|
June 2014, Volume 36, No. 2
|
Update Article
|
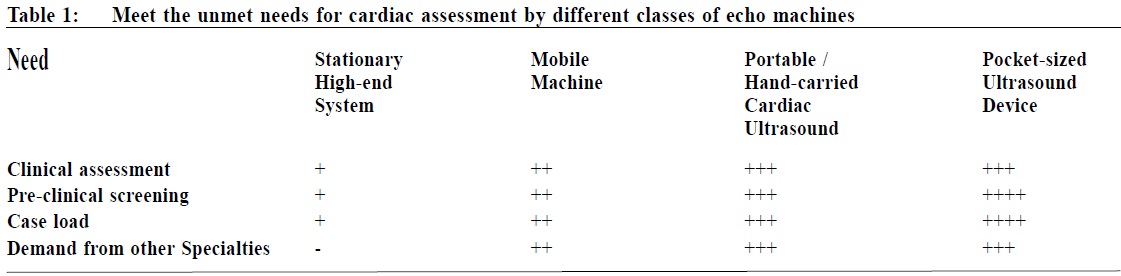
Hand-carried cardiac ultrasound in clinical practice: meeting the unmet needKwok-fai Leung 梁國輝 HK Pract 2014;36:61-65 Summary Former studies have demonstrated that echocardiography improves diagnostic accuracy. In the last few years, the miniaturisation of echo machines has made screening of patients at the bedside possible. Furthermore, these pocket-size ultrasound devices can be carried in a doctor’s white coat. They offer diagnostic real-time quality 2D and colour doppler imaging. This review serves to highlight the current unmet needs in the care of cardiac pat ients and illustrates how these devices can potentially help in clinical practice. The current evidences supporting their diagnostic performances in different setting will be updated. The training requirement and future appl icat ions of hand-car r ied cardiac ul t rasound including pocket-size ultrasound devices will also be discussed. 摘要 以往研究顯示超聲波心動檢查能提高診斷的準確性。在近年,因迴聲器械微型化,我們可用儀器在床邊為病人進行篩選檢查。再者,這些口袋大小的超聲波設備可攜帶在醫生的白袍內,它能提供實時高質素的2D和彩色多普圖像診斷。本述評指出現時在心臟病診斷上不足之處,並說明這些儀器在臨床應用的潛力。本文同時闡述這些儀器在不同環境下診斷功能的最新正面實據。本文亦會討論手提心臟超聲波儀器(尤其是口袋型超聲波儀器)在培訓上的要求和未來的方向。 Introduction Four unmet needs in clinical practice Many studies1,2 have demonstrated that auscultation often overlooks or erroneously interprets findings, resulting in missed or incorrect diagnoses. For example, the audibility of mild mitral regurgitation murmur is just less than 20%.3 Many factors affect audibility, including obesity, chronic lung disease and depressed left ventricular (LV) systolic function. Some patients with severe mitral regurgitation may only have a soft murmur during acute heart failure states. Even with the advances in the development of an electronic stethoscope, as compared with conventional stethoscope, the agreement rate among clinicians is still low.4 There is therefore a need to have a better bedside diagnostic tool for cardiac assessment (Table 1).
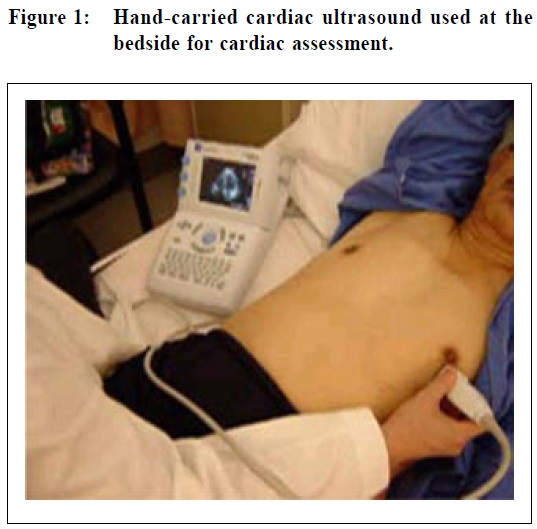
Such a tool needs to be cost-effective in identifying at risk populations before their disease becomes advanced, since the presence of physical signs already indicates advanced stages of heart disease. Suspicion of cardiac disease often prompts referral for a comprehensive echo, potentially creating a long waiting time.5 Simple bedside technologies at a primary care physician level may help to lessen secondary healthcare burden. Advances in echocardiography – smaller and smaller The first echocardiography machine introduced by Hertz and Edler in 1953, was very large and heavy. With the revolution in electronics, echocardiography has become much more portable in the recent 20 years. Modern echo machines can be classified into 3 systems according to size and function; (a) stationary high-end, (b) mobile or portable, and (c) hand-held.6 Stationary high-end systems provide comprehensive and advanced functionalities in echocardiography. However, because of its large size and cost, they cannot be made available to every patient in the ward or clinic, nor can it be used for pre-clinical screening. Mobile systems are smaller machines on wheelsthat can provide a full range of standard echo modalities and measurements. Bedside clinical assessment is possible, but its high cost is a stumbling block for wider applications. With its limited availability, its use in pre-clinical screening is also restricted. Battery-powered hand-held systems are small and lightweight, allowing full portability both within and, for the first time, outside the hospital setting. In the past, they could only provide 2D and colour mode, but nowadays most of them can offer all essential modalities to perform a comprehensive echocardiography study (Figure 1).
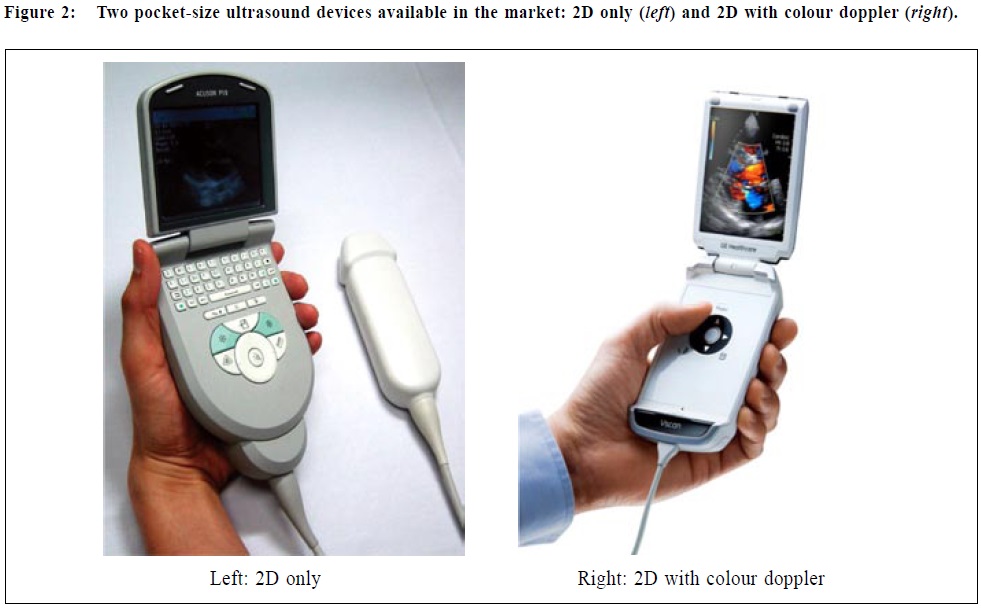
The hand-carried cardiac ultrasound (HCU) can help rule in, or out, specific conditions within a few minutes. Plenty of evidences support the use of HCU in clinical practice7,8,9 HCU has been shown to be the most cost-effective strategy for LV systolic function assessment in terms of pre-clinical screening.10 It is also very valuable for screening of left ventricular hypertrophy in hypertensive population11, abdominal aortic aneurysm12, and hypertrophic cardiomyopathy in the pre-participation athletic examination13. Other than cardiac application, HCU connected to different transducers can perform many varieties of tasks including superficial or organ-specific biopsy, vascular, musculoskeletal, nerve, trans-cranial, thoracic and abdominal, obstetric and gynaecological, paediatric and neonatal applications. However, although HCU is less costly as compared with the high-end or mobile system, the current price of the device is an obstacle to physicians purchasing them for their personal use, leading to its sporadic use in clinical practice. Pocket-size ultrasound devices (pUS) pUS is a new generation of echo has been developed over the last 5 years. The two available pUS in the market (Figure 2) are as small as the size of mobile phones, allowing these devices to be carried in one’s white coat for the first time, facilitating true bedside routine use. Moreover, the price is more affordable for the primary care clinical settings.
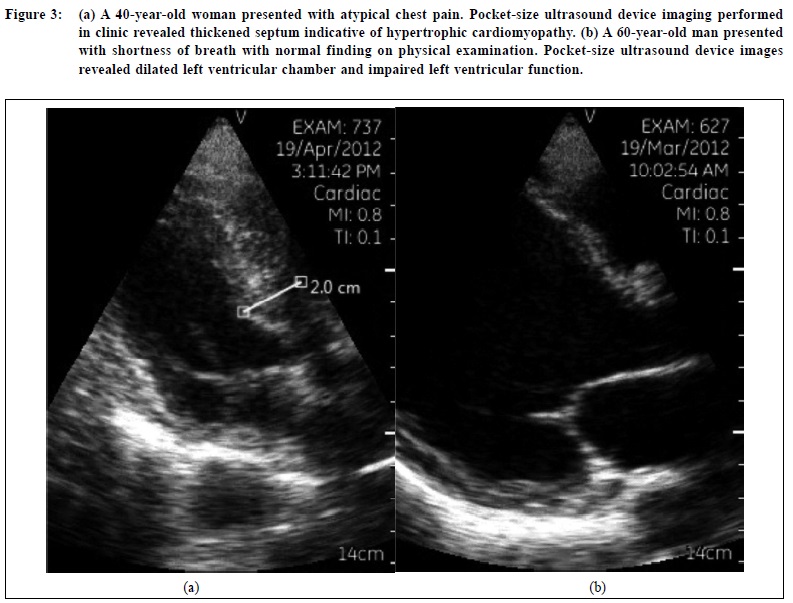
Strictly speaking, pUS is not an echo machine. However, their technical characteristics and image quality are usually sufficient for qualitative evaluation of basic cardiac assessment14, providing image qualities that are comparable to high-end systems. Only in patients with very poor echogenicity does high-end machines provide better image qualities. In patients with pericardial effusion, the pathology is somewhat more difficult to illustrate with the narrow sector of pocket-size device. There is very good agreement in the simple cardiac chamber linear measurements and concordant evaluation of regional and global left ventricular function as compared with high-end systems. pUS could capture all cases of pericardial effusion and valve stenosis. Valves regurgitation was mildly overestimated by pUS, with overall good concordance in detection of regurgitation using colour doppler. With the use of pUS in a cardiac ward setting (usually with suboptimal environmental condition) 16% of patients can have their diagnoses correctly confirmed15, 29% had the primary diagnosis verified, and 10% had an additional important diagnosis made. Therefore, a correct and comprehensive diagnosis could be made with possible favourable outcomes, less time delay and hence lessens a patient’s suffering. The older the patient, the higher the chance that pUS could influence the diagnosis. If pUS is used in the clinic for every new patient, the diagnostic performance for detecting cardiac abnormalities could be enhanced by 32% (35% and 30% by experts and trainees respectively).16 Just an addition of 5 minutes to perform pUS exam for all new patients in the cardiac clinic, some unexpected findings such as hypertrophic cardiomyopathy may be revealed (Figure 3a).17 Patients with flow murmurs can be discharged at their first cardiac clinic visit with the aid of pUS screen. Medical therapy can be commenced for newly diagnosed heart failure during the same initial visit instead of waiting for the results of a formal echo a few months later (Figure 3b).
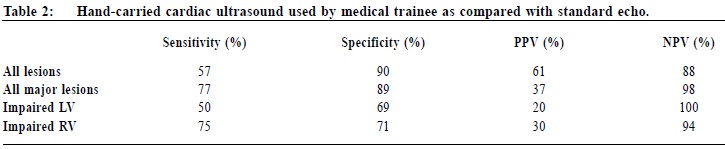
Such benefits would undoubtedly increase both patients’ and physician’s satisfaction. On the whole, pUS could modify the decision of whether to send a patient to the echocardiography laboratory. In a study from Nuno Cardim et al17, normal result on pUS increased discharge from cardiac clinic without need for further testing by 20%. After physical examination, 50.3% of patients were referred for echo, but this figure was lowered to 33.9% after pUS. Importantly, it enabled physicians to detect depressed LV systolic dysfunction and inaudible valvular disease that were not suspected clinically and thus for which full echo was not contemplated. Therefore, this new generation of ultrasound device, with its portability, user-friendly interface and affordability, has very great potential to supplement the clinical assessment, pre-clinical screening and triage of patients. Training and quality assurance With its versatilities, training for doctors from other specialties can be further broadened. They may include internists, emergency care physicians, anaesthesiologists, family physicians, or even medical students and nurses. The question is how can training be accomplished? American Society of Echocardiography in 2002 recommended level 2 competence before using HCU18, which includes performing at least 150 and personally interpreting 300 examinations respectively. To many non-cardiac doctors, it is almost impossible to attain such intensive training, and so a tailor-made training programme to help other specialists to build-up their focused cardiac ultrasound capability is essential.19 In our department, we had a long history of training our residents while they rotate to our team to perform focused echocardiography. Their capability was very valuable to help us triage patients, especially in ruling out major cardiac abnormalities (Table 2).20
Starting from October 2011, we had initiated a new and formal training programme specifically for use of the pUS. We taught and monitored image acquisition techniques, basic measurements, use of colour doppler to assess valve regurgitation severity and interpretation. We also organised two hands-on workshops to share our experience on using hand-carried ultrasound with specialists from other disciplines. Future training should be formal and involving a mandatory certification process. This appears to be the only way to avoid abuse and potential harm to patients due to both over-and under-diagnosis of serious heart disease. I believe that the more empowered and informed a physician is at the point of care, the more effective is the rendition of care. Conclusion Hand-carried cardiac ultrasound including the new pocket-size ultrasound devices can be used to complement physical examination in an out-patient setting, as well as for screening programmes in schools and communities. The capability and simplicity of these new pocket-size ultrasound devices may make it the new equipment in a doctor’s bag, becoming an extension of the physical examination and providing a ‘window to the heart’ that is unmatched by the physical examination alone. Such an accomplishment will significantly improve our service to our patients and help us further combat cardiovascular disease.
Kwok-fai Leung, MBChB(CUHK), FRCP (Glasg), FRCP (Edin), FHKAM (Medicine) Correspondence to: Department of Medicine and Geriatrics, United Christian Hospital, 130 Hip Wo Street, Kwun Tong, Hong Kong SAR, China. References
|
|