
|
March 2019, Volume 41, No. 1
|
Discussion Paper
|
Unto the next generation: the lifelong legacy of preterm birthNeena Modi HK Pract 2019;41:21-24 SummaryThis paper is based on the James Hutchison Memorial Lecture 2018 delivered by the author to the Hong Kong Paediatric Society on 27th March 2018. I discussed the current knowledge of the cardio-metabolic phenotype of the young adult who was born preterm, possible causal mechanisms and the implications for families, clinicians and researchers. 摘要本文是作者基於2018年3月27日在香港兒科學會舉辦的2018年度James Hutchison紀念講座發表的講詞。我討論了那些早產兒在他們長大成為年輕成人時心臟代謝表型的現有知識,可能的因果機制,對家庭,臨床醫生和研究人員的影響。 IntroductionThe number of preterm births is rising globally, with several countries including Indonesia, Pakistan, Zimbabwe, Gabon, Botswana, Mozambique and the Congo, now reporting rates in excess of 15%.1 It is estimated that worldwide there are around 15 million preterm births each year. Prematurity is now a leading cause of under-5-years-old mortality, but at the same time the number of survivors is increasing.2 The number of preterm children represented in the total population pool is therefore growing and their long term health is becoming an increasingly important issue. Preterm birth is well known to be a risk factor for later neurocognitive, developmental and psychological difficulties, and an increased risk of poor respiratory health. Here, I will discuss the current state of knowledge about the cardio-metabolic phenotype of the young adult who was born preterm, the possible causal mechanisms for these characteristics, and the implications for families, clinicians and researchers. The phenotype of the young adult born pretermEpidemiological studies from around the world showed an increased prevalence of disorders indicative of disruption to multiple organ systems and biological pathways, in young adults who were born preterm. In an individual participant study, the authors found that in comparison with full-term counterparts, young adults born very preterm are more likely to have higher systolic and diastolic blood pressures.3 Strong corroboratory evidence was noted in a systematic review and meta-analysis of published studies worldwide.4 In this study the authors identified a mean (95% confidence interval) increase in systolic blood pressure of 4.2 (2.8, 5.6) mm Hg, and a mean increase in diastolic blood pressure of 2.6 (1.2, 4.0) mm Hg in children and young adults born preterm.4 Young adults born preterm have been shown to have an altered cardiac morphology, including shorter ventricles, smaller internal ventricular cavity diameters, with reduction in left and right ventricular function.5 Studies of arterial stiffness have to date been inconclusive, with some, but not all, investigators identifying increased stiffness and other markers of aberrant development in young adults born preterm.6-9 However, studies have been conducted at different ages and involved the interrogation of different blood vessels, which may account for some of the variability in findings. Other observations indicate of altered cardiovascular development include a reduction in dermal capillary density, a possible mediator of higher blood pressure.10 Li et al in a systematic review and meta-analysis of confounder adjusted observational studies, showed an increased relative risk (95% CI) of both type 1 (1.18; 1.11, 1.25) and type 2 diabetes (1.51; 1.32, 1.72) in the preterm populations.11 Associations have been found between preterm birth and higher total cholesterol, LDL cholesterol, and apolipoprotein in adolescent boys.12 Data from a Swedish registry study involving over 14 thousand men and women born in Uppsala between 1915-1929, showed shorter length of gestation to be associated with higher mortality from cerebrovascular disease, particularly occlusive stroke.13 Another study utilising Swedish birth registry data showed birth before 32 weeks is associated with nearly twofold increased risk of cerebrovascular disease compared to term born individuals (adjusted Hazard Ratio (95 % CI) 1.89 (1.01-3.54) (1,306,943 men and women born 1983-1995).14 Boivin et al described an increase in pregnancy complications, including gestational diabetes, gestational hypertension, pre-eclampsia and eclampsia, in women born preterm.15 Women, themselves born preterm, are at an increased risk of giving birth prematurely, and reproductive rates are reduced in both men and women born preterm16; thus passing on the legacy of preterm birth to the next generation. Crump et al17 also identify a highly statistically significant relationship between all-cause mortality and the degree of immaturity in young adults. There is some evidence of a dose response relationship between adverse health outcomes and prematurity. Thus the reproductive relative risk for extremely preterm (born ≤27 weeks gestation) compared with term men is 0.24 (95%CI 0.17, 0.32), whereas for men born very preterm it is 0.7 (0.66, 0.74).16 Equivalent figures for extremely and very preterm women are 0.33 (0.26, 0.42) and 0.81 (0.78, 0.85).16 Similarly, the adjusted odd ratios (95% CI) for high systolic BP (140 mm Hg) varies in young men by gestational age at birth, with the most immature the most affected; 33-36 weeks: 1.25 (1.19, 1.30); 29-32 weeks: 1.48 (1.30, 1.68); 24-28 weeks 1.93 (1.34, 2.76).18 Possible biological mechanismsOver a decade ago, by chance observations were made that preterm babies, when studied at their “fullterm” age, had a body composition characterised by an excess of internal-abdominal adipose tissue, and a markedly elevated intra-hepatocellular lipid content.19 Subsequently the same features were identified in another cohort, a group of young, healthy adults who had been born very preterm.3 At the same time, other research groups around the world were identifying evidence of impaired glucose tolerance and insulin resistance in children and adolescents born very preterm or in those who were born with a very low birthweight.20,21 Our data suggested that altered adiposity and hepatic lipid accumulation might be biological mechanisms contributing to insulin resistance and glucose intolerance. The early onset of phenotypic characteristics typically associated with aging has led us to propose that preterm birth results in accelerated aging. We have recently obtained corroboratory molecular evidence with the finding that there is a preponderance of shorter telomere lengths in young adult men born preterm (unpublished data) in keeping with data from other investigators.22 Many possible mediators might explain these clinical and epidemiological observations. For example, alteration of the microbiome through antibiotic use, or enteral feed exposures might affect the development of the immune function23, and/or future intestinal energy harvesting24 leading to seemingly disparate disorders such as type 1 diabetes (immune-related) and type 2 diabetes (metabolism-related). Early nutrition with the provision of too much, or too little, protein and lipid have several plausible down-stream and long-term effects. Oxidative stress, chronic inflammation, disrupted sleep cycles similarly have the potential to perturb multiple biological pathways. Such exposures may induce permanent effects through, for example, epigenetic changes in somatic and/or germ cell lines leading to altered gene expression, or through structural changes, e.g. in micro-vasculature, leading to organ dysfunction. Conversely, other exposures, for example breast-feeding, may have a beneficial impact.25 What are the clinical implications of evidence to date?Raised blood pressure, raised intra-hepatocellular lipid, excess internal-abdominal adiposity and insulin resistance are markers of the metabolic syndrome, a now well-recognised and growing cause of chronic non-communicable disease and deceased life span. 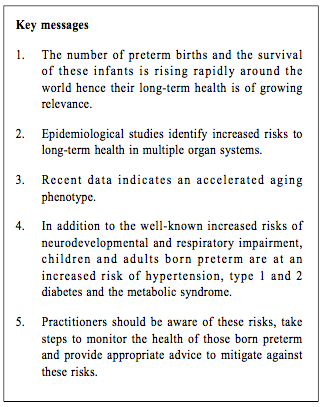
The increase in intra-abdominal adiposity in outwardly healthy young adults we have shown in replicated studies, and the epidemiological evidence of greater vulnerability of the preterm population to the metabolic syndrome and related conditions is of an important clinical relevance. In a follow-up cohort study for example, an increase in internal-abdominal adiposity of around 370g was associated with an 80% higher risk of death within five years, having adjusted for subcutaneous adiposity and hepatic lipid.26 Similarly, every 2mmHg rise in systolic BP is associated with a 7% increase in mortality from ischaemic heart disease and a 10% increased risk of stroke.27 It would seem that at the very least, healthcare professionals should take the opportunity when pre-term babies attend the follow-up clinics to check their blood pressure and to advise parents and in due course, the young people themselves about life-style choices that might mitigate some of the excess risks to which they are vulnerable. Healthcare professionals should be aware of the increased risk of developing metabolic disorders among those born preterm. For example a recent study utilizing Taiwan’s universal National Health Insurance Research Database from 1996 to 2004, showed that those born preterm had risks of hypertension, type 2 diabetes, type 1 diabetes and hyperlipidaemia ranging from 1.8 to more than 3 times that of healthy full-term infants.28 Neonatologists and other healthcare professionals responsible for the care of preterm babies should also be mindful that much of our current practice have a limited evidence base; for example, the optimum protein intake for very preterm babies is unknown, as is the optimum rate of postnatal growth and the long-term impact of exposure to exogenous probiotic species. Inadequately evidenced care is a major patient safety issue. Clinical research showing many widely accepted practices to be harmful have led to complete overturning of “consensus” or “expert opinion” based approaches. Examples of previous accepted, but now rejected practices include the routine use of oxygen for newborn resuscitation, separation of mother and baby, bicarbonate in the management of respiratory distress syndrome, and postnatal steroids in chronic lung disease. The inescapable conclusion is that much of preterm care remains experimental. What research is needed now?Longitudinal clinical studies are required, with deep phenotyping of preterm infants to identify candidate biomarkers of outcome and their predictive value, and care practices that may be contributing to favourable or adverse outcomes. These care practices then need testing in adequately powered comparative effectiveness trials; for example, there is suggestion that early exposure to intravenous lipid may contribute to cardiovascular risk29 and excessive protein intake to intra-abdominal adiposity30 and glomerular hyperfiltration31, leading respectively to the metabolic syndrome and renal impairment. ConclusionsThere is growing evidence of a higher prevalence in preterm populations of conditions typically associated with aging. Epidemiological and clinical observations suggest disruption to multiple biological pathways and organ systems. A challenge for neonatology is to identify candidate effector mechanisms, and test interventions and care practices in rigorous randomised controlled trials in order to improve life-long health prospects for this vulnerable patient group.
Neena Modi, MD, FRCP, FRCPCH, FFPM
Correspondence to: Prof Neena Modi, Section of Neonatal Medicine, Cheslsea and Westminster Hospital campus, Imperial College London, 369 Fulham Road, London SW10 9NH, United Kingdom.
References:
Funding: The author’s research noted in this paper was supported by grants from the Westminster Medical School Research Trust and British Heart Foundation. |
|