|
September 2014, Volume 36, No. 3
|
Case Report
|
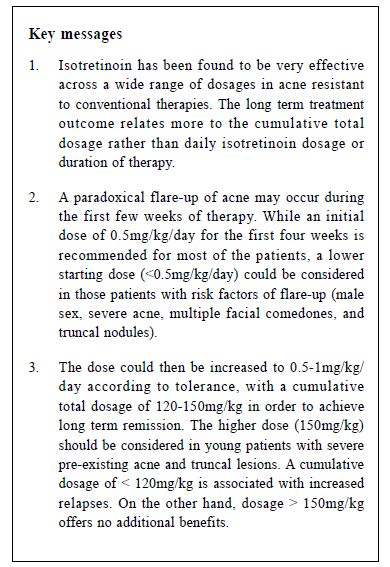
Isotretinoin treatment in acne patientsLouis CK Ma HK Pract 2014;36:113-137 Summary Isotretinoin is an effective treatment for severe acne. It has been found to be ef f icacious across a dose range of 0.1-1mg/kg/day. Isotretinoin can also result in its long term remission. This ar ticle will review current literature on isotretinoin use and discuss factors that are associated with a possibility of recurrences. Keywords: stroke, cardiovascular risk factors, knowledge, perception and primary care. 摘要 異維生素A酸是嚴重痤瘡的一種有效治療藥物。每日跨 0.1-1mg/kg的劑量是其有效治療範圍。與其他抗痤瘡藥物不同, 異維生素A酸也可對病情造成長期緩解。本文將回顧現有文獻 對異維生素A酸的使用和探討對所有與復發相關的可能性較高的因素。 Introduction Isotretinoin (13-cis-retinoic acid) is a vitamin A derivative. Since its widespread use in the 1980s, it has been proven to be a very effective treatment for severe acne.1,2 It is the only medication that acts simultaneously against all four major aetiological factors of acne.1,2 It is comedolytic and anti-inflammatory. It also reduces sebum secretion and indirectly inhibits Propionibacterium acnes. Inflammatory lesions generally respond faster than non-inflammatory comedones. The British National Formulary (BNF) recommends 500 microgram/kg daily, increased if necessary to 1mg/kg, for 16-24 weeks. A total of 120-150 mg/kg of isotretinoin given over 6 months is stated to be the optimal cumulative dose for acne clearance. The current product licence indications are severe forms of acne (such as nodular or conglobate acne or acne at risk of permanent scarring) and acne resistant to adequate courses of standard therapy with systemic anti-bacterials and topical therapy. Prescribers need to be aware of the many potentially serious adverse effects associated with isotretinoin including teratogenicity, hyperlipidaemia, impaired liver function and possibly depression. Other sideeffects of isotretinoin include muco-cutaneous effects, musculoskeletal effects, gastrointestinal effects, ocular effects and haematologic effects.1,2 Because of its potentially serious complications, the prescription of isotretinoin is restricted in many parts of the world. In the United Kingdom, it's prescription is limited to dermatology consultant-led teams only. However, there is no such restriction in Hong Kong. Hence, it is important for doctors who will prescribe them to have a sound knowledge in the dosages of isotretinoin. A case presentation History SK, a 17-year-old student, presented to me with acne on his face and trunk since the age of fifteen years. Different skin cleansing agents from a local pharmacy were ineffective. He received advice from his general practitioner (GP) and used topical erythromycin gel twice daily. His acne worsened after one year's usage. His GP then put him on a six-month course of oral minocycline 100mg daily and changed his topical treatment to 2.5% benzoyl peroxide in the morning and 0.01% tretinoin gel at night-time. His acne improved but flared up again 2 months later. Another six-month of minocycline 100mg was prescribed, which was again ineffective. His acne worsened and there was scarring on his face and trunk. SK had enjoyed good past health. He was not on any drugs that could induce acne, including topical and oral steroids and some anticonvulsants. He lived with his elder sister and parents in a nearby residential estate. His elder sister also had mild acne, which was managed by 0.1% adapalene. Findings Examination of SK revealed numerous inflammatory papules, pustules and severe nodulocystic lesions on his face, chest and back. Comedones and seborrhoea were present. Significant scarring was noted over the chest. A diagnosis of rosacea was unlikely in the presence of comedones and truncal involvement. There were no discharging sinuses to suggest acne conglobata. Acne fulminans was unlikely in the absence of systemic upset and articular symptoms. SK was psychologically affected by his acne lesions but he did not have depressive symptoms. To be comprehensive, assessment of acne should include mood assessment as acne can be associated with depression. SK suffered from severe nodulocystic acne with truncal involvement and had failed to respond to systemic antibiotics. Isotretinoin was the best available treatment for him as it works better for inflammatory lesions than comedones. Pustules can be reduced by 50% after 2-4 weeks of therapy, although truncal lesions and nodules are more resistant to treatment. Considerable or complete resolution is expected after a course of therapy. Lesions may recur, though they are usually less severe. SK weighed 78kg. He was started on isotretinoin 40mg daily after his baseline liver function and fasting lipids results were noted to be unremarkable. He was asked to recheck his blood tests one month after starting therapy and 3 months thereafter. He was reviewed one month later. His facial lesions have slightly improved but his truncal lesions showed no noticeable improvement. The only adverse effect was mild cheilitis. His isotretinoin was increased to 70mg daily in view of his minimal response and limited side effects. One month later, his facial acne was much better while his truncal lesions started to improve. However, his cheilitis was worsened, accompanied by the development of skin dryness as well as eyes and nose irritation. These were treated with moisturisers. The same dose of isotretinoin was given for two more months, by which time his facial lesions had cleared up while only some papules remained on the trunk. Because truncal lesions were associated with higher relapse rates, the decision was made to reach a cumulative dose of 150mg/kg. After 2 more months of isotretinoin at 70mg/kg, all his acne lesions had cleared up. SK received a total dosage of (40mg x 30) + (70mg x 30 x 5) = 11,700mg or 150mg/kg, which was in keeping with the recommendations in the BNF. SK had a mild relapse about one year post-treatment, presenting with only facial comedones and inflammatory papules. There were no nodulocystic lesions and no truncal involvement. In view of the mild severity, topical 0.1% adapalene was prescribed to which there was good response. Discussion Results from studies on isotretinoin treatment have been mixed.3-7 Nevertheless, these studies suggest that a total isotretinoin dosage of at least 100-120mg/kg was effective to reduce relapses. A meta-analysis8 of 18 articles indicated that relapse was dose-dependent and a cumulative dose of 120mg/kg/day was required to obtain optimal results. On the other hand, Ng and Goh5 opined that cumulative dosage > 150mg/kg provided little therapeutic benefit as some therapy-resistant patients were destined to respond poorly. The same recommendation was made by Lehucher-Ceyrac D and co-workers.9 Current guidelines10,11 recommend isotretinoin at 0.5-1mg/kg/day for 16-24 weeks with a cumulative dosage of 120-150mg/kg. Isotretinoin may cause paradoxical flare-ups, especially of the inflammatory lesions, during the first few weeks of therapy.10-12 They are usually mild and subside spontaneously within 1 – 2 weeks. Severe flares necessitate isotretinoin dose reduction and a course of systemic steroids. The underlying mechanism remains elusive, although a sudden release of a large number of Propionibacterium acnes antigens is hypothesised to be the culprit.13 These antigens produce an intense local inflammatory reaction which is manifested as acute flare-ups. Clark and Cunliffe 13 investigated 980 acne patients treated with isotretinoin 0.5-1mg/kg/day. They reported flare-ups in 59 patients, usually within 3-5 weeks of therapy. However, severe flares occurred only in those taking 1mg/kg/day. In order to reduce flares, recent guidelines 10,11 recommended starting isotretinoin at a low dose (0.5mg/kg/day) for the first four weeks and increasing the dosage to 1mg/kg/day afterwards. Demircay and co-workers 14 used an initial isotretinoin dose of 0.5mg/kg/day and noticed flares in 32% of their patients after a median time of 4 weeks' therapy. Most of them had mild flares that resolved spontaneously. 10% had moderate flares, necessitating a dose reduction. Severe flares that required systemic steroids were rare (4.5%). Males, severe acne, multiple facial comedones, and truncal nodules were significant predictors of severe flares. They opined that patients with these risk factors warrant a starting dose below 0.5mg/kg/day, which was in keeping with the guideline by an acne expert working group.11 Borghi et al 15 compared 132 patients who were treated with a lower starting dose of < 0.2mg/kg/day with a control group of 142 patients who received the standard dose of 0.5mg/ kg/day initially. They reported that 7.5% of patients on a lower starting dose flared, while 15.5% of those on the standard 0.5mg/kg/day did so during the first 4 weeks (p=0.0415). They suggested that a lower starting dose (< 0.5mg/kg/day) for selected acne patients might further reduce the possibility of flares than the standard regime. The study was, however, limited by possible surveillance bias as investigators were not blinded. The initial dosage may also be limited by the patient's tolerance of side effects. Most of these side effects are dose-related and are quite common.16-18 The majority of patients suffer from muco-cutaneous effects (cheilitis, xerosis, skin peeling, hair loss, photosensitivity; dryness of eyes , nasal and genitourinary mucous membranes). Cheilitis was reported in 91.3% patients treated with isotretinoin.17 The other common adverse effects were dry skin (90%), nasal dryness and epistaxis (30-40%) and eye irritation (28%).17 McLane 17 summarised the findings of two safety trials of isotretinoin. Cheilitis occurred within two weeks of therapy and lasted throughout the treatment period. The occurrence of dry skin and facial rash peaked at four weeks while dry eyes and nose were most common in the second month of therapy. Unlike cheilitis, these side effects tended to lessen gradually with therapy. Side effects also involve the musculoskeletal system (myalgia and arthralgia), nervous system (headaches and possibly depression) and gastrointestinal system (vomiting). Laboratory side effects (impaired liver function and hyperlipidaemia) have been reported. If the patient is unable to tolerate these side effects, the dosage should be adjusted accordingly.
Louis CK Ma, MBChB, MRCP (UK), DPD (Cardiff)
Master Student MScPD (Cardiff), Department of Dermatology, Cardiff University, United Kingdom. Correspondence to : Dr. Louis CK Ma, louishkp@gmail.com
References
|
|