
|
June 2019, Volume 41, No. 2
|
Update Article
|
An overview and approach to shoulder painStephen C Y Chung 鍾礎逸 HK Pract 2019;41:50-56 Summary
1. The single most important test at the shoulder
is the point of maximal tenderness. This allows
shoulder pathology to be localised for specific
physical examination to be performed. 摘要
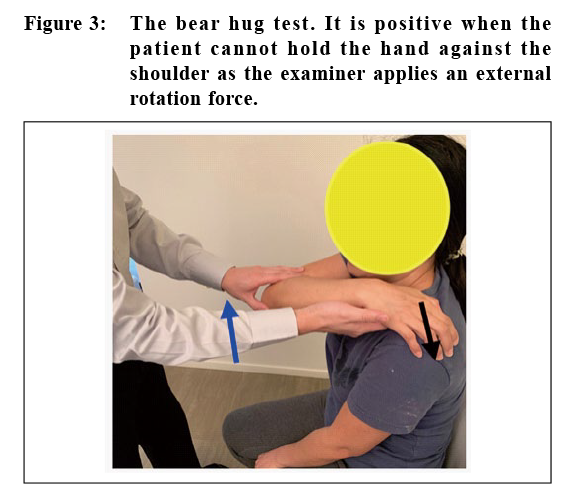
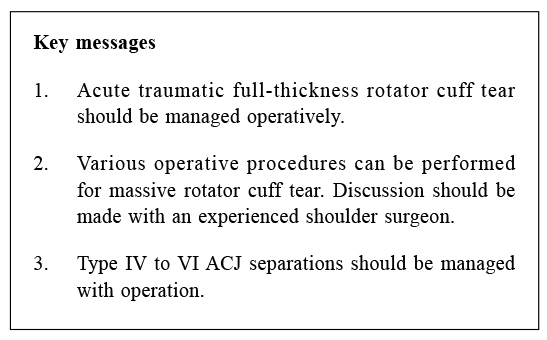
1. 肩膊檢查最重要的測試是找出肩膊的最痛點。這方法容許肩膊疾病得到針對性的檢查。 IntroductionShoulder joint is a complex region consisting of four joints (glenohumeral joint, acromioclavicular joint (ACJ), sternoclavicular joint and scapulothoracic joint) as well as encapsulating ligaments and rotator cuff muscles (supraspinatus, infraspinatus, subscapularis and teres minor). It is the most mobile joint of the body and yet despite its complexity it has stability and strength. History taking and examinationsA comprehensive history and physical examination for a patient who presents with shoulder pain is essential to make the correct diagnosis from an extensive list of differential diagnoses. For shoulder pain, the onset, the duration, the character, the location, any exacerbating and relieving factors should be carefully asked. Localised pain at supraspinatus tendon insertion together with night pain is suggestive of rotator cuff tear. Pain that occurs during overhead activities and internal rotation motion of the shoulder joint is suggestive of shoulder impingement pain. One needs to rule out cervical spine or brachial plexus pathology when pain and its associated numbness radiate distally to the elbow joint. The presence of constitutional symptoms such as fever, weight loss or migratory resting pain should alert clinicians to infections and neoplastic diseases. When shoulder pain occurs immediately after trauma, traumatic rotator cuff tear, acromioclavicular joint injury and fracture or dislocation of the shoulder joint are common differential diagnoses. Other symptoms associated with shoulder pain include stiffness, weakness and instability. Functional limitations of dressing, performing overhead activities, combing or washing hair, toileting and hygiene should be addressed. Recreational and occupational limitations should also be documented. For physical examination, both shoulders should be examined from the front, side and back. A proper and complete examination of both shoulders is essential. There are many specific physical examinations around the shoulder region but the single most important test is asking the patient to point to the most painful site with one finger. This often helps the clinician to localise the site of pathology and allow specific physical examination to be performed. When the shoulder pain is diffused and cannot be localised, the clinician should examine the cervical spine carefully to rule out referred pain. ManagementsShoulder impingement syndromeImpingement shoulder pain typically radiates down the superolateral aspect of shoulder. This mechanical pain occurs at overhead activities and internal rotation of shoulder. The symptoms can be reproduced during a positive Hawkins impingement sign (pain with passive internal rotation of the arm with shoulder in 90 degrees forward flexion) and Neer impingement sign (pain with forced passive forward elevation with arm at internal rotated position). (Figure 1) Shoulder pain is generated when the undersurface of the acromion irritates the bursal side of the rotator cuff tendons. Supraspinatus outlet view of shoulder plain radiograph can detect curve-shaped (type 2) or hook-shaped (type 3) acromion which has a higher chance of mechanical impingement on the rotator cuff. Ultrasound study allows dynamic visualisation of the acromial spur impinging onto the bursal side of the supraspinatus tendon. The impingement test with lignocaine (1%,10cc) injected into the subacromial space is a simple bedside procedure for making the diagnosis of shoulder impingement syndrome. The test is positive when there is diminution of pain with Hawkins and Neer impingement manoeuvres. Subacromial injection of local steroid and lignocaine has three objectives in the management of shoulder impingement syndrome. Firstly, this is diagnostic with a positive impingement test. Secondly, it is a therapeutic procedure. Thirdly, it has prognostic value when shoulder impingement pain subsided for a period but recurred after a couple of weeks or months. These patients are good candidates for operative intervention with shoulder arthroscopic surgery for long term relief of pain. Repeated subacromial injections of steroid of more than 3 times is best avoided to prevent excessive scarring in the subacromial space or weakening of rotator cuff tendons. Non-steroidal anti-inflammatory drugs (NSAID) and physiotherapy with scapular stretching and strengthening exercise can help to alleviate shoulder impingement pain. Patients who suffer from shoulder impingement syndrome and have failed conservative treatment for more than three months can be offered operative treatment with arthroscopic subacromial decompression. This minimally invasive procedure removed inflamed bursal tissue and bone spurs underneath the acromion. The coracoacromial ligament is also released from the anterolateral acromion edge to increase the subacromial space to prevent further impingement.1,2 Partial thickness rotator cuff tearPartial thickness rotator cuff tear can be asymptomatic or presented as shoulder pain at night and overhead activities. Most patients have a painful arc of motion between 60 to 120 degrees of abduction. The impingement signs are almost always positive in patients with symptomatic partial thickness rotator cuff tear at bursal side. Partial thickness tears of the rotator cuff may involve either the articular surface, bursal surface or both sides of the rotator cuff or can be intratendinous. These can be distinguished by T1-weighted magnetic resonant imaging (MRI). An increase in signal in the rotator cuff without evidence of tendon discontinuity is suggestive of a partial tear. The progress of partial thickness rotator cuff tear appears to be worse with increasing age, a larger initial tear size and the absence of a traumatic episode. The risk of progression of a partial thickness tear to a full thickness tear is significant and it ranges between 28% to 81%.3 Non-operative treatment for partial thickness rotator cuff tear is similar to shoulder impingement syndrome. However, clinicians must be careful about repeated injection of steroid as this may weaken the tendon and accelerate the progression to full thickness tear and cause more symptoms. For patients who failed conservative treatment, surgical interventions by shoulder arthroscopy include arthroscopic debridement, debridement with subacromial decompression, arthroscopic repair of partially torn rotator cuff and completion of partially torn tendon then repair with suture anchors are the accepted operative choices.4 The choice of these operative procedure is usually based on patient’s age, physical demand, the location and size of partial thickness rotator cuff tear. Full thickness rotator cuff tearRotator cuff tear can occur after an acute traumatic event or gradually with chronic tendinopathy. Night pain and weakness are classical features of full thickness rotator cuff tear. Physical examination should focus on the discrepancy between active and passive shoulder range of motion and rotator cuff power. Supraspinatus tendon power is tested by an empty can test (30 degrees shoulder forward flexion and internal rotation). Infraspinatus tendon tear usually presents as weakness of external rotation power. (Figure 2) Subscapularis tear presents as weakness of internal rotation. Several tests including the belly press test, the lift off test and the bear hug test (Figure 3) can demonstrate weakness of subscapularis muscle power. 
Both ultrasound and MRI can provide accurate diagnosis of rotator cuff tear. MRI can confirm the location and degree of tear, whether there is retraction of tear and the quality of tendon. Acute traumatic full thickness tear is best managed surgically by rotator cuff repair. Both open and arthroscopic rotator cuff repair give equally good clinical outcome.5 Arthroscopic surgery has the advantage of shorter hospital stay and faster recovery time. Patients with chronic rotator cuff tear should first be offered conservative treatment with NSAID and physical therapy for a period of 6 to 12 weeks. Those who have failed conservative treatment and experience persistent shoulder pain, weakness and limitation in daily activities should be offered rotator cuff repair operation. Massive rotator cuff tearMassive rotator cuff tear is defined as two or more tendon tear or tear size larger than 5cm.6 Even after surgical repair of these rotator cuffs, the retear rate approaches 50%.7,8 Radiologically, there is proximal migration of humeral head with break in the gothic arch. (Figure 4) Weakness rather than pain is predominant. Clinically, there is significant atrophy of supraspinatus and infraspinatus muscle bulks. The rotator cuff muscle power is very weak and often there is a positive drop arm sign where the patient is unable to hold active forward flexion of shoulder. In the MRI, irreparable features of massive rotator cuff tear include tendon retraction beyond the glenoid rim, muscle atrophy and fatty infiltration of more than 50%. (Figure 5) Non-operative treatment with NSAID, physiotherapy, subacromial injection of corticosteroid can be offered to elderly patient with low functional demand. A wide range of surgical interventions with different levels of surgical complexity may be performed. These include arthroscopic debridement, subacromial balloon insertion, partial repair of rotator cuff, graft repair, tendon transfer, superior capsular reconstruction and reverse total shoulder arthroplasty. The optimal surgical interventions for massive rotator cuff tear should be individualised and determined by orthopaedic surgeons specialised in the shoulder. 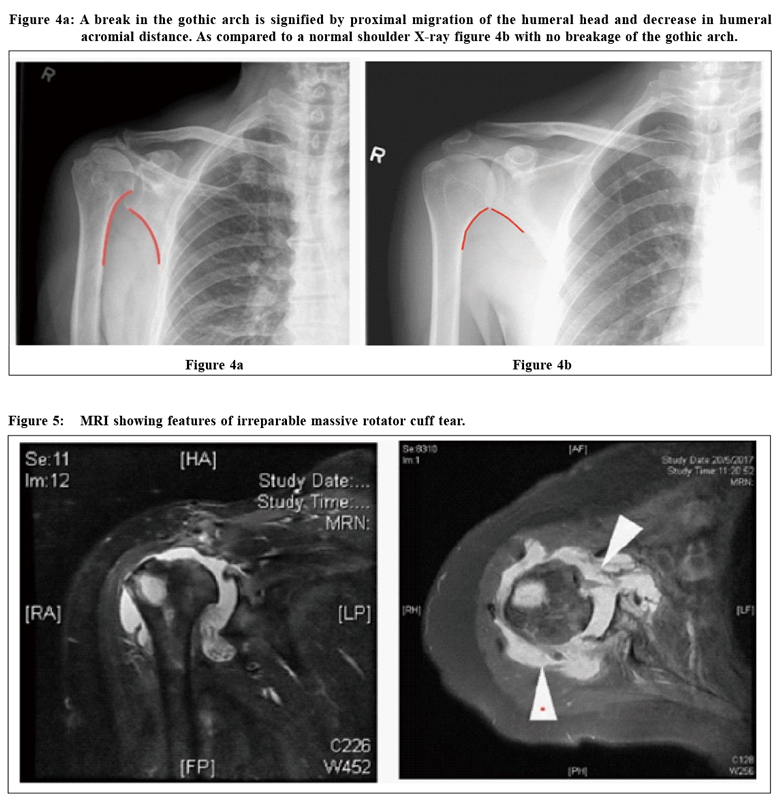
Biceps pathology Superior labrum anterior to posterior (SLAP) lesion is common in young throwing athletes or after a traumatic event. A tear in the proximal biceps anchor occurs at the 12 o’clock of the glenoid face. The most prevalent complaints include anterior shoulder pain, clicking and popping in the shoulder. A positive O’Brien test is suggestive of a SLAP lesion.9 Magnetic resonance arthrogram improves the sensitivity and specificity of the diagnosis of a SLAP lesion. Non-operative treatment with physical therapy directed at posterior capsular stretching is the mainstay of initial treatment. Surgical intervention with arthroscopic debridement or repair depends on the different subtypes of SLAP lesions. 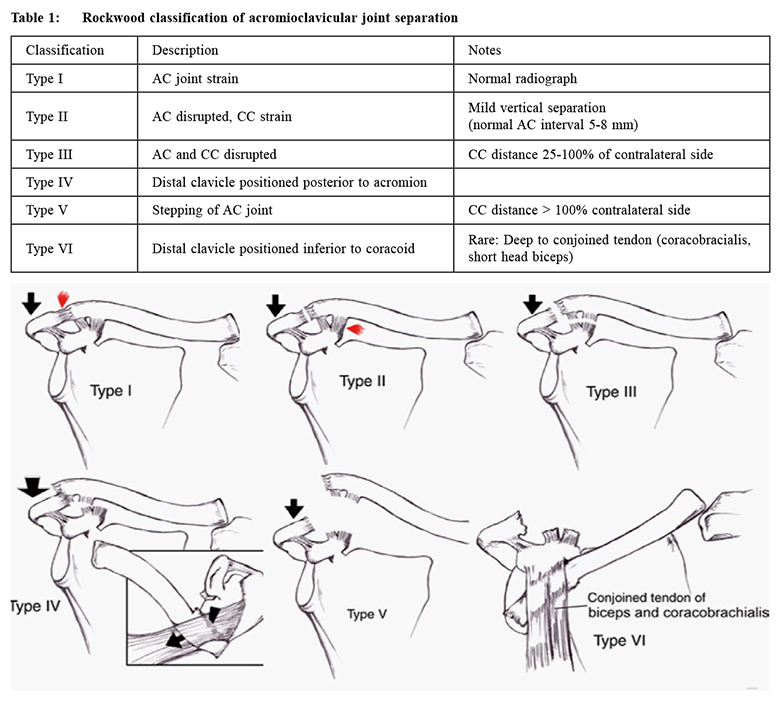
Biceps tendonitis involves inflammation of the tendon within the bicipital groove. It is associated with shoulder impingement syndrome and rotator cuff disease. Anterior shoulder pain with tendinosis at the bicipital groove on palpation is the hallmark of biceps tendon pathology. The pain is worsened with lifting and overhead activities. Speed test (resisted shoulder forward flexion with elbow in extension) and Yergason's test (resisted supination with elbow in flexed position) are provocative tests which help to make the diagnosis of long head of biceps pathology. Ultrasound can detect increased fluid signal in bicipital groove and tendinopathy change of long head of biceps tendon. In MRI, loss of sharp delineation of the tendon indicates biceps tendon pathology. Most biceps tendinitis responds well to traditional method of rest, ice and NSAID. If conservative treatment fails after 3 months, surgical treatment can be considered. Arthroscopic debridement, tenotomy (surgical release) of proximal biceps tendon and tenodesis (reattachment) of long head of biceps tendon are different surgical options. Typically, tenotomy is reserved for elderly sedentary patients with larger body build, whereas tenodesis is indicated in younger active patients who require full elbow flexion and supination strength.10 Acromioclavicular joint pathologyAcromioclavicular joint (ACJ) injury is common following direct contusion to the shoulder. The presenting symptom is shoulder pain maximum at the ACJ with limited shoulder range of motion. ACJ separation is managed according to the Rockwood classification (Table 1). Plain radiograph of bilateral zanca views for comparison with the unaffected side is needed. Type I and II ACJ injury can be treated successfully with non-operative treatment. Treatment of type III ACJ injury is controversial. Usually surgical intervention is offered if conservative treatment has failed or if patient has high physical demand. For type IV, V and VI ACJ separations, the trapezius fascia is disrupted, operative treatment is preferred in order to obtain the best clinical results. Many ACJ stabilisation technique by direct and indirect methods have been described in the literature. Shoulder arthroscopic assisted ACJ stabilisation is one of the more popular methods nowadays (Figure 6). ACJ arthritis can be a source of shoulder pain when the articular disc of the ACJ is torn. Shoulder pain occurs at end range of shoulder abduction and during overhead activities. Physical examination shows localised tenderness at the ACJ and cross arm test is positive. Lignocaine test by injection of lignocaine (1%, 2cc) directly into the ACJ can help to make the diagnosis. Conservative treatment includes activities modification, NSAID and physical therapy. If the above has failed, ACJ excision may be performed by open surgery or arthroscopically as an isolated procedure or in combination with other subacromial and rotator cuff procedures.11 
Calcified Tendinitis Calcified tendinitis has an unknown aetiology. It is characterised by the accumulation of calcium phosphate crystal within the rotator cuff tendons. Patients with calcific tendinitis will complain of pain and loss of range of motion during the resorptive phase. Patients are usually able to localise the pain and point to the site of maximal tenderness. Physical examination may exhibit significant tenderness in the area of affected tendon. Impingement signs are frequently present and some may demonstrate catching sensation. Both plain radiograph and ultrasound show calcification within the tendon. The mainstay of treatment is ice, rest and NSAID. Extracorporeal shock wave therapy is an non-invasive alternative prior to surgical intervention.12 In refractory cases with failed conservative treatment, ultrasound guided aspiration of calcified material13 or arthroscopic debridement of calcified tendon together with subacromial decompression can provide a long term pain relief.14 Scapular PainThe most common causes of scapular pain are muscle strain and referred pain from cervical spinal nerve root or dorsal scapular nerve pathology. It is characterised by a dull ache, burning or stabbing pain at the scapular region of the shoulder. In athletes who repetitively use their arm for overhead motion such as throwing, swimming or swinging a racket may lead to abnormal muscle contracture of the shoulder causing scapular dyskinesia. A good exposure of both shoulders and examination from behind can detect the asymmetrical shoulder scapular movement. The affected scapular blade may appear more prominent than the opposite one. Physical examination must include examination of the cervical spine as well as a full upper limb neurological examination. The mainstay of treatment is physiotherapy involving posterior capsular stretching and scapular muscle strengthening exercise. ConclusionUnderstanding the shoulder anatomy and the typical presentation of various shoulder pathologies help in deriving the correct diagnosis. Lignocaine and steroid injection is a particularly useful clinic procedure in the management of shoulder pain. Further investigations including plain radiograph, ultrasound or MRI should be performed after a traumatic event or when there is persistent symptoms after conservative treatment.
Stephen C Y Chung, MBBS (HK), MScSMHS (CUHK), FRCSEd (Orth), FHKAM (Orthopaedic Surgery)
Correspondence to: Dr Stephen CY Chung, Associate Consultant, Princess Margaret Hospital, 2 Princess Margaret Hospital Road, Hong Kong SAR.
References:
|
|