
|
March 2018, Volume 40, No. 1
|
Case Report
|
Multiple Myeloma presented with a pathological fracture of the clavicle: a case reportDerek GC Ying 邢格政, Siu-hin Ko 高嘯軒, Catherine XR Chen 陳曉瑞, King-hong Chan 陳景康 HK Pract 2017;40:37-39 SummaryMultiple myelomas(MM) are cancer of the plasma cells, characterised by neoplastic proliferation of a single monoclonal immunoglobulin. The initial presentation can range from completely asymptomatic to more severe systemic involvement. Here we report a case of a middle-aged female patient who presented initially to the primary care with bilateral shoulder discomfort. Plain radiographs demonstrated a displaced fracture of the left clavicle. Further evaluations and series of investigations for this pathological fracture revealed that she was suffering from multiple myeloma. Keywords:Multiple Myeloma, Pathological Fracture, Primary Care 摘要多發性骨髓瘤(MM)是漿細胞的癌症,其特徵在於單 個單克隆免疫球蛋白的腫瘤增生。最初的表現可以從完全 無症狀到更嚴重的系統性波及。在這裡,我們報告了一個 中年女性病人,最初來門診時是因為雙邊肩部不適。平片 顯示左鎖骨移位性骨折。對這種病理性骨折的進一步評估 和系統性檢查顯示出,她患有多發性骨髓瘤。 關鍵詞:多發性骨髓瘤,病理性骨折,基層醫療 IntroductionMultiple Myeloma(MM) is a debilitating malignancy of the plasma cells. It is relatively uncommon, accounting for only 1.8% of all cancer cases. The median age of patients diagnosed with MM is 68 years for men and 70 years for women.1 Malignant proliferation of the plasma cells results in haematologic abnormalities, such as anaemia, leukopaenia and thrombocytopaenia. Presenting symptoms may be nonspecific, ranging from common complaints such as weakness, malaise, anaemia, and infections, to bleeding tendency. Bone pain is also common with MM, caused by both bone marrow infiltration with aberrant monoclonal immunoglobulin production and the direct effect of the growing tumour mass. With more extensive bone involvement, pathologic fractures often ensue, with axial bones being the most common fracture sites.2 We re-examine the diagnostic process of a case of MM presented to the general out-patient department with bilateral shoulder discomfort. The CaseA 64-year-old lady, who has enjoyed relative good past health and was a part-time salesperson by occupation, first presented to a General Out-Patient Clinic (GOPC) in Hong Kong complaining of dull discomfort over her shoulders and clavicles for 1 month. During this period she also noted a swelling over her left clavicle. She had no history of trauma, injury or muscle sprain, and denied constitutional symptoms such as fever, weight loss or lethargy. On physical examination, her vital signs and body mass index were normal. General condition was satisfactory. Musculoskeletal examination showed tenderness over both clavicles and a bony prominence over the medial one-third of the left clavicle. Bilateral shoulders examination was otherwise unremarkable. Plain radiographs of the clavicles showed a fracture at the medial one-third of left clavicle, with superior displacement of medial fragment (Figure 1). She was invited for a second clinic visit to review her condition and the radiographs. The pain in her clavicles was persistent. She reiterated that she had not suffered any injury to her upper limbs or torso. Review of systems revealed that she was menopausal at around the age of 48. She was clinically euthyroid, and had no unusual chest, breast, or gastrointestinal symptoms. She had no history of chronic corticosteroid use. As osteoporosis was a diagnostic possibility, bone densitometry scan was initially suggested for the patient. However, blood investigation demonstrated a normocytic normochromic anaemia (haemoglobin level 10.3 g/dL), with other blood cell lineage counts within normal range. Biochemical profile revealed a reversed Albumin/Globulin (A/G) ratio (Total protein 108 g/L, Albumin 31 g/L, Globulin 77 g/L). Erythrocyte sedimentation rate (ESR) was significantly elevated at 140mm/hr. Other biochemical investigations, including renal function tests, calcium and phosphate levels, thyroid function tests, were unremarkable. Hepatitis serology was negative. In view of the above abnormalities, the patient was referred for hospital admission for suspected multiple myeloma. Serum electrophoresis was carried out and revealed increased free kappa and lambda light chains. Urine for Bence-Jones protein showed increased A kappa and Fr kappa light chains. Skeletal surveys revealed multiple osteolytic lesions in the skull, as well as multiple collapsed fracture of the lumbar vertebrae. Bone marrow biopsy revealed malignant plasma cells, confirming the diagnosis of multiple myeloma. 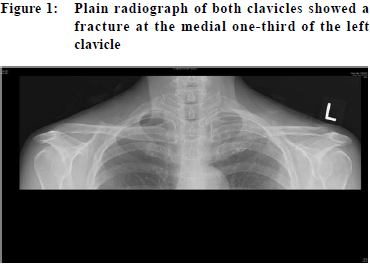
In-hospital care was under the haematology, oncology and orthopaedic teams. Her clavicle fracture was treated conservatively. Her MM was treated with pamidronate and thalidomide, and the disease started responding with improvement in her serum light chains and laboratory abnormalities. DiscussionPathological fractures are fractures from weakened bone due to underlying systemic diseases. The weakened bone predisposes patients to fractures without adequate trauma. Once a pathologic fracture is suspected, its underlying cause must be sought. Osteoporosis, in particular, is by far the most common cause that leads to non-traumatic fracture. Osteoporotic fractures commonly occur in three typical sites: compression fracture of the vertebrae, neck of femur fracture, and Colles fracture at the wrist. When pathological fractures occur in sites other than these, clinicians should be vigilant to look for other possible underlying pathologies, especially neoplasms or endocrinopathies. Thorough history is mandatory, including the degree of trauma and the mechanism of injury, as well as any prodromal pain in the fracture region. Previous history of cancer or irradiation, and constitutional symptoms should raise particular concerns. Physical examination should include but not be limited to a detailed neurological examination, as well as assessing the neurovascular status of the fracture site. Baseline haematological and biochemical tests form an integral part of the initial evaluation. Complete blood count, renal and liver function tests, calcium and phosphate levels, inflammatory markers (ESR/CRP), Lactate Dehydrogenase (LDH), and skeletal survey looking for lytic or blastic lesions may offer pointers to delineate the cause of fracture. Depending on the clinical clues, further endocrine and biochemical tests such as thyroid function tests, parathyroid hormone, serum and urine protein electrophoresis for Bence-Jones Protein, Immunoglobulin levels may be warranted for diagnosis.3 
Patients with MM may present to the general practitioners with non-specific complaints, posting a diagnostic challenge in the general outpatient setting. Timely diagnosis of MM is of utmost importance, as a delay in diagnosis is associated with negative outcomes of the disease.4 According to a retrospective analysis, the most common signs and symptoms MM patients may experience were, in the order of their frequencies, anaemia (73%), bone pain (58%), deranged renal functions (48%), hypercalcaemia (28%) and weight loss (24%).5 Anaemia is usually normocytic and normochromic, related to bone marrow infiltration and renal involvement. Bony pain and subsequent fractures in MM are most common in the thoracic and lumbar vertebral bodies.6 Upper limb lesions and pathological fractures such as the one seen in the presented case are relatively rare in MM. Serum creatinine concentration may be raised in MM, as a result of hypercalcaemia, amyloidosis and light chain cast nephropathy. Usual office urine dipstick test may not be helpful in diagnosing MM, as it detects albumin but not the urinary monoclonal protein.2 Musculoskeletal complaints are common yet challenging problems encountered in primary care. This case represents a diagnostic challenge in the general out-patient setting as this patient with MM initially presented only of vague shoulder discomfort. It highlights the importance that when encountering a diagnostic uncertainty, the family physician should not only focus on the “most likely” diagnosis (i.e. Osteoporosis for this case), but also remain cautious on the “important yet not to be missed” possibilities. When tackling a pathological fracture, a sound diagnostic algorithm is called for to reach an aetiological diagnosis.
Derek GC Ying,LMCHK, FHKCFP, FRACGP
Correspondence to: Dr Derek GC Ying, Room 807, Block S, Queen Elizabeth
Hospital, 30 Gascoigne Road, Kowloon, Hong Kong SAR.
E-mail: ygc800@ha.org.hk
References:
|
|