Multi-morbidity and its associations with
healthcare service utilisation and glycaemic
control in diabetic patients in a primary
care clinic in Hong Kong
Cheuk-chung Sung 宋卓聰,Tsun-kit Chu 朱晉傑,Jun Liang 梁峻
HK Pract 2020;42:77-86
Summary
Objective:
Multi-morbidity is common among diabetic
patients and often complicates its treatment. The
objectives of this study were: (1) to investigate the
magnitude of multi-morbidity among patients with
Type 2 diabetes, and (2) to examine its relationship
with glycaemic control and public healthcare service
utilisation.
Design:
A cross-sectional study, retrospectively
analysing electronic medical records
Subjects:
A random sample of 386 adults, aged 18
or over, with Type 2 diabetes who attended a General
Out-patient Clinic (GOPD) in Hong Kong, for their
diabetic follow-up between 1 January 2014 and 31
December 2015.
Main outcome measures:
The outcome measures
were the number of co-existing chronic conditions,
glycaemic control (as measured by HbA1c) and
healthcare service utilisation (as measured by the
number of attendances for medical consultations in
the General Out-patient Clinics, Specialist Out-patient
Clinics, Accident and Emergency Departments, and
number of unplanned hospital admission episodes)
within the reported period. Other data collected were
the number of chronic medications (polypharmacy),
and patient demographics including age, gender, body
mass index (BMI) and smoking status. Regression
analyses were used to analyse the associations
between multi-morbidity and HbA1c level and public
healthcare service utilisation.
Results:
Multi-morbidity was observed in almost all
(99.2%) patients in our sample, with 91% of them
having two or more co-existing conditions. The
four most common co-existing conditions were
hypertension, hyperlipidaemia, visual conditions
and chronic kidney disease. After adjusting for
age, sex, BMI, smoking status and the presence of
polypharmacy, an increase in number of co-morbid
conditions significantly increased the healthcare
service utilisation in secondary care. The number of
co-existing conditions had no statistically significant
association with the glycaemic control or the number
of attendances to General Out-patient Clinics.
Conclusions:
The magnitude of multi-morbidity
is associated with healthcare service utilisation,
independent of the presence of polypharmacy. This
study highlighted the importance of adopting a
multidisciplinary and holistic patient-centred approach
when managing patients with diabetes.
Keywords:
Diabetes, multi-morbidity, polypharmacy,
disease control, healthcare utilisation
摘要
目 標 :
糖尿病人經常伴有其他病患,而使治療變得複雜。本研究旨在:(1) 探研二型糖尿病人伴有其他病患的普遍性,和(2) 檢視其他病患與血糖控制及對公共醫療服務需求的關係。
設計 :
按病人的電子醫療紀錄作橫切面式,回顧性分析。
對象 :
隨機挑選386名18歲或以上,於2014至2015年間在香港一所普通科門診因二型糖尿病而覆診的病人進行研究。
主要結果測量 :
結果測量項目為長期並存病患的數目,血糖控制(按HbA1C量度),在研究期內對公共醫療服務的需要(包括前往普通科門診、專科門診、急症室求診和非預約入院的次數)。其他收集的數據有長期服用藥物的數量(多元藥物治療)和病人的統計學個人資料:包括年齡、性別、體重指數(BMI)和吸煙習慣。以還原分析法分析共存病患、血糖控制和對公共醫療服務需求的關係。
結果 :
在研究組別中,接近所有(99.2%)病人伴有其他病患。其中91%有兩種或以上不同病患。最常見的四種病症是高血壓、高血脂,視力障礙和慢性腎病。經調整年齡、性別、體重指數、吸煙狀況和使用多元藥物等因素後,發現並存病患的多少和對公共醫療服務需求有密切的直接關係。而它與血糖控制和往普通科門診次數則無明顯聯繫。
結論 :
共存病患的多少和對公共醫療服務的需求有相聯關係,但與服用多種藥物無關。本研究結果突顯在醫治糖尿病時,採納以不同專科匯診方式,並以病人為本作全人治療的重要。
主要詞彙 :
糖尿病,多種病患,多元藥物治療,疾病控制,醫療服務需求。
Introduction
The prevalence of diabetes in Hong Kong has
increased significantly over the past decade and in
2014, the overall prevalence of diabetes in Hong Kong
was 10.29%.1
Multi-morbidity, defined as the presence
of two or more chronic conditions2
, is increasingly
recognised as a major challenge in healthcare service
globally. A recent study undertaken in Hong Kong
showed multi-morbidity was commonly encountered in
the public General Out-patient Clinics (GOPDs), with
diabetes being the chronic condition which had the
strongest association with multi-morbidity.3
With an
ageing population, it is expected that the prevalence
of multi-morbidity will increase, along with the rising
burden and risks associated with polypharmacy.
Multi-morbidity often complicates diabetic
treatment and its outcomes, as evidenced by studies
undertaken with Caucasian subjects, which analysed
the relationship between multi-morbidity, diabetic
care goal achievement and healthcare utilisation.4-10
However, these associations are less studied in the
Asian population. Given the phenotypic variabilities,
it is important to study these associations in the local
population. Polypharmacy can increase the risk of
drug-drug interactions, and hence, the adverse drug
reactions, particularly in the older population and
those with multi-morbidity.11-12 Therefore, both multimorbidity and
polypharmacy create
significant concerns
for the individual as well as for the healthcare system.
The public General Out-patient Clinics in Hong
Kong manage a significant proportion of diabetic
patients in the locality.13 With diabetes shown to have
the strongest association with multi-morbidity in the
public GOPDs3
, further analysis on the multi-morbidity
pattern of diabetic patients is warranted. In addition,
there is no study published, in the literatures thus far,
on the association of multi-morbidity and glycaemic
control and healthcare service utilisation in the local
Chinese diabetic patients.
We hypothesised that the number of co-existing
conditions would be associated with poor glycaemic
control (as measured by HbA1c), and a higher degree
of healthcare service utilisations (as measured by the
number of medical consultation visits to the GOPDs,
Specialist Out-patient Clinics and Accident and
Emergency Departments, and number of unplanned
hospital admission episodes). We envisaged
polypharmacy as a potentially significant confounding
factor which would influence glycaemic control and
the degree of healthcare service utilisation. Therefore,
in addition to age, sex, BMI and smoking status, we
adjusted for the presence of polypharmacy in our
regression analysis.
Methods
Study Design and Population
This was a retrospective cross-sectional study
using electronic health record data of a computer
generated random sample of adult patients aged 18 or
over with Type 2 diabetes, who were followed-up in a
GOPD in Hong Kong within the period of 1 January
2014 (Time 0) – 31 December 2015 (Time 2 years).
Sample size calculation was determined by using the
following formula, using confidence level and margin
of error as 95% and 5% respectively14:-
n = Z2 x P (1 – P) / d2
where:
Z
= Z value, which is the standard normal variate.
For 95% confidence level, Z value is 1.96.
P
= expected prevalence of a condition in a
population in decimal. We set the P figure as 0.5, as
among our clinic patients requiring regular follow-up
appointments for chronic conditions, we estimated the
actual proportion with diabetes would not be more than
50%.
d
= absolute error or precision in decimal. As we
set the margin of error as 5%, the d figure is 0.05.
The sample size thus was calculated to be 384.
The Clinical Data Analysis and Reporting System
(CDARS) is one of electronic medical systems used in
the Hong Kong’s public healthcare service. A list of
Type 2 diabetic patients, i.e. those with International
Classification of Primary Care – 2nd Edition [(ICPC –
2) codes T89 and T90], who attended follow-up in our
clinic within the period between 1 September 2013
and 31 December 2013 was drawn from CDARS. We
believed a 4-month-pool of patient attendances was a
representative cohort because follow-up within 4-month-interval was our clinic policy.
430 patients (over 10%
greater than the calculated sample size) were randomly
selected from the list by computer generated random
numbers, as we anticipated that some cases had to be
excluded from our study. We excluded patients under
18 years of age, and patients with gestational or Type
1 diabetes, as well as the ones who died before Time
0, those who were actually followed up in Secondary
Care or in Private Sector, and the ones who were
misdiagnosed with diabetes. For the cases included, the
patients had to have at least 12-month-history of Type 2
diabetes before Time 0.
Definitions
The World Health Organisation (WHO) defined
multi-morbidity as the co-existence of two or more
chronic conditions in the same individual. 2
In this
study, a list of 28 chronic conditions was used to
identify patients with multi-morbidity (Table 1). These
28 conditions had included 14 chronic conditions shown
to be associated with multi-morbidity among patients
attending the Hong Kong General Out-patient Clinics3
,
as well as 15 chronic conditions, which were considered
prevalent in Singapore.15 Papers from Chu et al3
and
Subramaniam et al15 were chosen to formulate the
list of the chronic conditions since both Hong Kong
and Singapore have similar demographics and social
structure with the majority of the population being of
Chinese ethnicity. Both cities also are noted to have a
highly developed medical and economic infrastructure.
There is no consensus on the definition of
polypharmacy, and diverse definitions have been used
by researchers to date. The most commonly reported
definition of polypharmacy is a numerical definition
of five or more medications daily.16 In this study, we
adopted the definition of polypharmacy as 5 or more
medications daily as this had the advantage of being
simple and easily classified in clinical practice. As-required medications (e.g.
analgesics or symptomatic
treatment) as well as topical medications (e.g. emollient
for eczema) were excluded while counting a patient’s
total medication usage.

Data Collection
Data were collected by reviewing the medical
records and consultation notes in the period between
1 January 2014 (Time 0) and 31 December 2015 (Time
2 years). The review was performed by the principal
investigator. Whenever there were uncertainties with
the data, the records would be reviewed by the second
investigator, and any discrepancies were resolved via
discussion and consensus.
Our main explanatory variable was the number
of co-existing chronic conditions (ever diagnosed and
actively under treatment) collected at the time closest
to Time 0. The actual diagnoses of the co-existing
conditions were also recorded.
Our primary outcome variables were glycaemic
control (as measured by HbA1c) collected at the time
closest to Time 0, and the record of public healthcare
service utilisation between Time 0 and Time 2 years.
The parameters of healthcare service utilisation
included the number of attendances for medical
consultation in the public General Out-patient Clinics,
Specialist Out-patient Clinics, Accident and Emergency
Departments, as well as the number of unplanned
hospital admission episodes.
The covariates we collected were patient
characteristics, namely age, sex, BMI, smoking status
and the number of regular medications prescribed at the
time closest to Time 0.
Other data we collected but not used for our
analysis in this study were the new conditions
developed between Time 0 and Time 2 years, the actual
diagnoses and number of co-existing chronic conditions
and the number of regular medications at the time
closest to Time 2 years.
Statistical analysis
All analyses were conducted using Statistical
Package for the Social Sciences (SPSS). Regression
analyses were performed to analyse the association
between the number of co-morbid conditions and
HbA1c level and the degree of public healthcare service
utilisation, after adjusting for patient demographic
characteristics and the presence of polypharmacy.
Results
Study population
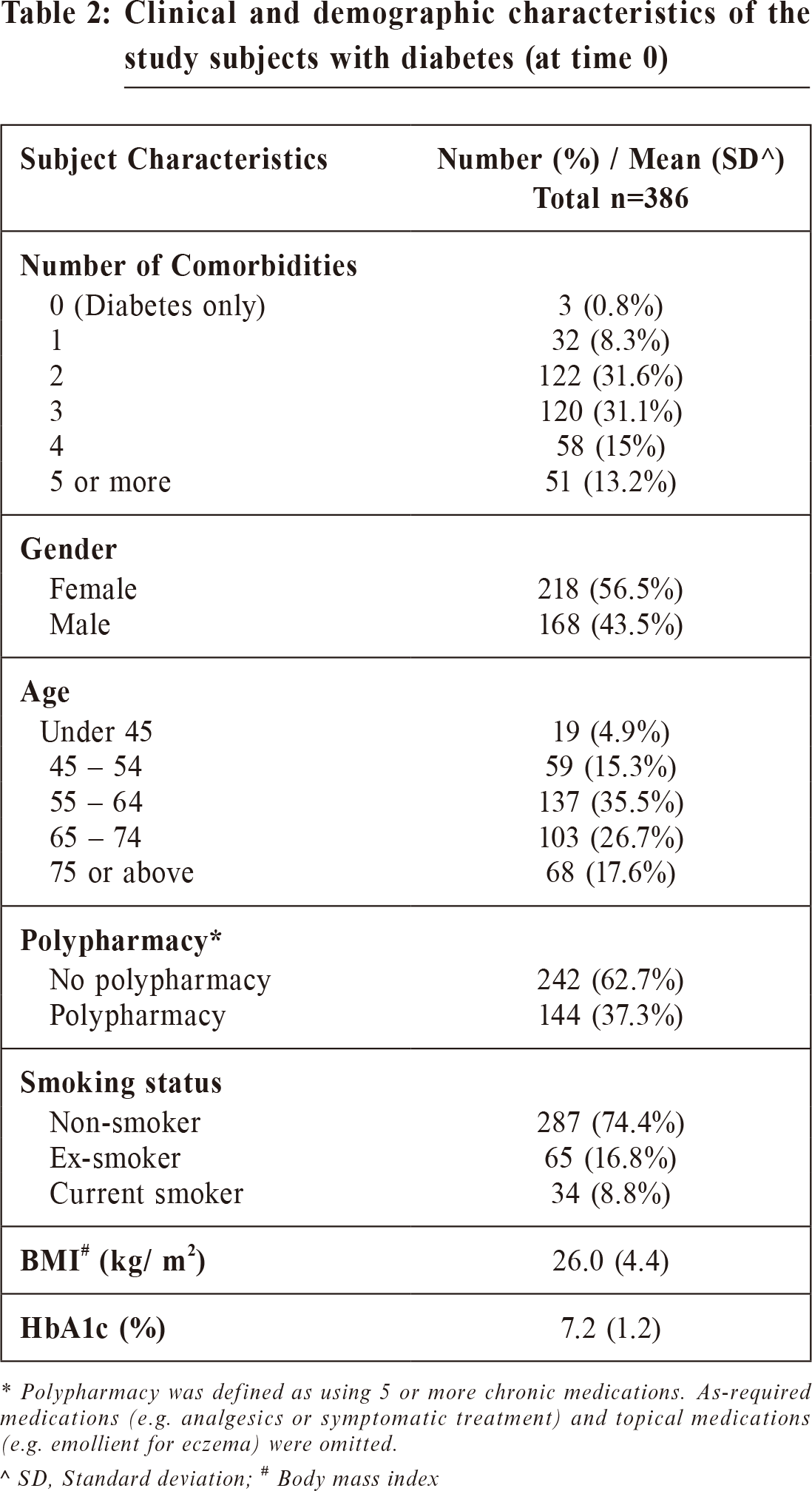
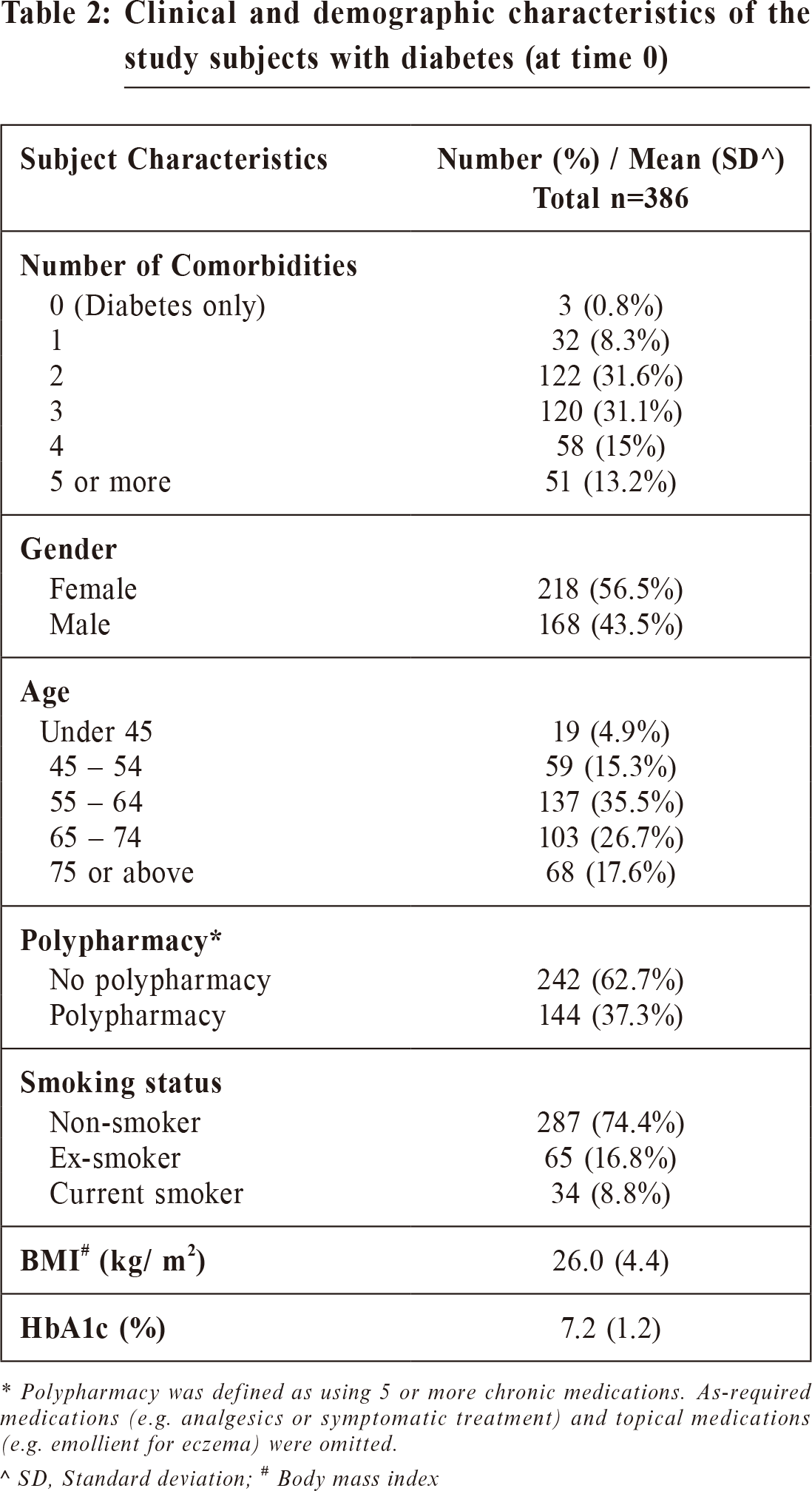
In total, we reviewed the electronic medical
records of 386 patients. At Time 0, the mean age was
63.4 years and 56.5% were female. Multi-morbidity
was observed in almost all subjects (n=383, 99.2%),
with a mean number of co-existing conditions of 3 per
person. Polypharmacy was observed in 144 (37.3%) of
patients, with a mean of 4.2 drugs per patient in the
study population. The mean HbA1c was 7.2% and the
mean BMI was 26.0 kg/m²
. 34 patients (8.8%) were
current smokers (Table 2).
Nature of multi-morbidity
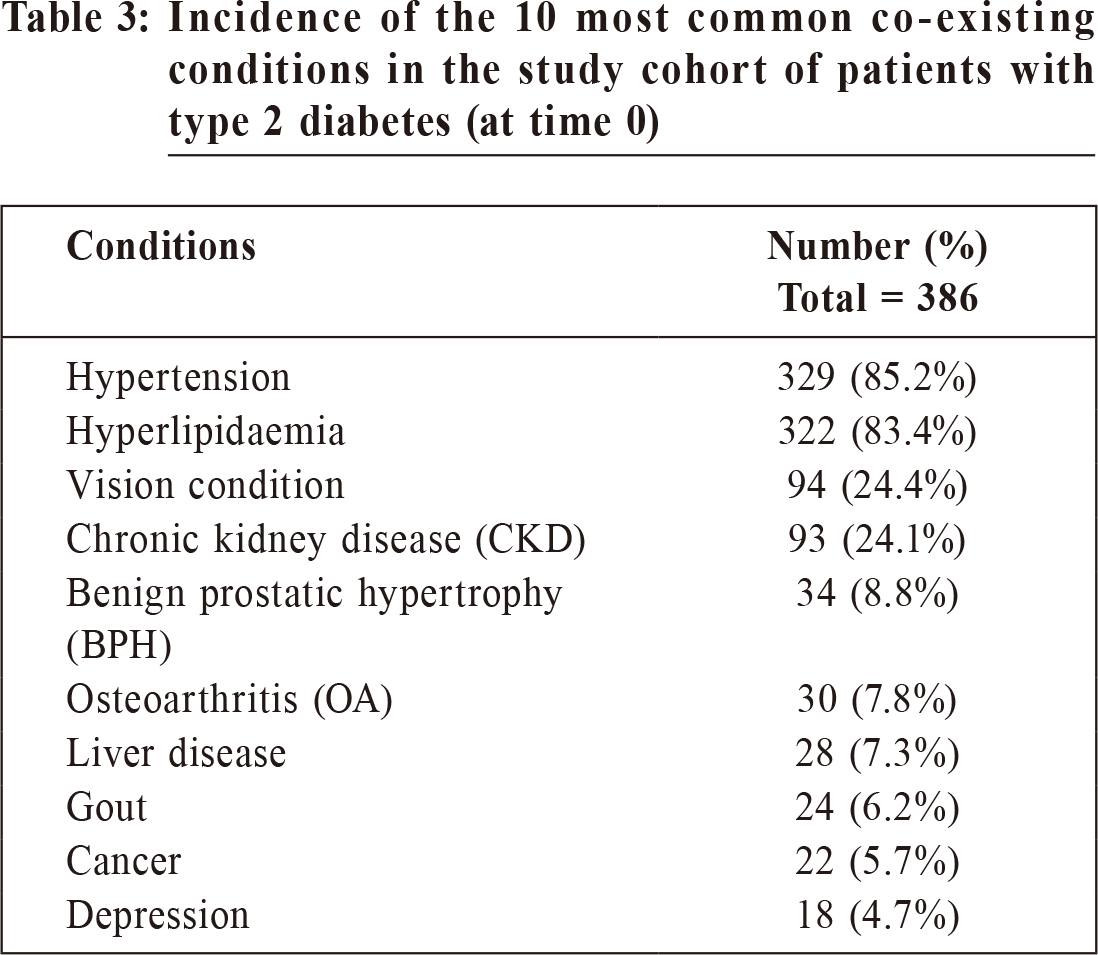
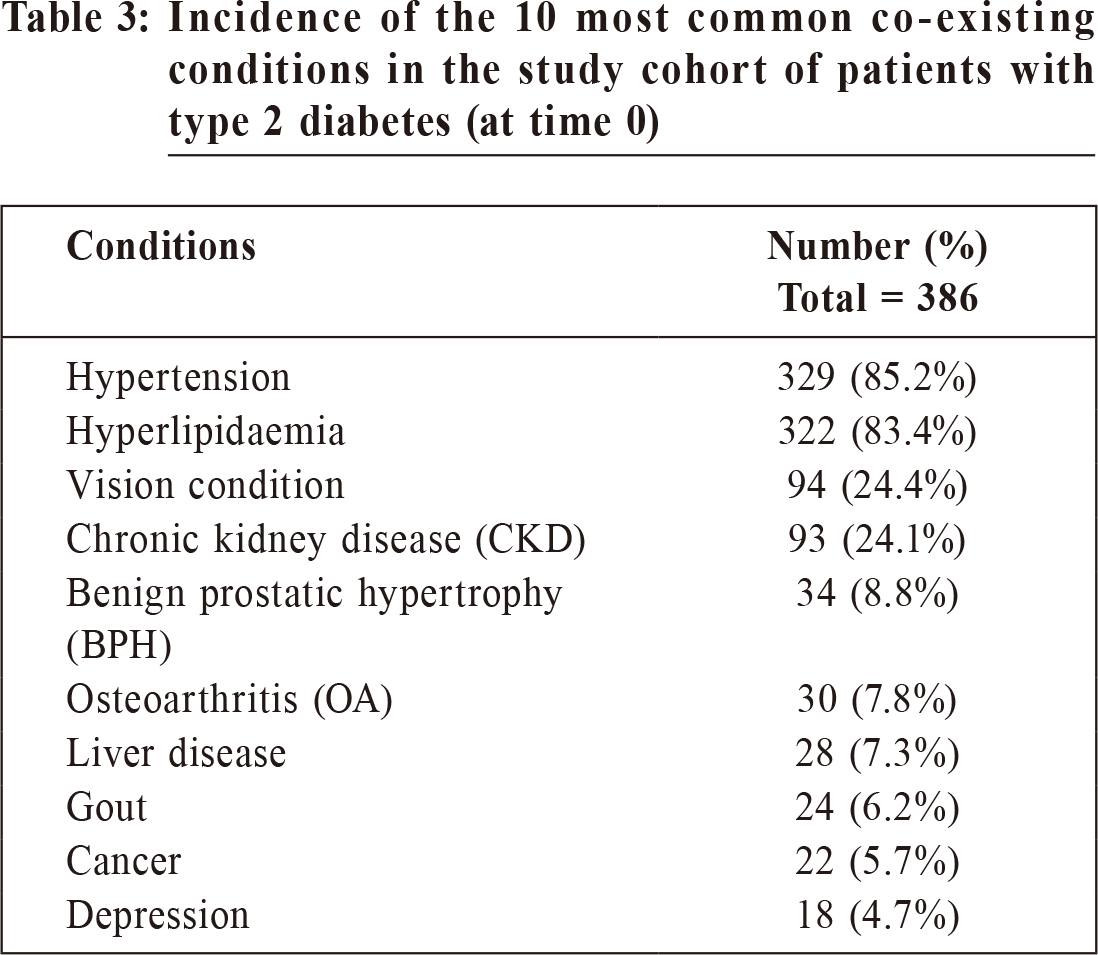
At Time 0 of our study period, of the 386 records
reviewed, the majority (n = 242, 62.7%) had 2 or 3
co-existing conditions. The four most common co-existing chronic conditions were
hypertension (85.2%),
hyperlipidaemia (83.4%), visual condition (24.4%) and
chronic kidney disease (24.1%). Other co-morbidities
were observed in less than 10% of the study population
(Table 3).
Association between number of co-existing conditions
and diabetes control, as measured by HbA1c
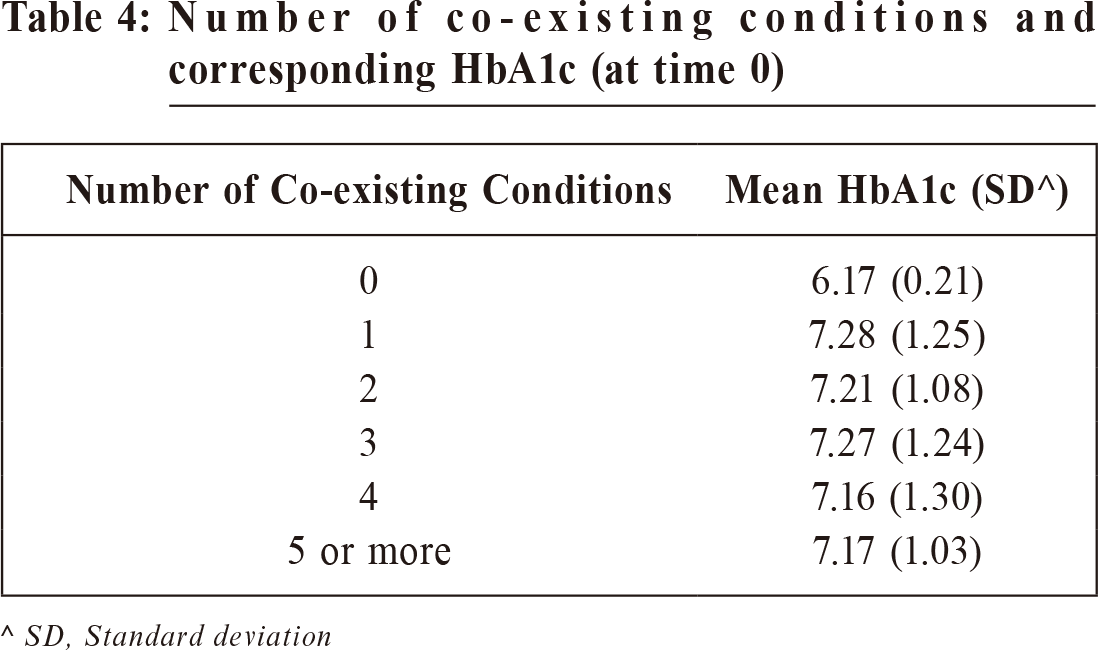
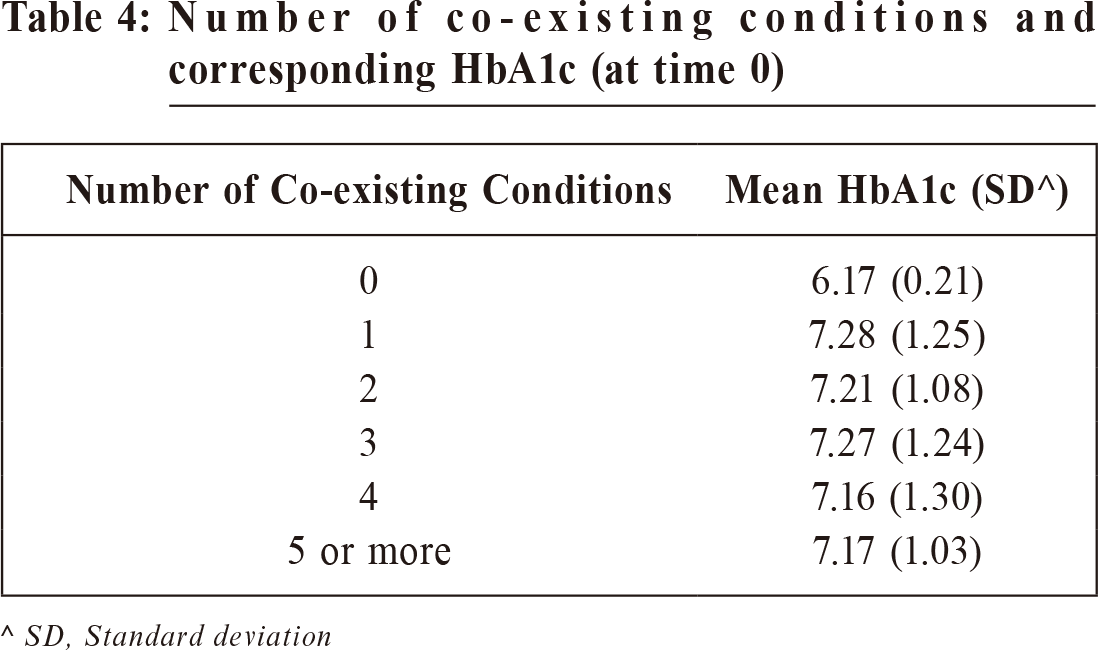
The mean HbA1c levels stratified by different
categories of number of co-existing chronic conditions
among the diabetic patients are shown in Table 4.
Using multiple linear regression adjusted for age, sex,
BMI, smoking status and presence of polypharmacy,
there was no statistically significant association
between the number of co-existing conditions and the
mean HbA1c (p = 0.138).
Association between the number of co - existing
conditions and healthcare utilisation
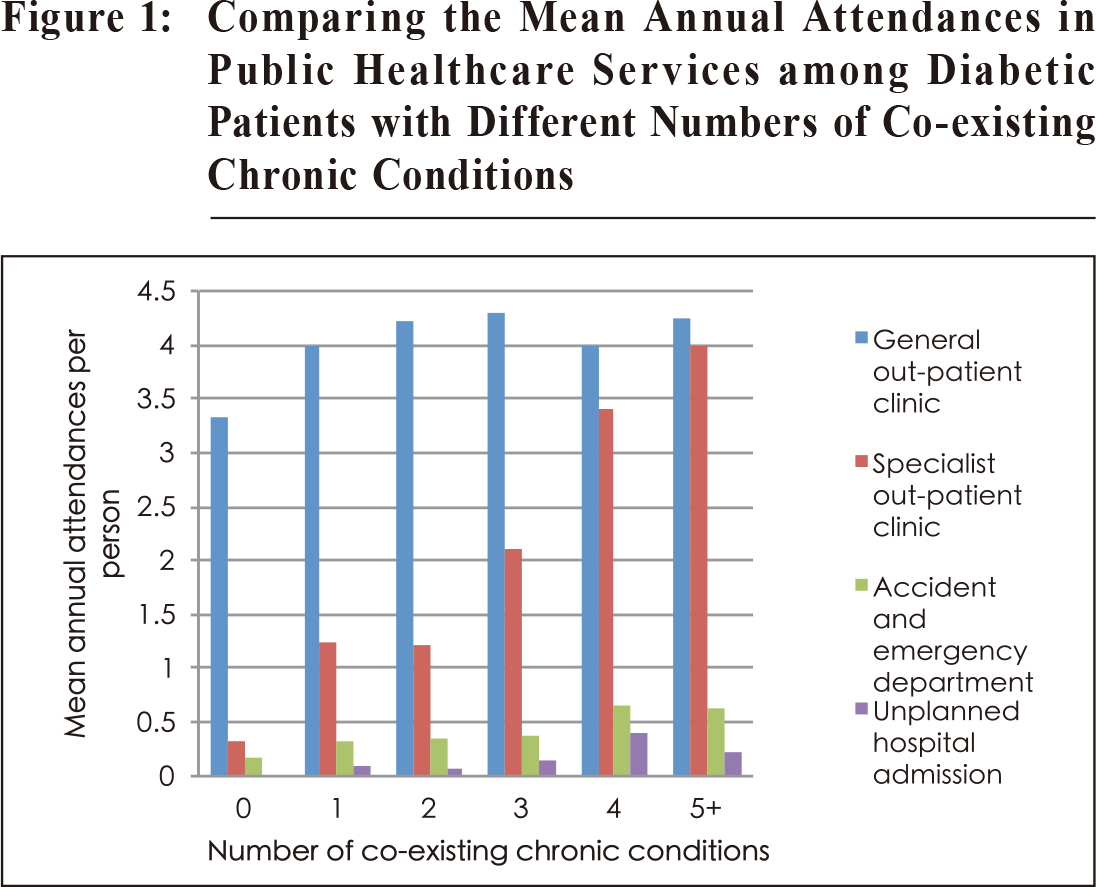
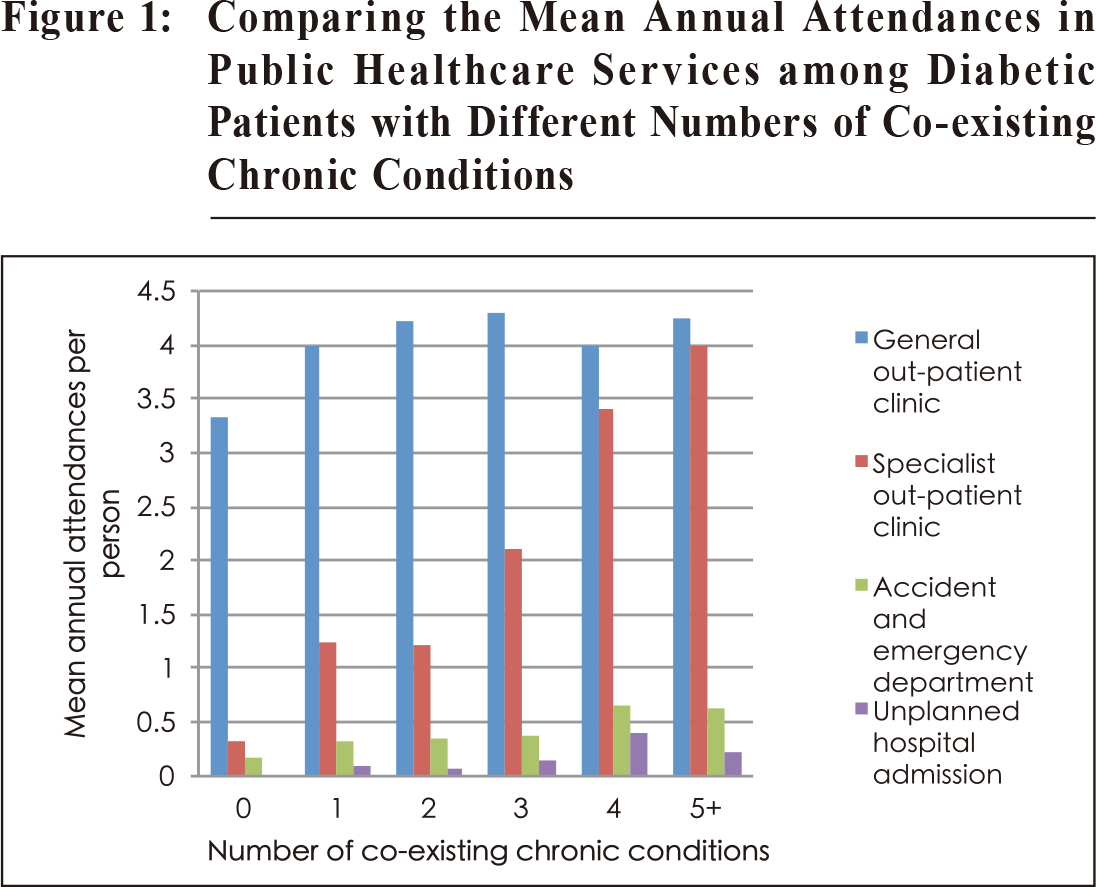
Figure 1 compared the patterns of public
healthcare service utilisation among the subjects with
different numbers of co-existing chronic conditions.
The mean number of annual attendances in the General
Out-patient Clinics, Specialist Out-patient Clinics,
Accident and Emergency Departments and the mean of
annual unplanned hospital admission episodes were 4.18,
2.18, 0.44 and 0.16 per person respectively.
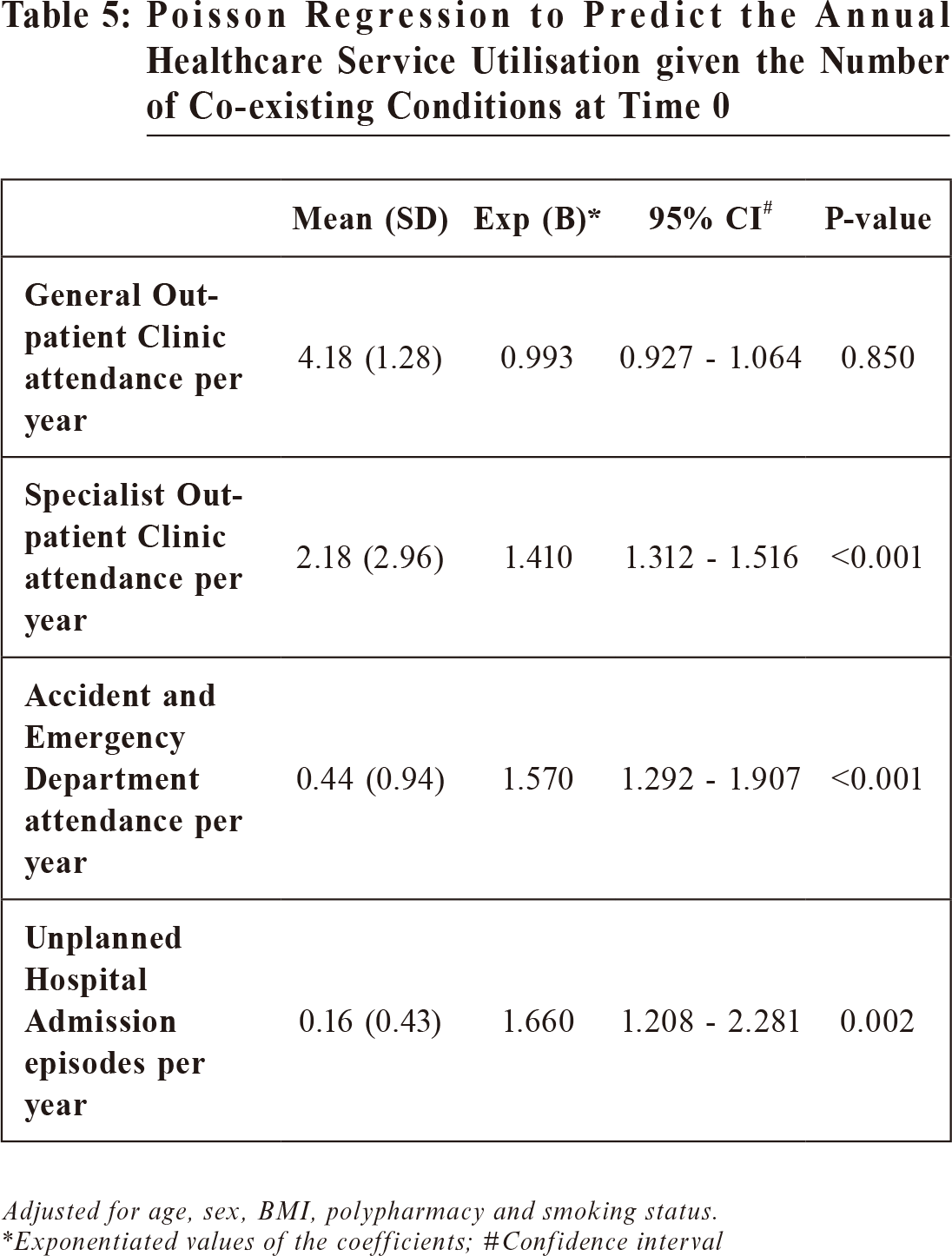
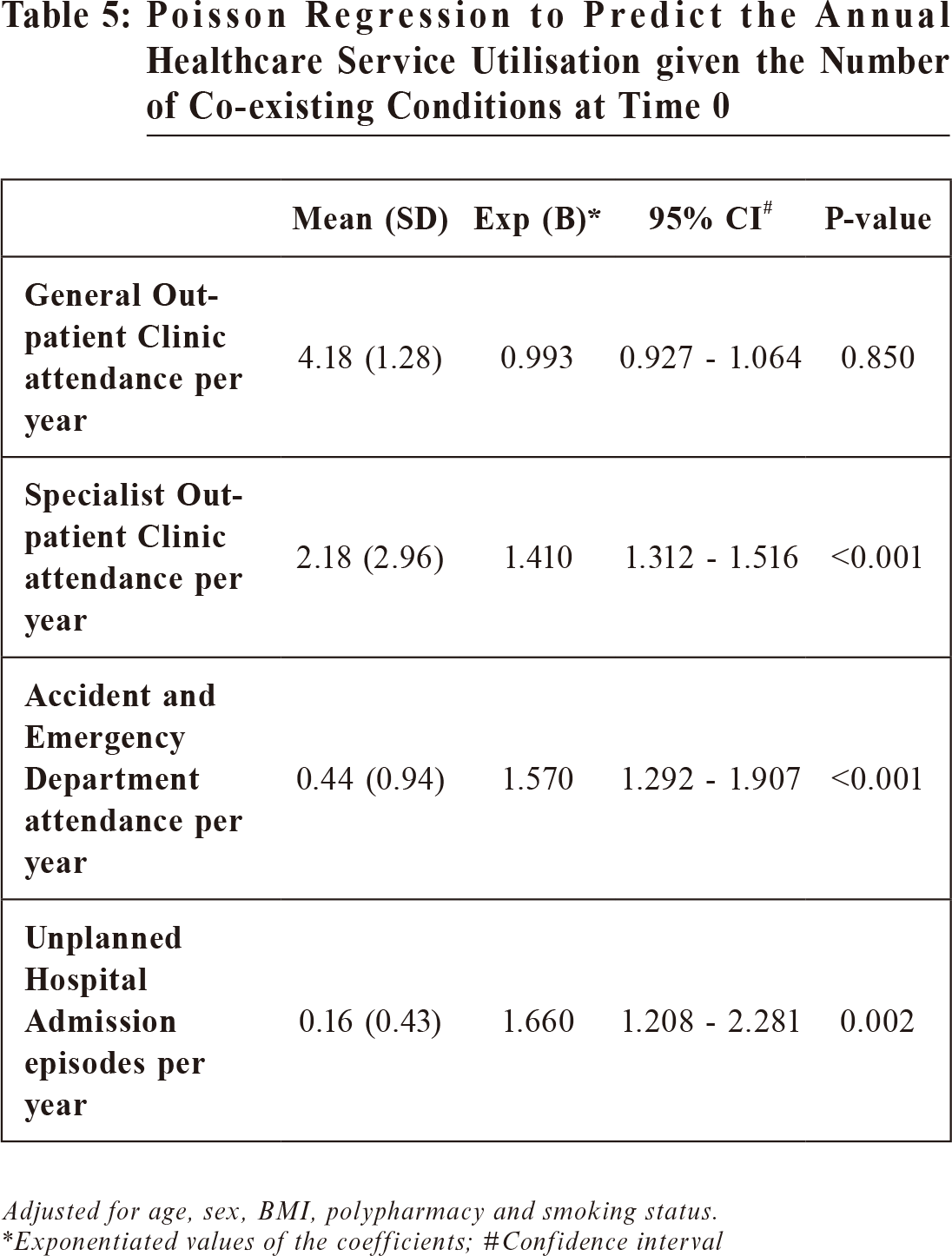
A poisson regression was used to predict the annual
attendances in the public healthcare services based on
the number of co-existing conditions. After adjusting
for age, sex, BMI, smoking status and the presence
of polypharmacy, there were statistically significant
associations between the number of co-existing conditions
and the number of visits to Specialist Out-patient Clinics,
Accident and Emergency Departments, as well as the
number of unplanned hospital admission episodes.
As presented in Table 5, for every extra number of
chronic co-existing condition, 1.41 (95% CI, 1.312-1.516;
p < 0.001) times more Specialist Out-patient Clinic
attendances, 1.57 (95% CI, 1.292-1.907; p < 0.001) times
more Accident and Emergency Department attendances
and 1.66 (95% CI, 1.208-2.281, p < 0.05) times more
unplanned hospital admission episodes were observed in
the following year.
5 patients (1.3%) died within the 2-year reporting
period. The mean age of death was 75 years (range:
65 – 90 years), and all the deceased were non-smoker. They had a mean number
of co-existing
chronic conditions of 4.2 per person and a mean BMI
of 25.9 kg/m².
Discussion
This is the first-ever study evaluating the
magnitude of multi-morbidity and its relationship with
glycaemic control and healthcare service utilisation in
diabetic patients in a Hong Kong Primary Care Outpatient Clinic. We managed to achieve
our primary
objectives by collecting and analysing the data we set
out to achieve at the start of the project.
Similar to the findings reported in studies
conducted on Caucasian subjects4,6-9, the majority of our
study population had multi-morbidities. Hypertension
was observed to be the commonest co-morbid condition.
Almost all (99.2%) of our study cohort had at least
one co-morbid condition. This incidence rate was the
highest among all published in the literatures, and even
higher than that in a similar study which only included
older adults (66 years of age and older) with diabetes
by Gruneir et al.6
Contrary to the first part of our hypothesis, there
was no statistically significant association between the
number of co-morbidities and the glycaemic control (as
measured by HbA1c levels). This is in line with the
finding shown in the study of a cohort of patients with
Type 2 diabetes attending general practice in Ireland by
Teljeur et al.4
This finding could be explained by the
presumption that increasing number of co-morbidities
is associated with increased patient awareness of their
health condition. This might lead to better adherence to
lifestyle measures and drug taking, resulting in better
glycaemic control. As presented in Table 4, patients
with 1 co-existing condition had the highest mean
HbA1c of 7.28%, and other groups had insignificantly
lower HbA1c. A possible explanation is that, with
the comprehensive management programme and the
extensive coverage of diabetes medications in the drug
formulary of General Out-patient Clinics, a mean HbA1c
of less than 7.3% was achieved, regardless of how many
co-existing chronic conditions the patients have.
Other studies classified co-morbid conditions
as diabetes concordant or discordant, depending on
whether they shared the same pathophysiologic risk
profile of diabetes and therefore more likely to be part
of the same management plan.8,10 The study by Magnan
et al10 on 7 health systems in Midwestern US concluded
having more concordant conditions made diabetic care
goal achievement more likely.
We did show a significant positive relationship
between the number of co-existing conditions and
all parameters of healthcare service utilisation in
secondary care. The increasing number of co-morbid
conditions was associated with more attendances
to Specialist Out-patient Clinics and Accident and
Emergency Departments, as well as more unplanned
hospital admission episodes. There was, however, no
association between the number of co-morbidities and
the number of attendances to the General Out-patient
Clinics, and this is in contrast to the result found in
Teljeur et al4, which showed that the general practitioner
visits increased significantly with the increasing
numbers of chronic conditions. Our study findings
could be explained by the distinctive scopes of public
services provided by primary and secondary care in
Hong Kong. While the drug formulary of General Outpatient Clinics of our cluster does
cover the drugs for
most medical conditions, drugs for certain conditions
are only available in secondary care. For example,
anti-psychotic medications for schizophrenia and
disease-modifying anti-rheumatic drugs for rheumatoid
arthritis can only be prescribed in psychiatry clinics
and rheumatology clinics respectively. For a patient
to be transferred from secondary care to primary care,
certain criteria have to be met. In our opinion, this
is beneficial for both the public health care provider
and the population, as this can ensure the patients are
being followed up by the Specialist Out-patient Clinics
if indicated. Furthermore, primary health care will not
be overwhelmed, and its resources can be allocated to
a broad range of services, including health promotion,
prevention of acute and chronic diseases, health risk
assessment, self-management support and adjusting
its services in unforeseen circumstances such as
pandemics.
Other studies had shown that utilisation across all
health services increased with the number of comorbid
conditions.6,7 This could be explained by the different
structures of healthcare systems in different countries.
It is of interest to note that 3 out of the 5 deceased
subjects had cancers of the gastro-intestinal system
diagnosed within the reporting period. The causes of
the 3 deaths were metastatic rectal cancer, metastatic
pancreatic cancer and metastatic sigmoid cancer. In
recent years, there had been emerging evidences
showing the link between Type 2 diabetes and increased
risk for cancer of gastro-intestinal tract.17-19
Strengths and limitations
Firstly, the major strength was that we did not
rely solely on the preliminary data drawn from the
computerised system of electronic record (CDARS).
Instead, the investigators reviewed each record
individually. This significantly minimised the potential
for misclassification and / or underestimation of chronic
conditions. Although reporting of discrepancies
between the actual health conditions of the patients
and the information in the records was outside the
scope of our objectives, it is worth pointing out that the
investigators frequently identified chronic conditions
which were not coded appropriately in the patient
records, and these discrepancies would hence not have
been identified via CDARS. Secondly, compared to
similar researches conducted with Caucasian subjects,
our study was unique as we considered polypharmacy
as a potentially important confounding factor. In
addition to the patient demographic characteristics, we
adjusted the analyses for the presence of polypharmacy.
Thirdly, although our list of chronic conditions was
not exhaustive, we included a comprehensive set of 28
conditions.
However, several limitations should be mentioned.
Firstly, this was a cross-sectional study, hence, we
could only assess the associations of multi-morbidity
with glycaemic control and healthcare service
utilisation. We could not draw definite cause and
effect relationships between our outcome measure
parameters. Secondly, although the Electronic Health
Record Sharing System (eHRSS) launched by Hong
Kong Government in 2016 allows sharing of patient
medical records between the public and private
healthcare sectors, participation in the eHRSS is not
mandatory for both healthcare providers and patients.
Consequently, there is the potential for missing data
should the patients attend both public and private
sectors for medical consultations. Thirdly, this study
was conducted in a single General Out-patient Clinic,
generalisability of results hence could not be concluded
from it. Fourthly, this study only analysed the public
healthcare service utilisation by the number of visits
for medical consultation and unplanned hospital
admission episodes, and the actual public healthcare
service utilisation should also include other parameters
such as nursing and allied health service, duration of
hospital admissions, prescriptions as well as diagnostic
investigations. Lastly, HbA1c was the only diabetes
care goal that we included in our study, while actual
management of diabetic patents is more complex, which
entails other key indices including blood pressure, lipid
profile, presence and degree of retinopathy, and others.
Implications and future research
This study evaluated the extent of multi-morbidity
among diabetic patients attending a General Out-patient
Clinic in Hong Kong, and the majority of these patients
were Chinese. The result of this study should be useful
in developing diabetic care guidelines and intervention
in Primary Care Service in Hong Kong.
It is more often the case that a diabetic patient
suffers from other co-morbid conditions, and this result
underscores the importance of knowing the multimorbidity pattern in patients with Type 2
diabetes, and
the need for a multidisciplinary approach to address
their complex health care needs and ensure optimisation
of their medical treatment.
This study tested the feasibility and identified
challenges of such potential research work being
conducted within the Hong Kong public healthcare
setting. One challenge as already mentioned is that,
despite the launching of eHRSS, there is still limitation
of medical information sharing between the public and
private healthcare providers. This consequently creates
a major obstacle, should anyone wish to perform an
epidemiological study on multi-morbidity in Hong
Kong. Another limitation is the accuracy of medical
record as the documentation and coding may vary
among clinicians.
Using a single-disease framework to set
management guideline for chronic diseases, such as
diabetes, is rather out-dated. There is a need for
further researches to examine the impact of multimorbidity on the achievement of
diabetic care goals and
the degree of healthcare service utilisation, which in
turn will be useful for strategic resource planning and
education.
We were aware that analysing the degree of multimorbidity by the total number of
comorbid conditions
would not give an account of the nature of the co-existing diseases. The majority of
diabetic patients have
2 to 3 other co-existing conditions. Therefore, future
multi-morbidity researches exploring commonly co-occurring disease combinations, are
likely to provide
more meaningful insights into the complex care needs
of individuals with multiple chronic conditions.
Conclusion
Our study has illustrated again the fact that
diabetes rarely occurs as a single chronic condition.
The occurrence of multi-morbidity is common in
Type 2 diabetic patients who are under the care of
public primary care out-patient clinic in Hong Kong.
Accordingly, it is imperative to use a multi-morbidity
framework, not only to deliver a comprehensive patient-centred programme, but also to
optimise diabetic care
in order to reduce treatment burden and unplanned care.
Acknowledgement
We acknowledged the support from the research
team of the Department of Family Medicine and
Primary Health Care, New Territories West Cluster, the
Hospital Authority of Hong Kong.
This study was approved by the Cluster Research
Ethics Committee of New Territories West Cluster, the
Hospital Authority of Hong Kong.
We do not have any conflict of interest to declare.
Cheuk-chung Sung,
MBChB (Leeds), MRCSEd, MRCGP, FHKAM (Family Medicine)
Associate Consultant,
Department of Family Medicine and Primary Health Care, New Territories West
Cluster, Hospital Authority
Tsun-kit Chu,
MBBS (HK), MSc, FHKCFP, FRACGP, FHKAM (Family Medicine)
Associate Consultant,
Department of Family Medicine and Primary Health Care, New Territories West
Cluster, Hospital Authority
Jun Liang,
MBChB (Glasg), MRCGP, FHKAM (Family Medicine)
Chief of Service,
Department of Family Medicine and Primary Health Care, New Territories West
Cluster, Hospital Authority
Correspondence to:
Dr Cheuk-chung Sung, Associate Consultant, Department of
Family Medicine and Primary Health Care, New Territories West
Cluster, Hospital Authority, Hong Kong SAR.
E-mail: ccsung@doctors.org.uk
References:
-
Quan J, Li TK, Pang H, et al. Diabetes incidence and prevalence in Hong
Kong, China during 2006-2014. Diabet Med. 2017 Jul;34(7):902-908. doi:
10.1111/dme.13284. [Epub 2016 Nov 29.
-
Multimorbidity: technical series on safer primary care. World Health
Organization 2016. Available from: apps.who.int
-
Chu TK, Lau P, Cheng SYC, et al. A study on the prevalence of multimorbidities
of diseases and utilization of public healthcare services in the
New Territories West area of Hong Kong. HK Pract. 2018;40:43-50.
-
Teljeur C, Smith SM, Paul G, et al. Multimorbidity in a cohort of patients
with type 2 diabetes. Eur J Gen Pract. 2013 Mar;19(1):17-22. doi:10.3109/1
3814788.2012.714768.
-
Magnan EM, Palta M, Mahoney JE, et al. The relationship of individual
comorbid chronic conditions to diabetes care quality. BMJ Open Diabetes
Res Care. 2015 Jul 23;3(1):e000080. doi: 10.1136/bmjdrc-2015-000080.
eCollection 2015.
-
Gruneir A, Markle-Reid M, Fisher K, et al. Comorbidity burden and
health services uses in community-living older adults with diabetes
mellitus: a retrospective cohort study. Can J Diabetes. 2016 Feb;40(1):35-
42. doi: 10.1016/j.jcjd.2015.09.002. [Epub 2016 Jan 6.]
-
Fisher K, Griffith L, Gruneir A, et al. Comorbidity and its relationship with
health service use and cost in community-living older adults with diabetes: a
population-based study in Ontario, Canada.
Diabetes Res Clin Pract. 2016
Dec;122:113-123. doi:10.1016/j.diabres.2016.10.009. [Epub 2016 Oct 20.]
-
Ricci-Cabello I, Stevens S, Kontopantelis E, et al. Impact of the prevalence
of concordant and discordant conditions on the quality of diabetes care in
family practices in England. Ann Fam Med. 2015 Nov;13(6):514-522. doi:
10.1370/afm.1848
-
Calderón-Lar rañaga A, Abad-Díez J M, Gimeno-Feliu LA, et al.
Global health care use by patients with type-2 diabetes: Does the type
of comorbidity matter? Eur J Intern Med. 2015 Apr;26(3):203-210.
doi:10.1016/j.ejim.2015.02.011. [Epub 2015 Mar 10.]
-
Magnan EM, Palta M, Johnson HM, et al. The impact of a patient's
concordant and discordant chronic conditions on diabetes care quality
measures. J Diabetes Complications. 2015 Mar;29(2):288-294. doi:10.1016/
j.jdiacomp.2014.10.003. [Epub 2014 Oct 13.]
-
Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of
adverse drug events among older persons in the ambulatory setting. Jama.
2003 Mar 5;289(9):1107-1116.
-
Pérez T, Moriarty F, Wallace E, et al. Prevalence of potentially inappropriate
prescribing in older people in primary care and its association with hospital
admission: longitudinal study. BMJ. 2018 Nov 14:363.
-
Statistics & Workforce Planning Department, Strategy & Planning
Division, Hospital Authority Head Office, Hospital Authority. Primary
care services portfolio 2016-2017.
-
Charan J, Biswas T. How to calculate sample size for different study
designs in medical research? Indian J Psychol Med. 2013 Apr; 35(2):121-
126. doi: 10.4103/0253-7176.116232. PMID: 24049221.
-
Subramaniam M, Abdin E, Vaingankar JA, et al. Impact of psychiatric
disorders and chronic physical conditions on health-related quality of life:
Singapore Mental Health Study. J Affect Disord. 2013 May;147(1-3):325-
330. doi: 10.1016/j.jad.2012.11.033. [Epub 2012 Dec 20.]
-
Masnoon N, Shakib S, Kalisch-Ellett L, et al. What is polypharmacy? A
systematic review of definitions. BMC Geriatr. 2017;17:230. Published
online 2017 Oct 10. doi: 10.1186/s12877-017-0621-2.
-
González N, Prieto I, Del Puerto-Nevado L, et al. 2017 update on the
relationship between diabetes and colorectal cancer: epidemiology,
potential molecular mechanisms and therapeutic implications. Oncotarget.
2017;8(11):18456-18485.
-
Miao ZF, Xu H, Xu YY, et al. Diabetes mellitus and the risk of gastric cancer:
a meta-analysis of cohort studies. Oncotarget. 2017;8(27):44881-44892.
-
Andersen DK, Korc M, Petersen GM, et al. Diabetes, Pancreatogenic
Diabetes, and Pancreatic Cancer. Diabetes. 2017;66(5):1103-1110.
|