|
September 2014, Volume 36, No. 3
|
Original Article
|
The usefulness of primary care physicianled motivational interview in a substance abuse check-up clinic: a retrospective studyTsz-yan Lo 盧芷欣, Carlos king-ho Wong 黃競浩, Po-shan Lau 劉寶珊, Chi-hang Lau 劉知行, Winnie Wan-yee Chan 陳韻宜, Tak-cheung Wong 黃德祥 HK Pract 2014;36:83-98 Summary
Objective: To assess the outcome of a structured health check-up
clinic for substance abusers.
Keywords: Substance-related disorders, motivational interviewing, primary health care 摘要
目的: 對一家為藥物濫用者而設之結構化體檢診所結果進行評估。
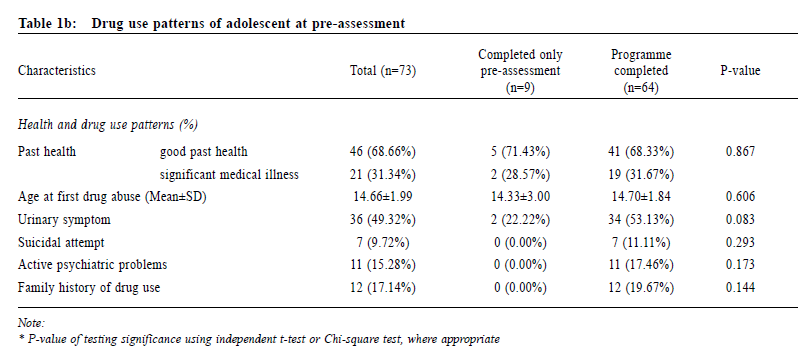
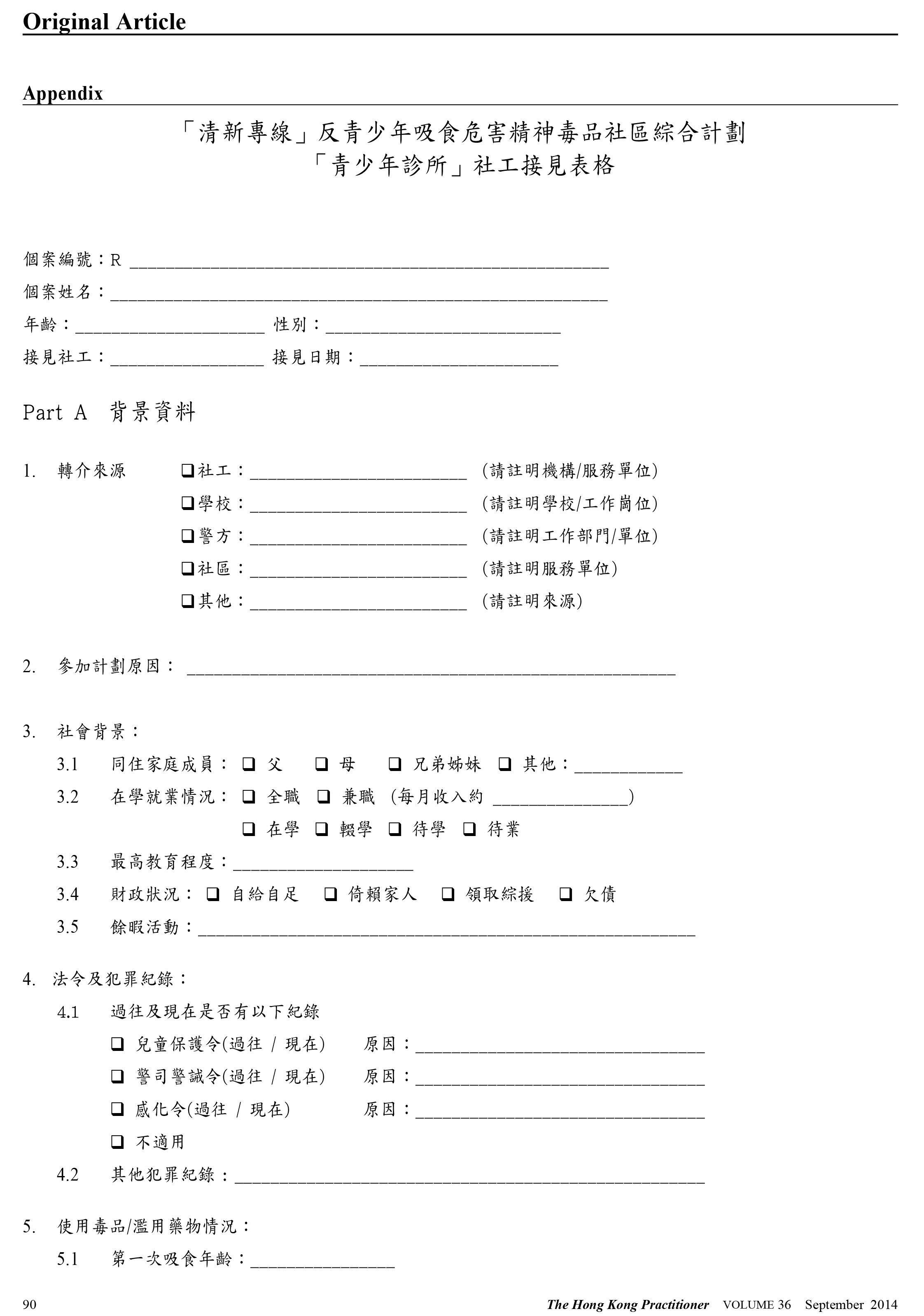
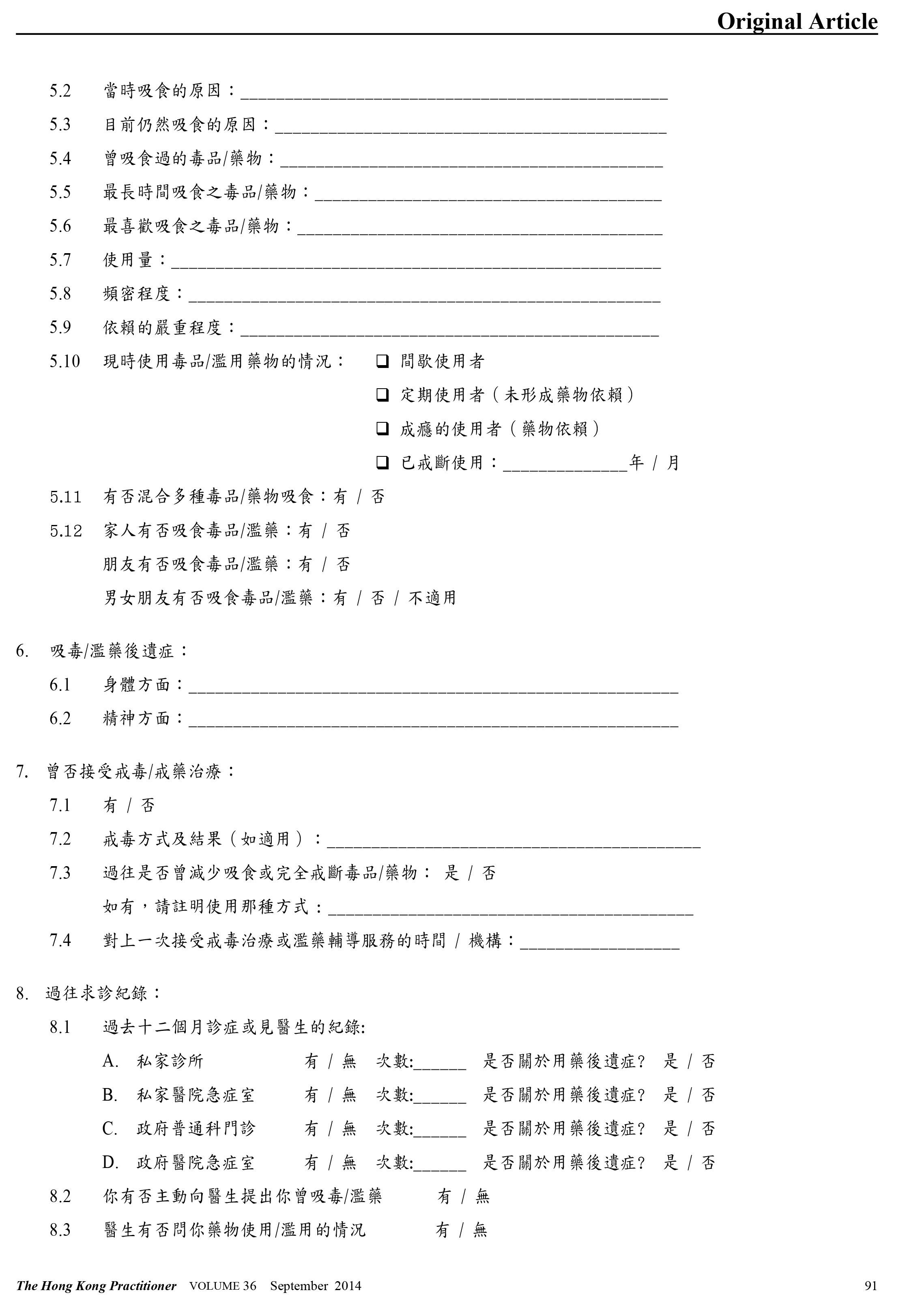
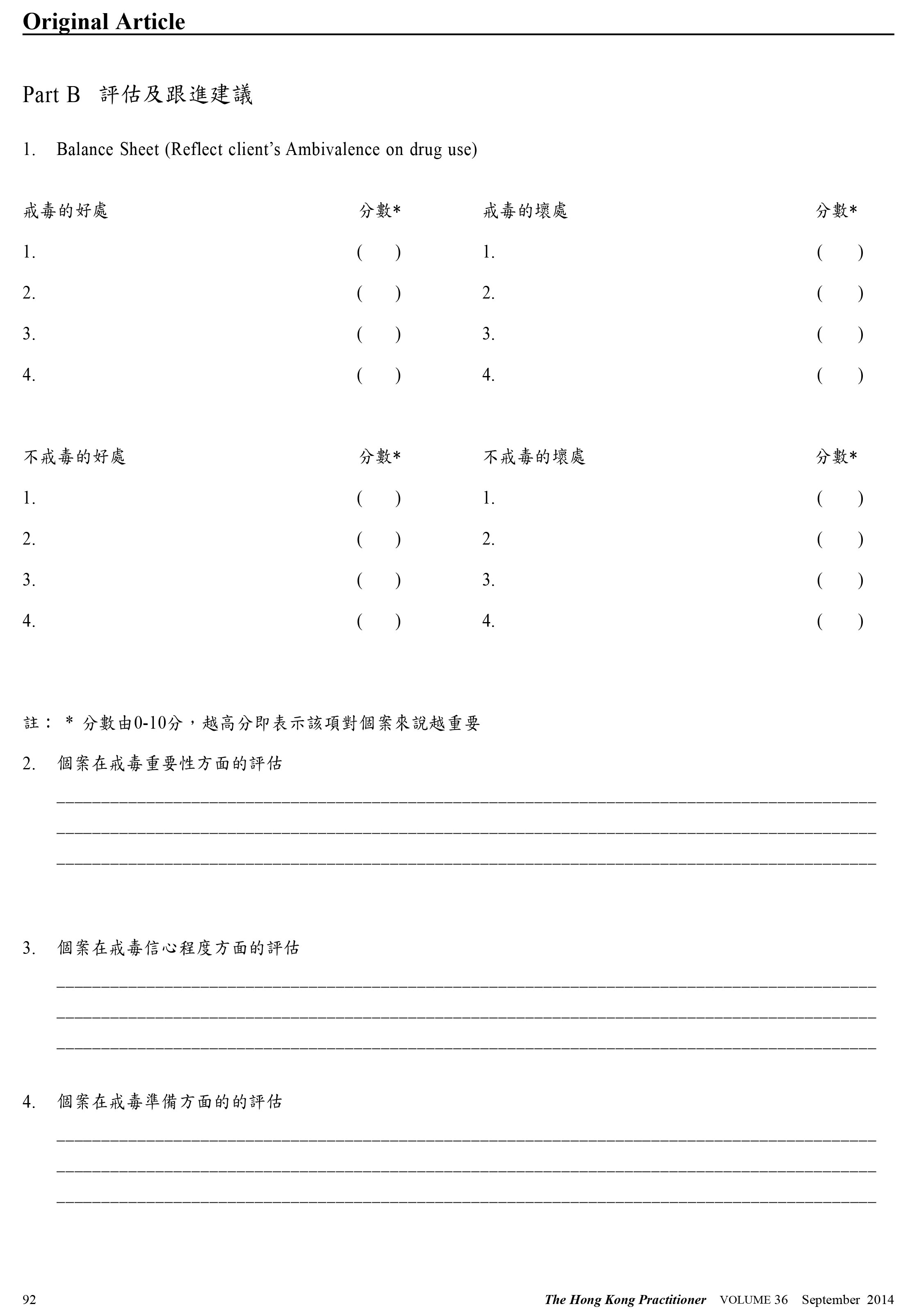
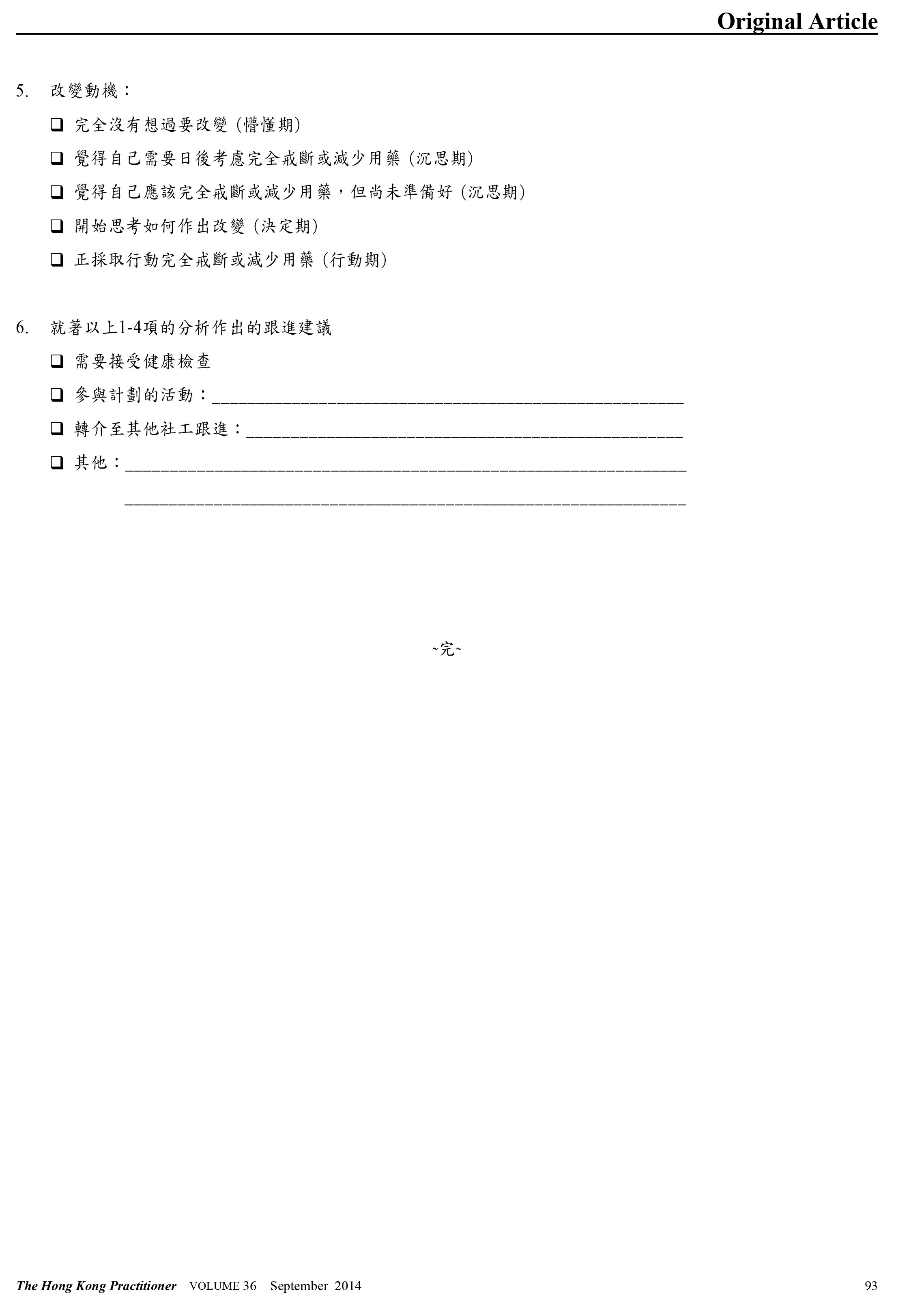
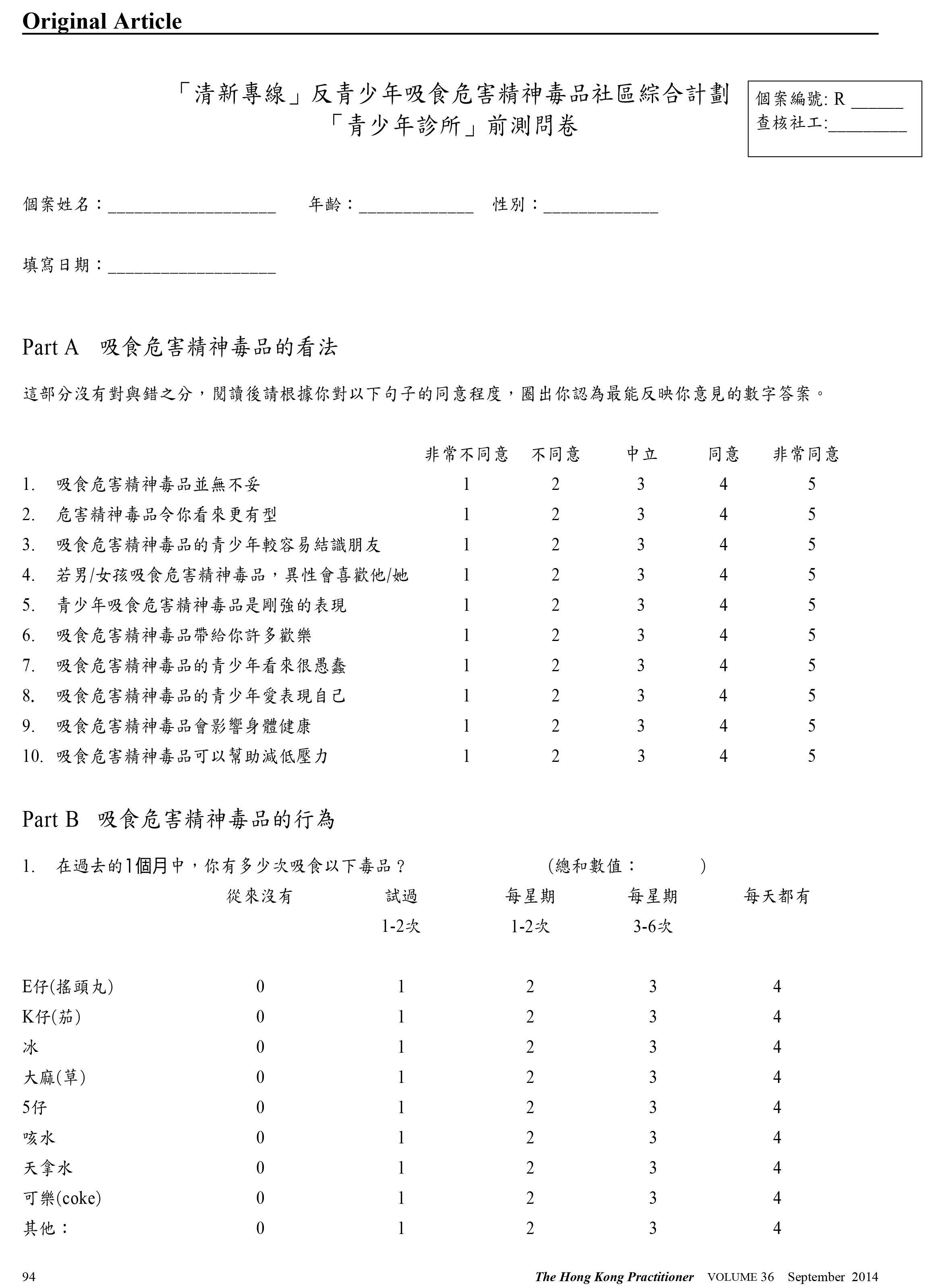
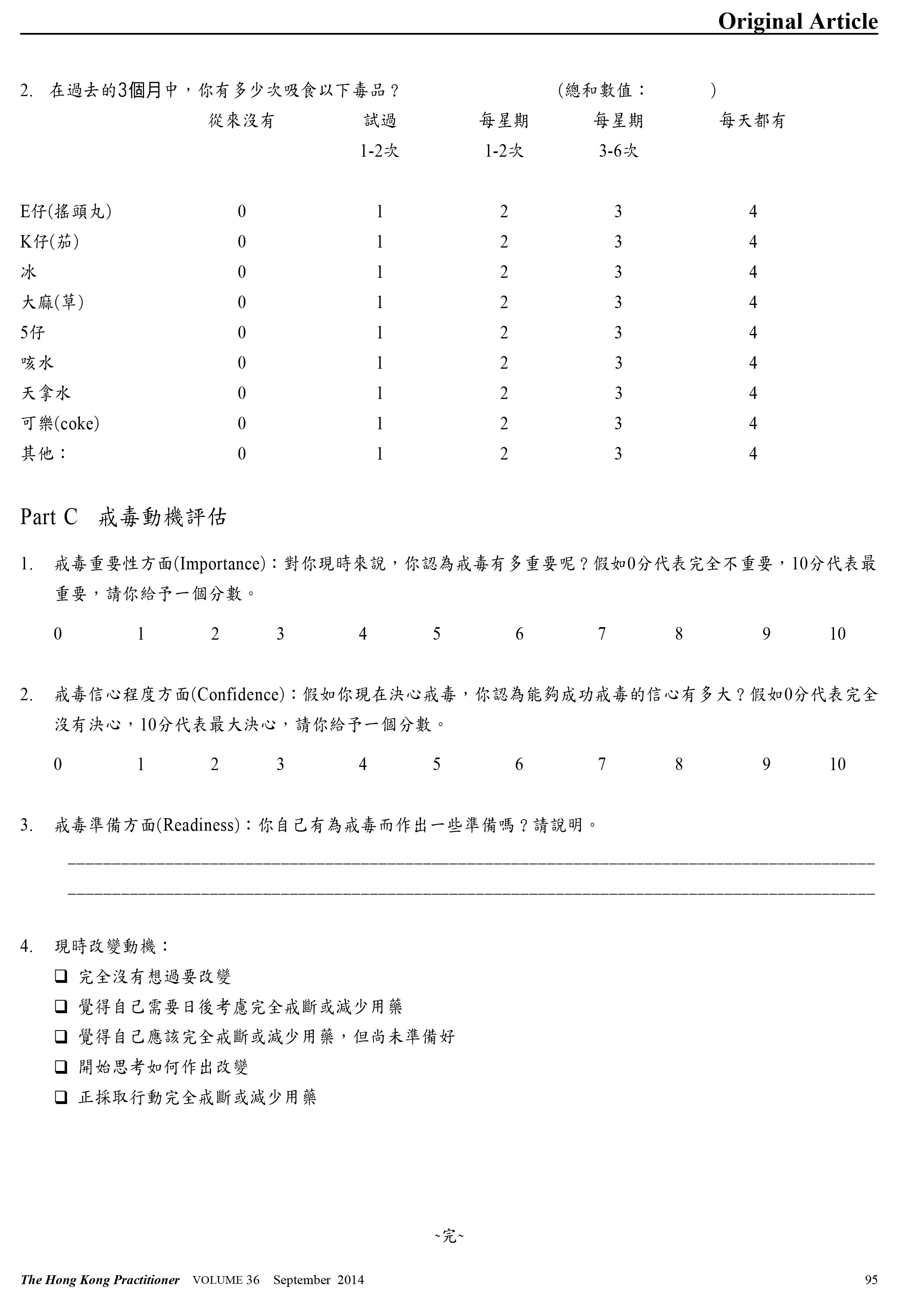
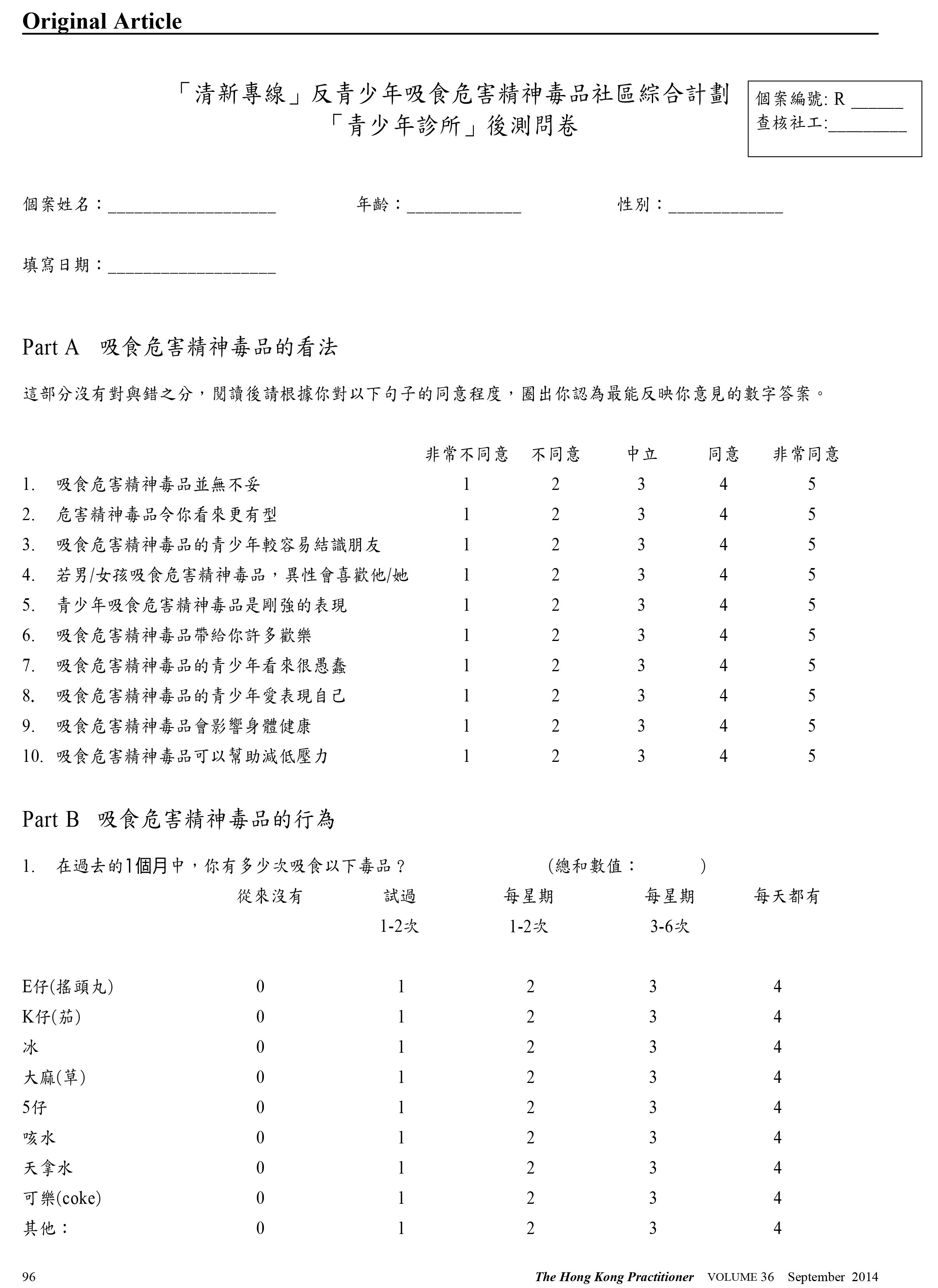
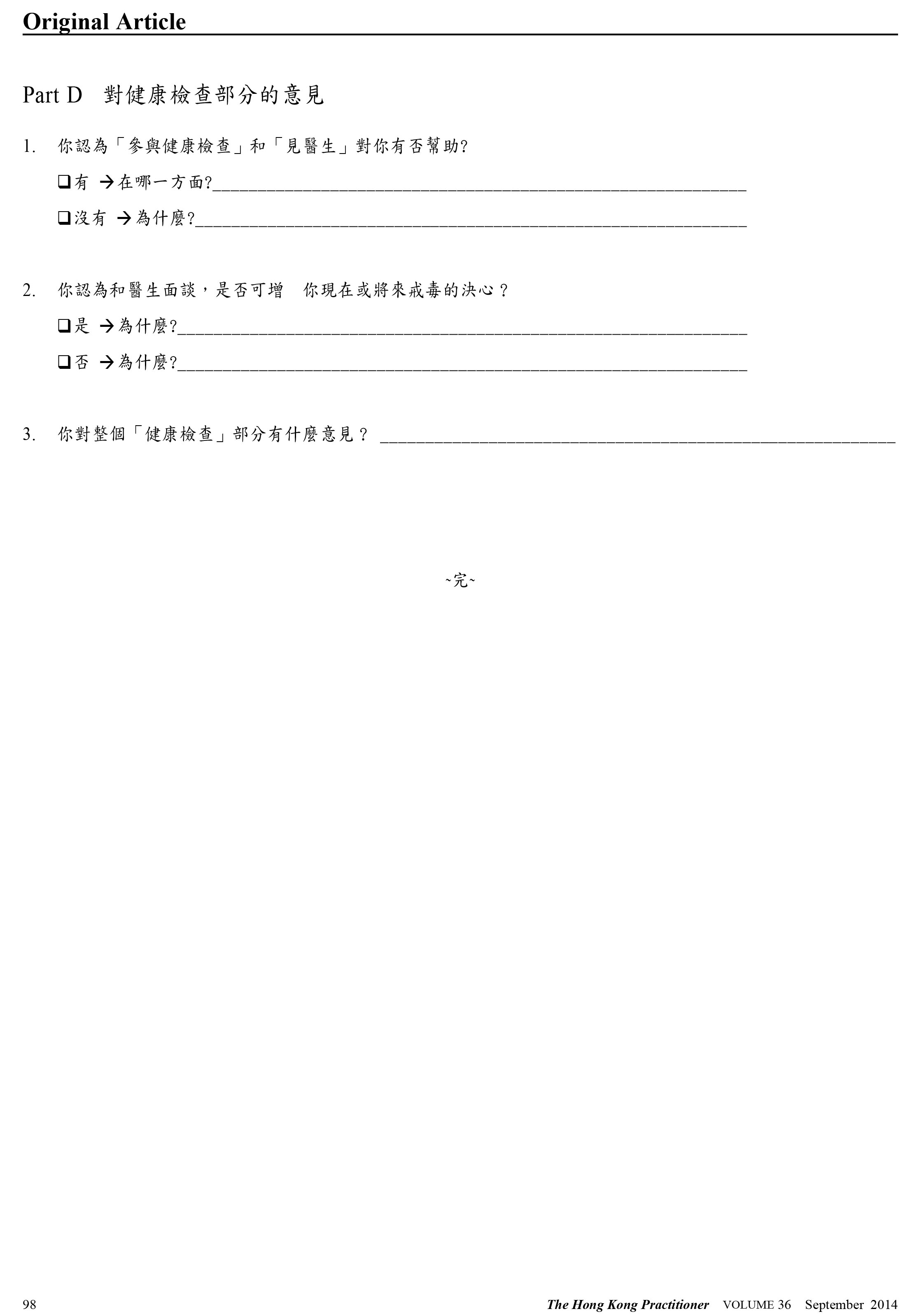
主要詞彙: 藥物相關性障礙,動機性訪談,基層保健。 Introduction Substance abuse among young people is a significant problem worldwide. In 2010, 230 million people or 1 in 20 adults were estimated to have used an illicit drug at least once.1 The evolution of a drug problem has been influenced by demographic trends, socioeconomic and sociocultural factors such as value systems, religion and youth culture. According to the Hong Kong Central Drug Registry of Drug Abuse,2 there were 10,939 reported number of drug abusers in 2012. 14.5% were aged less than 21 years old. 96.6% of these young drug users reported using psychotropic substances, and 49.9% were previously convicted. The total cost of treatment , rehabilitation, counselling, preventive education, and research related to substance abuse in 2010 was $301.42 million dollars.3 Unfortunately, there is currently insufficient training, no organisation, or reimbursement to screen, assess, and refer those with drug dependence or abuse disorders to appropriate services.4 Multi-discipline partnership, adopting multi-systemic therapy approach, is a viable option for substance abuse treatment programme.5 In addition, primary care physicians have a role in routine drug use screening during our consultation,6,7 screening for physical and psychological co-morbidities and complications, providing brief motivational interviewing for their drug abuse behaviour, and co-ordinating referrals to appropriate parties.8,9 Motivational interviewing is useful in the treatment of a broad range of behavioural problems and diseases,10,11 which is defined as "a client-centred, directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence".12 Evidence suggests that motivational interviewing is useful for substance abuse treatment,13,14,15 able to reduce drug use by teenagers 16,17 and can be performed by primary care physicians.18 Motivational interviewings (MI) are already employed by psychologists 19 and psychiatrists 20 in some of Hong Kong's substance abuse treatment programmes. However, data on the efficacy of MI employed by primary care physicians, especially in our locality, is lacking. The substance abuse check-up clinic in Our Lady of Maryknoll Hospital was established in September 2009. It is run by primary care physicians who provide health check-up, group activities and motivational interviewing to young subjects and is part of a project supported by Beat Drug Fund of the Hong Kong Government. This paper describes the impact of this primary care-led MI-based substance abuse check-up programme. There are 8 primary care physicians in the team; the team leader is experienced in motivational interviewing and he is responsible for training of the team members, designing guideline for motivational interviewing. All team members are given 3 hours of training including materials for motivational interviewing, based on Miller and Rollnick's motivational interviewing theories.12 Briefing sessions and peer sit-in sessions are held before the start of seeing subjects. The pre- and post- intervention questionnaires on drug use are adopted from evaluation questionnaire of Project Astro Mind.21 Permission was granted by Prof Daniel Shek of Hong Kong Polytechnic University to use the questionnaires of the programme. The Hong Kong Playground Association, which is a non-government organisation, recruits young drug users in the community. The drug users should be Hong Kong citizens and are suitable to manage in primary care setting. Their social workers interview the subjects individually at baseline, to gather background and drug use information in a confidential way. During the interview, the social workers fill in the intake forms and pre-intervention questionnaires accordingly (see Appendix). After an interview by social workers, subjects are arranged into group activities including an educational talk by social workers and doctors, and group sharings with ex-drug users. An individual health check-up session in Our Lady of Maryknoll Hospital is then implemented, which includes body weight, height, memory test, urinalysis, complete blood count, liver and renal function tests. After all tests results are available, subjects are arranged a 45-60 minutes of medical consultation with motivational interviewing by a family physician. During the consultation, the doctors explain check-up results, screen for physical and psychological co-morbidities and complications, and perform a motivational interview. The motivational interview consists of 2 phases: building up motivation for change followed by strengthening commitment for change. Follow-up visits by family physicians for other health problems, referral to psychiatrists, paediatricians, or other specialty doctors are arranged if needed. All subjects are followed up by social workers after consultation for at least 3 months, followed by a post-intervention questionnaire, describing their drug use pattern from 3 months to 1 year after the motivational interview, and also their opinions about the service. Methodology Study Design This was a retrospective study on attendees of a substance abuse check-up clinic. Inclusion criteria All subjects aged 13-40 years who attended the check-up clinic between 9/2009 and 1/2013; and who had self-reported any history of substance abuse. Exclusion criteria Those who only abuse alcohol and/or tobacco were excluded. This was consistent with definition of substance abuse by the Hong Kong Government.22 Data collection Drug-use information was gathered by self-report, as self-report of drug users had been found to be reliable in previous studies.23,24 The intake forms, pre- and post- intervention questionnaires and medical records of the subjects were reviewed by the attending doctors. Information gathered included socio-demographic data: age, gender, referral source, living status, drinking status, smoking status, occupation, education level, financial status, and criminal record; information on health; drug-use pattern including age at first drug abuse and type of drugs used ever at baseline. For change in drug-use in the past 1 and 3 months before and after motivational interviewing, we reviewed number of drugs used, total drug score based on frequency and abstinence. There was also a section on patient's subjective feeling about usefulness of the programme. Outcome measures Change in abstinence rate, frequency and number of drugs used Our main outcome measures were to compare (1) abstinence rate, (2) total drug score reflecting drug-use frequency, and (3) number of drugs used during past 1 and 3 months, at baseline and after motivational interview. Statistical analysis All statistical analyses were conducted using SPSS version 20 for Windows. Descriptive statistics of defaulters and non-defaulters were compared using Chi-square and independent t-test, where appropriate. Changes in continuous variables including number of drugs used and total drugscore between pre- and post-intervention were compared by paired t-test. Binary categorical variables including 1 and 3 months abstinence were analysed by McNemar test. This study was approved by the Hong Kong Hospital Authority, Kowloon West Cluster Clinical Research Ethics Committee. Results Demographic characteristics A total of 73 subjects were seen (42.5% males) and 64(87.7%) completed the programme; none of the subjects was excluded. For the 64 non-defaulters, 14 subjects completed at 6-12 months and 1 completed at 38 months when called back, and 9 defaulters were not reachable, despite efforts to call by our social workers. Their demographic data are shown in Table 1. When we compared demographic characteristics of defaulters with non-defaulters, we found no significant differences between 2 groups.
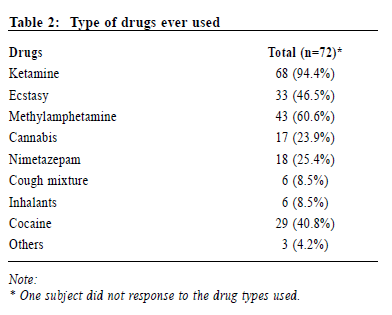
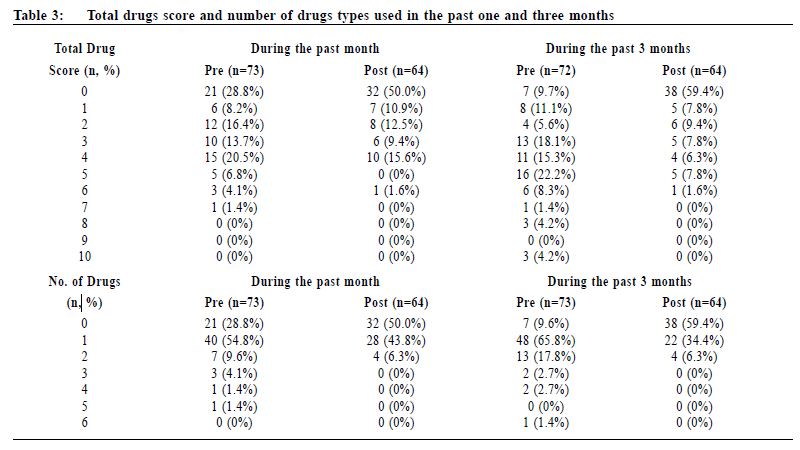
Drug pattern The mean age of first drug-use was 14.7 years old (Table 1). The most commonly used drug was ketamine (94.4%), followed by methylamphetamine (60.6%) and ecstasy (46.5%) (Table 2). 16.4% of our subjects used more than 1 type of drugs in the past 1 month; 24.7 % used more than 1 type of drugs in the past 3 months (Table 3).
Co-morbidities 7 (9.7%) were found to have history of suicidal attempt(s), 6 (8.3%) had depression, 1 (1.4%) had attention-deficit-hyperactivity disorder and 1 (1.4%) had conduct disorder. 57 (78.1%) were found to have physical symptoms. 36 (49.3%) of all drug users had urinary symptoms, while 60% (27 out of 45) of ketamine users had urinary symptoms (Table 1). Change in drug-use after programme completion The total drug score (p<0.001) and number of drugs used (p<0.001) reduced significantly at both 1 month and 3 months after programme completion. The abstinence rate (9.6% vs 59.4 %; p< 0.001) was significantly higher in 3 months after programme completion compared to baseline (Table 4).
Programme evaluation 93.2% found the service helpful in changing their drug use behaviour and 86.2% found motivational interview could increase their confidence of abstinence. Discussion This study focused on the change in drug-use pattern after a motivational interviewing-based programme. The population reviewed in this study was younger and had more female drug users. The higher prevalence of ketamine abuse was likely related to our younger population. Otherwise the population was similar to previous local studies.2 It seems that the programme helped subjects to decrease and quit drugs. Subjects in our programme decreased their drug-use at 1 and 3 months after programme completion. A similar study revealed that the percentage of regular drugs users decreased from 44% to 13% at 6 weeks, then increased to 18% at 6 months.20 This is likely due to the fact that both studies have similar population and intervention. The finding is also consistent with previous systematic review 14 in that motivational interviewing reduces substance-use during short follow-up. The long-term effects are however unknown as we did not have long term follow-up in the programme. There is another local treatment programme organised by paediatricians, which consisted of interview, cognitive and motor function testing, followed by debriefing and counselling. 51.9% of their subjects could abstain for at least 3 months;25 it is only slightly lower than 59.4% in our programme. Though that study was not targeted for abstinence rate, it was possible that other non-MI based treatment programmes were also effective for young drug users. Limitations There are some limitations in this study. Firstly, our sample size was very small despite our much efforts, which restricted analysis of associations between abstinence rate and demographic factors, including smoking. Secondly, we relied on subjects' self-report about their drug-use; there were no objective measures to verify their drug-taking; some subjects had post-intervention assessment more than 6 months after programme completion, due to various reasons like defaults and being in hostels. These results could be inaccurate and prone to recall bias. Lastly, there was no control available in the study so the effect of the programme may be over-estimated, because some reduction of drug-use may be attributed to natural time course only. Despite these limitations, this study provides preliminary local evidence that a structured programme involving motivational interviewing by primary care physicians is effective and feasible for the care of these young drug users. Extension of similar service with expansion to other districts can be considered in view of the positive impact. Future service improvement may include motivational interviewing for smoking cessation,26,27 as there is high proportion of smokers in this programme. On the other hand, smoking cessation may actually enhance outcome success as well.28 Future randomised control study in this aspect with longer follow-up duration may help to further verify efficacy and effectiveness of substance abuse management by primary care physicians. More research is also needed to understand the mechanisms of change, the impact of motivational interventions on adolescent developmental transitions and to understand how to disseminate these interventions effectively to those adolescents who need them most.29
Conclusion A local structured programme with motivational interviewing is effective for abstinence and reduction in drug-use in primary care setting. Small sample size is the key limiting factor in local drug abuse research. Acknowledgements We thank the Beat Drug Fund of the Government of Hong Kong SAR for funding the Youth Substance Abuse Check-up Clinic; the Hong Kong Playground Association, which helped to recruit subjects, complete questionnaires, implement group activities and co-ordinate the programme; Dr Fu Sau Nga and Dr Sydney Cheung who advised on research project; Dr Lam Tak Man, Dr Tam Ho Shan, Dr Cheung Wing Wo, Dr Lau Wing See and Dr Ching Tak Kwan who contributed to Youth Substance Abuse Check-up Clinic data collection and entry.
Tsz-yan Lo, MBBS (HKU), FHKAM (Family Medicine)
Resident Specialist Department of Family Medicine and Primary Health Care, Kowloon West Cluster, Hospital Authority, Hong Kong SAR, China. Carlos king-ho Wong, BSc(HKUST), MPhil(HKUST), PhD(HKU) Research Assistant Professor Department of Family Medicine and Primary Care, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China. Po-shan Lau, MB ChB (CUHK), FHKAM (Family Medicine) Associate Consultant Department of Family Medicine and Primary Health Care, Kowloon West Cluster, Hospital Authority, Hong Kong SAR, China. Chi-hang Lau, FHKAM (Family Medicine) Associate Consultant Department of Family Medicine and Primary Health Care, Kowloon West Cluster, Hospital Authority, Hong Kong SAR, China. Winnie Wan-yee Chan, MBBS(SYD), FHKAM (Family Medicine) Family Medicine Coordinator Department of Family Medicine, Our Lady of Maryknoll Hospital, Kowloon West Cluster, Hospital Authority, Hong Kong SAR, China. Tak-cheung Wong, MBBS (HK), FHKAM(Medicine) Hospital Chief Executive Our Lady of Maryknoll Hospital, Kowloon West Cluster, Hospital Authority, Hong Kong SAR, China. Correspondence to : Dr Tsz-yan Lo, Department of Family Medicine and Primary Health Care, 1/F, OPD Block, Our Lady of Maryknoll Hospital, 118 Shatin Pass Road, Kowloon, Hong Kong. SAR, China.
References
|
|