
|
December 2020,Volume 42, No.4
|
Case Report
|
A middle aged man with an unusual cause of hip and knee pain: a case presentationDavid CH Cheung 張志康 HK Pract 2020;42:94-98 SummaryHypertrophic pulmonary osteoarthropathy (HPOA) is a rare disease which is seldom seen in the primary care setting. However it can be diagnosed, if we pay attention to the history of a patient. This case presentation is typical of the disease. Early diagnosis and management may lead to a better clinical outcome. 摘要肺性肥大性骨關節病是一種稀有疾病,在基層醫療中少見。但如我們留意病人的病史,它可被診斷出來。本報告陳述一宗典型病例。及早診斷和治理可帶來更佳的臨床效果。 The caseA 63-year-old man with a past medical history of colonic polyp in 2015, alcoholic liver disease and hypertension complained of right hip and knee pain for 6 months. The pain became worse when walking upstairs and walking for more than 10 minutes on level ground. There was some slight pain at rest. There was no history of injury, numbness nor knee swelling. He was a chronic smoker with 50 pack years of cigarette smoking. He quitted drinking after he was diagnosed with alcoholic liver disease. His only long term medication was amlodipine 5mg daily. Physical examination found that he walked with an antalgic gait. There was no hip or knee deformity. His right hip was non tender on palpation, the active ranges of motions were full and without pain. However, his right thigh was tender on palpation, but no swelling was felt. The right knee was also not tender on palpation, no effusion or crepitation, and active ranges of motions were full. X rays of his right hip and right knee were ordered. Analgesic balm and paracetamol were given as symptomatic relief. X-ray of his right hip and knee showed laminated periosteal reaction along the femoral diaphysis, proximal tibia and fibula. No displaced fracture or dislocation was seen. Features were suggestive of hypertrophic pulmonary osteoarthropathy. (Figures 1a and 1b) At the follow-up consultation, the doctor inquired about his respiratory symptoms. In fact he had suffered intermittent cough for 6 months. He had had mild whitish sputum. There was no haemoptysis, no shortness of breath at rest, no weight loss and no fever. On physical examination he was not found to be clinically dyspnoeic. There was no palpable cervical lymph nodes and auscultation of his chest was clear with good air entry. However, there were gross finger clubbing in both hands. An urgent chest X ray was ordered in view of his hip and knee X ray findings and a given history of prolonged cough in a smoker. The chest X ray report showed a 6.3cm x 6.5cm spiculated mass the right middle zone, (Figure 2). This was highly suspicious of malignancy and an urgent referral was made to the Internal Medicine Specialist 

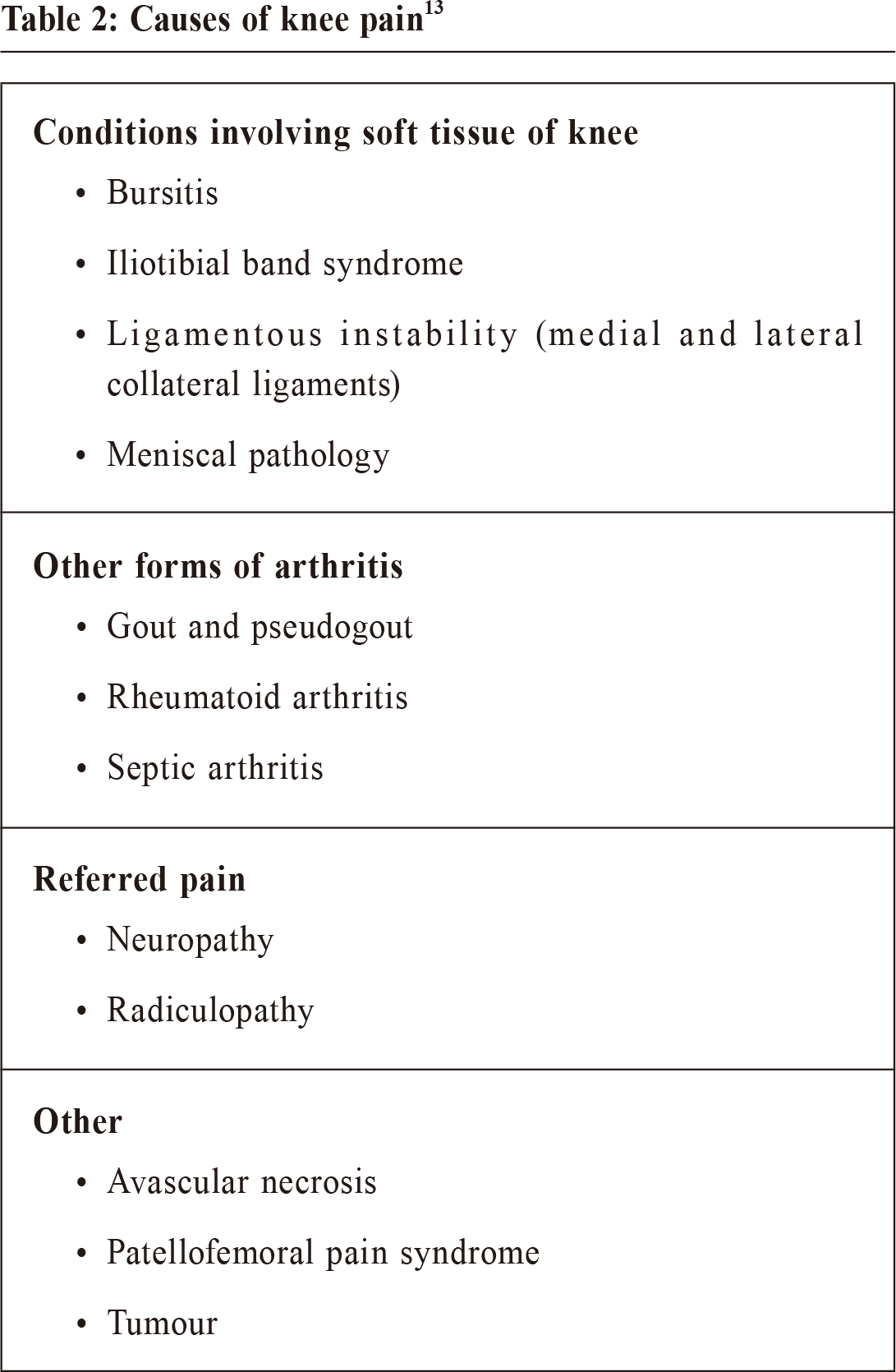
Clinic. CT thorax showed a 8cm right upper lobe mass extending into his right middle lobe and right lower lobe with mediastinal lymph node enlargement and emphysematous changes. Transbronchial biopsy showed adenocarcinoma. Unfortunately he died of lung cancer one month later. DiscussionHypertrophic pulmonary oeteo-arthropathy is a group of symptoms that can affect the organs, lungs, bones and joints. It is also called Bamberger–Marie syndrome or osteoarthropathia hypertrophicans. HPOA is a paraneoplastic syndrome most commonly found in people with non-small cell lung cancer.1 Less than 1% of lung cancer patients develop HPOA . Men who smoked heavily and who has advanced lung cancer predominates those with HPOA.2 The signs of the condition include swelling of the ends of the fingers (called clubbing), spoonshaped nails and inf lammation, swelling and pain in the hands, fingers, knees or ankles. Finger Clubbing is characterised by bulbous enlargement of termina segments of the fingers and toes due to proliferation of subungual connective tissue.3 X ray shows periosteal thickening occurs along the shafts of long and short bones, appearing initially in the distal diaphyseal regions of the long bones.4 The causes of periosteal reaction are broad; including trauma, infection, arthritis, tumours, and drug-induced and vascular entities. In HPOA it typically produces a periosteal reaction that is symmetrical and widely distributed. It typically involves the diaphyses of tubular bones, sparing the ends. It should be associated with finger clubbing, enlargement of the extremities and swollen joints.5 HPOA can be confirmed by the use of bone scintigraphy because of its higher sensitivity to X ray.6 The typical finding is a symmetrical, abnormally high uptake in the diaphysis and metaphysis of long bones. Adenocarcinoma of the lung is the most frequent histological type, followed by squamous cell carcinoma. Small cell carcinoma is the least frequent type which is associated with HPOA. 6 Vascular endothelial growth factor (VEGF) produced by the tumour is a cytokine which can lead to vascular hyperplasia, new bone formation and edema. This is suggestive in the pathogenesis of HPOA.7 Excision of lung cancer with high levels of VEGF causes a disappearance of the skeletal abnormalities and reduction in VEGF level.8 The management of HPOA would be to treat the underlying cause, and the pain will relief itself. As medical treatment, non-steroidal anti-inflammatory drugs (NSAIDs) may be helpful for the painful osteoarthropathy in controlling the symptoms but treatment with bisphosphonate such as zoledronic acid would be a better alternative.9 The pain associated with HPOA can occasionally be disabling and often refractory to conventional analgesics if the primary cause is not treated.10 Finally, the survival rates between lung cancer patients with and without HPOA are similar.11 In this case, our patient presented with hip and knee pain, which was due to periostitis secondary to the paraneoplastic effect of his lung carcinoma. Primary care physicians should always bear in mind the possible malignant causes of hip and knee pain so that this important diagnosis would not be missed. The causes of hip and knee pain are shown in Table 1 and Table 2 respectively. 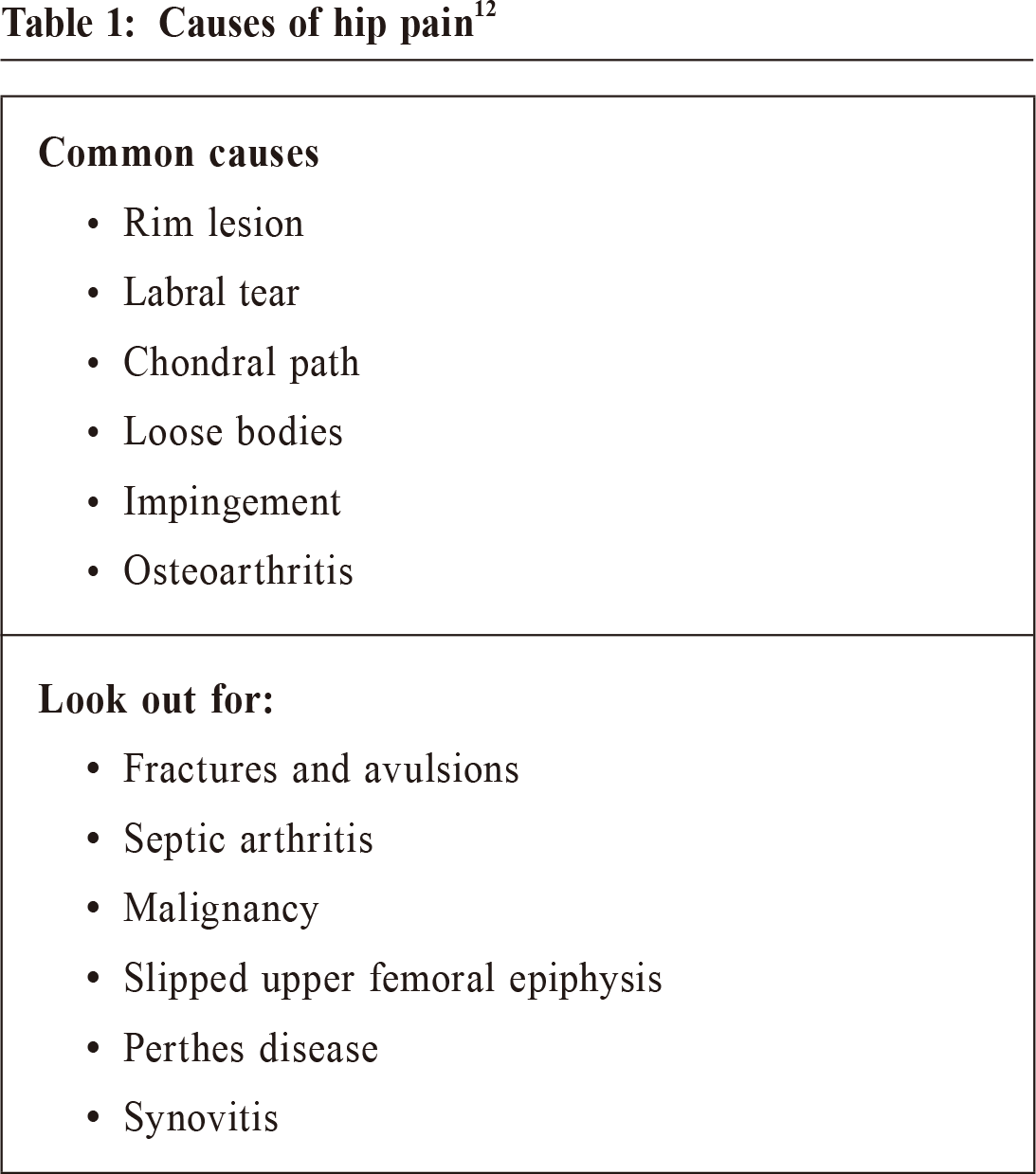
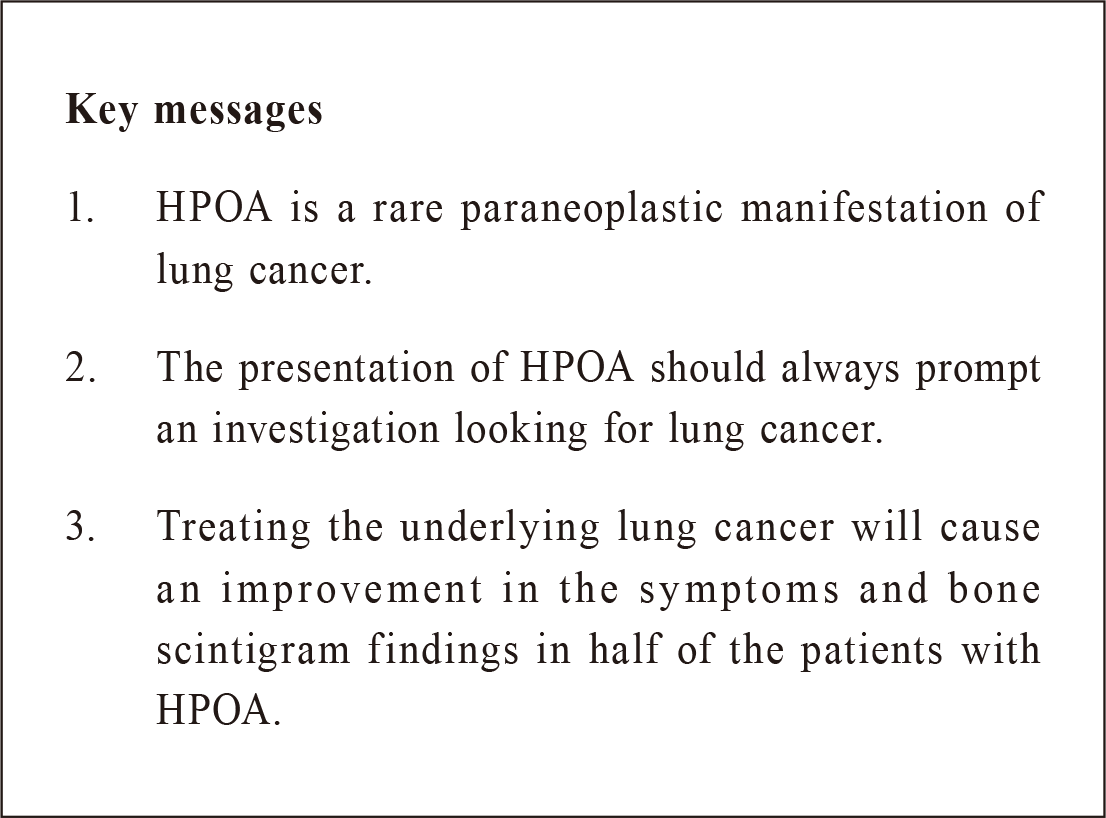
ConclusionLung cancer is becoming commoner nowadays with an aging population. Although we may just be aware of the typical symptoms of lung cancer, its presentation as a paraneoplastic syndrome should not be forgotten. Clinicians should bear this diagnosis in mind. Once this condition is suspected a prompt search for lung cancer must follow.
David CH Cheung, MBBS (HKU), FRACGP, FHKCFP, FHKAM (Family
Medicine)
Correspondence to:Dr. David CH Cheung, 10 Aberdeen Reservoir Road, Aberdeen,
References
|
|