying to find a rare condition. Measures need to be taken in order to avoid patients slipping into the fourth one. Poor information from the Internet is a source of anxiety and unjustified demand for care. Screening for prostate or breast cancer can throw the patient into the fourth field if he or she becomes cancerophobic. A puzzling note in a treatment protocol can also trigger patient anxiety. Therefore, adequate training for doctor behaviour, communication and practice is needed in order to avoid causing unnecessary distress. The shift from time-based prevention towards a relationship-based one offers new perspectives into a physician’s work. He or she observes himself / herself, and questions the ethical limits of their activities. In this sense, quaternary prevention is aimed more at the doctor than the patient. International impact of the quaternary prevention concept Quaternary prevention, also known as P4, is a new term for an old concept: first, do not harm. Disseminated by the colleagues of the Wonca International Classification Committee (WICC), the P4 concept is now widely recognised in Europe and South America and is on its way to Asia. Astonishingly, quaternary prevention has lain dormant for two decades. With the expansion of Internet and social networks, family doctors are now recently jostled with the idea. First launched in Brazil during the Conference for the 20th Anniversary of the Brazilian Primary Care System (2008), P4 has provoked the emergence of numerous groups in Argentina, Uruguay, Peru and Bolivia. In Europe, Spain and Portugal have been hit first followed by France. Following the Quaternary Prevention Workshop during the Wonca Europe Basel Conference in 2010, the Swiss journal Primary Care has published a paper on P4 in 6 languages.41 During the Wonca World Conference in Prague in 2013, a P4 seminar was organised with speakers from New Zealand, China, Pakistan, the UK and Belgium42 and a poster was translated in French, Spanish, Portuguese, Vietnamese and Thai.43 After the 2013 Curutiba Meeting in Brazil, members of the Brazilian P4 group have written the Curutiba Manifesto on quaternary prevention, soon available in English.44 The enthusiasm generated around this topic shows that the P4 concept is used as a framework for a multifaceted repositioning of current questions and limitations of medical practice: disease invention, Attention Deficit Hyperactivity Disorder (ADHD) Quaternary prevention involves the need for close monitoring by the doctor himself, a sort of permanent quality control on behalf of the consciousness of the harm they could, even unintentionally, do to their patients. Quaternary prevention is about understanding that medicine is based on a relationship, and that this relationship must remain truly therapeutic by respecting the autonomy of patients and of doctors. P4 attitude acts as a resistance, a rallying cry against the lack of humanity of whole sectors of medicine and their institutional corruption.13
M Jamoulle, MD Correspondence to: M Jamoulle, marc.jamoulle@doct.ulg.ac.be For information about quaternary prevention-related events, links, bibliography and slides, refer to the Wonca International Classification Committee website www.ph3c.org under the Quaternary Prevention rubric. References
|
|