|
December 2020,Volume 42, No.4
|
Update Article
|
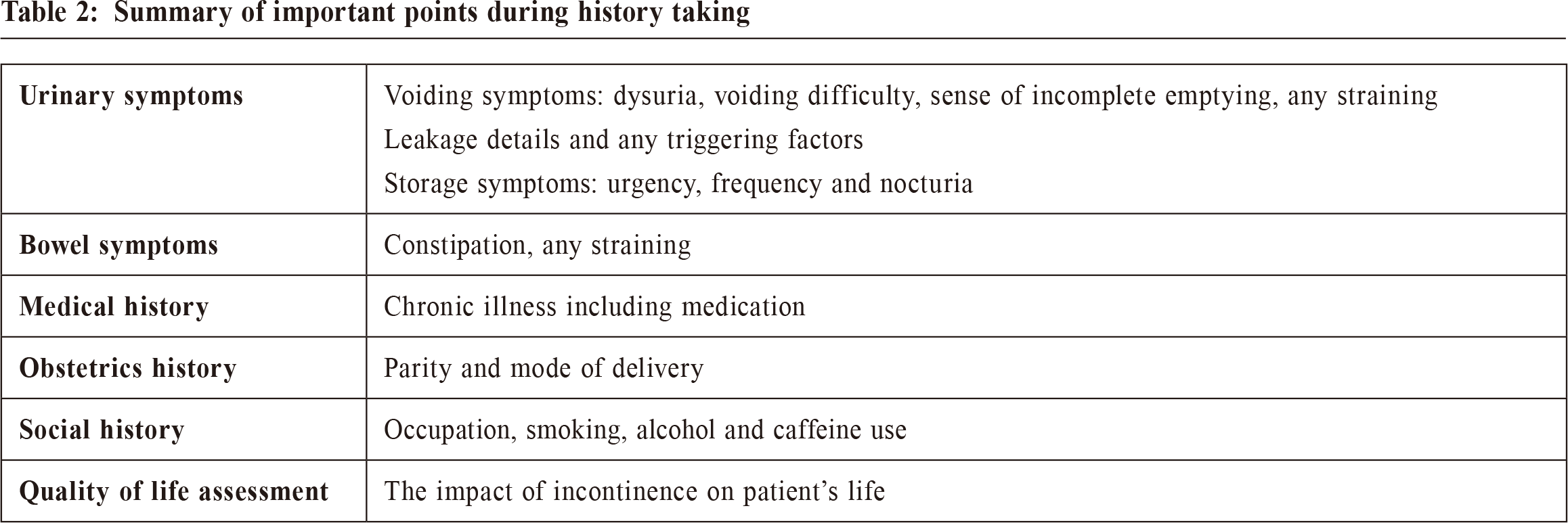
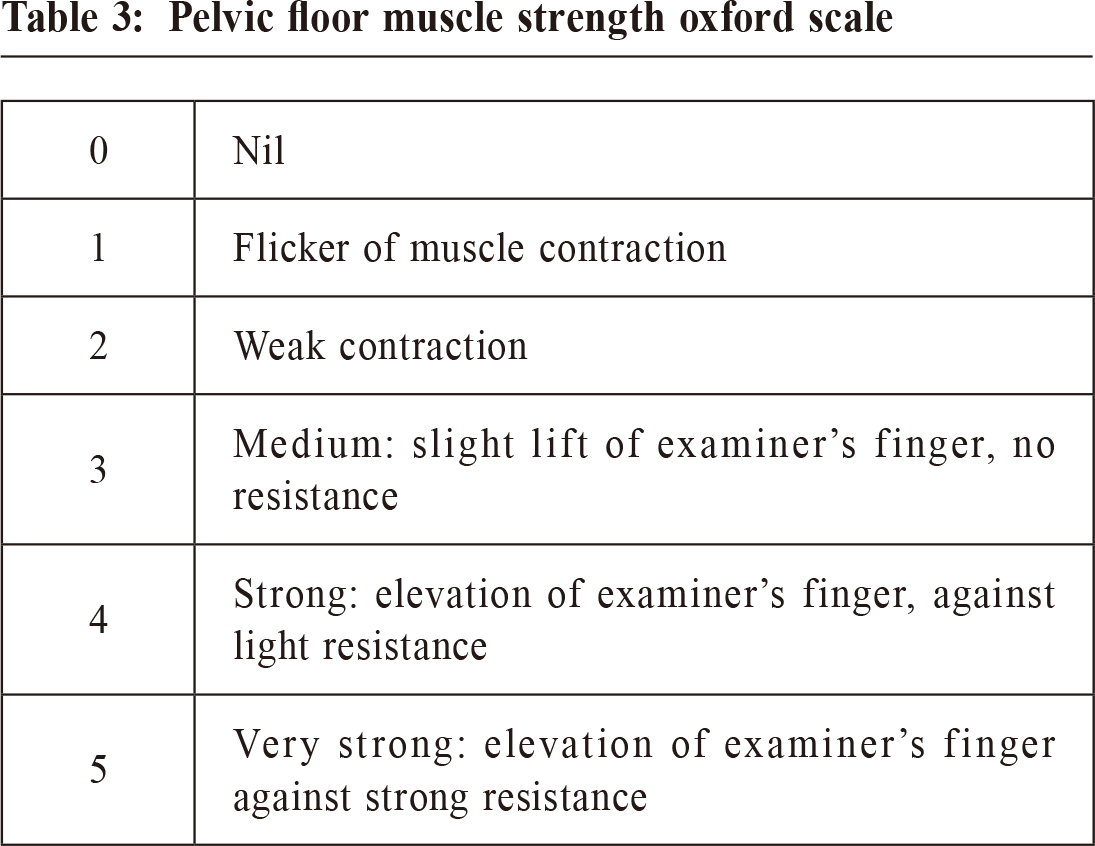
Management of female urinary incontinenceMandy CH Yu 于春紅 HK Pract 2020;42:99-104 SummaryUrinary incontinence is a common problem but often been dismissed as being normal and neglected. According to a local telephone survey performed in 2005 which included 540 women aged 17-77, over 75% of the respondents reported having some kinds of urinary incontinence.1 The prevalence of urinary incontinence is believed to be even higher now, with an aging population. 摘要尿失禁是一個普遍的問題, 但始終被忽略。 根據2005年進行的一項本地電話調查, 其中包括540位17 - 77歲的女性, 超過75%的受訪者報告患有某種尿失禁。1 隨著人口老齡化,相信現在尿失禁的患病率甚至會更高。 IntroductionIn dealing with urinary incontinence, we should try to categorise the woman’s urinary incontinence, and treatment can then get started accordingly. In managing mixed incontinence, we should direct treatment towards the predominant symptoms. Types of urinary incontinence2Stress urinary incontinenceInvoluntary leakage of urine on effort or exertion, or on sneezing or coughing Urge incontinenceInvoluntary leakage of urine associated with urgency Mixed incontinenceInvoluntary leakage of urine associated with urgency as well as exertion, effort, sneezing or coughing Overflow incontinenceInvoluntary leakage of urine associated with poor bladder emptying Nocturnal enuresisInvoluntary urination that happens at night while sleeping History takingBesides the basic questions about the patient’s background, we will ask for relevant questions like duration of symptoms, severity of incontinence, any triggering factors like coughing, sneezing, change of position during history taking. We would also assess any overactive bladder symptoms like urgency, frequency, prolapse symptoms, bowel symptoms, coital incontinence and voiding problems. Patient’s past medical, surgical and medication history is also important since some medical conditions like asthma or some medications can be precipitating factors for urinary incontinence. Table 1 showed medications that might exacerbate urinary symptoms. We should also try to understand patent’s lifestyle which may help to give modification advice for the incontinence problem (Table 4). Conservative management always comes first before any medication or surgery. If the patient is young, her fertility wish has to be taken into consideration as this may affect the management option. During physical examination, we aim to rule out any pelvic mass, check for any genital prolapse and also assess the strength of pelvic floor during vaginal examination according to the oxford scale. (Table 3) 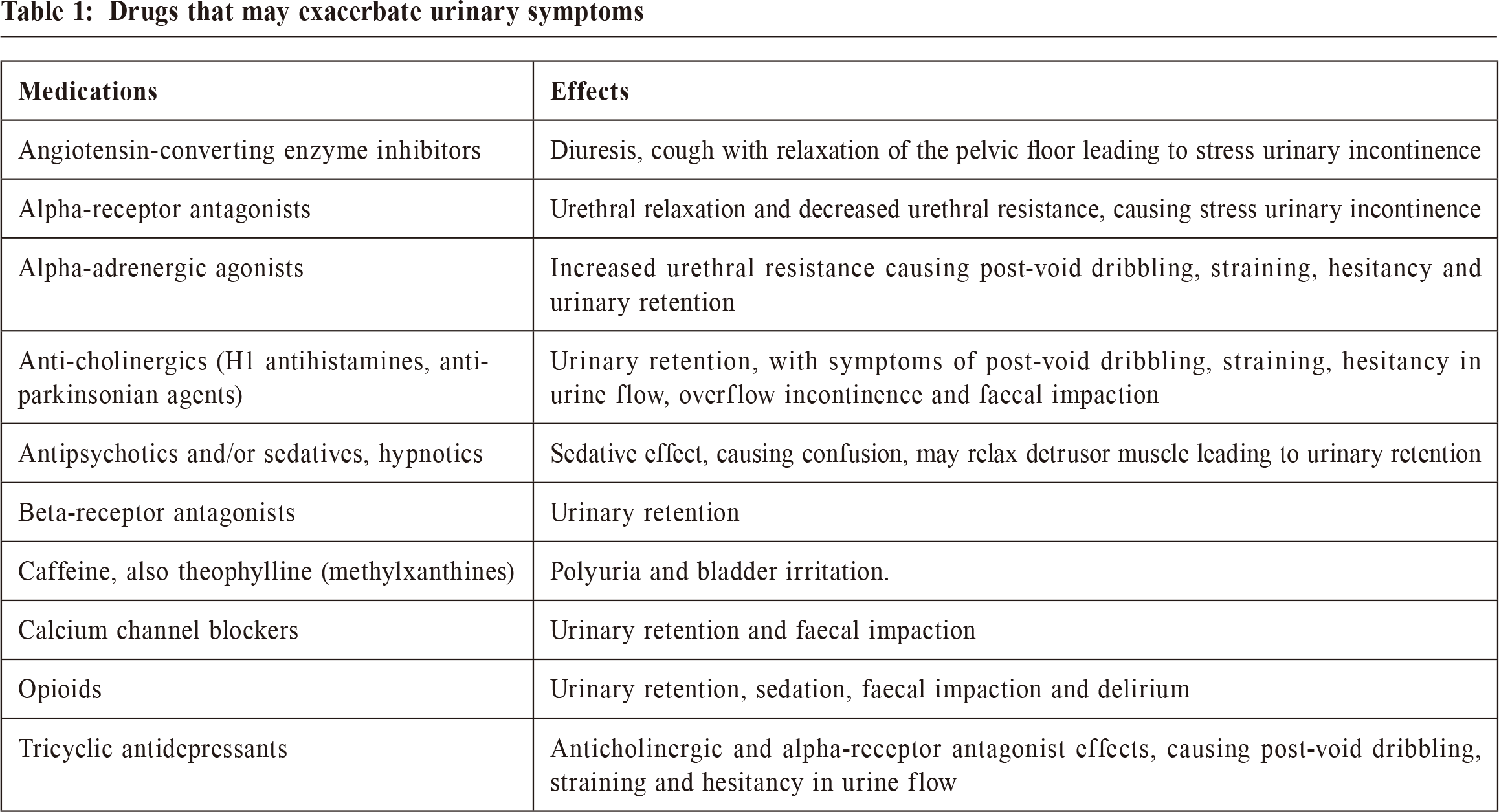
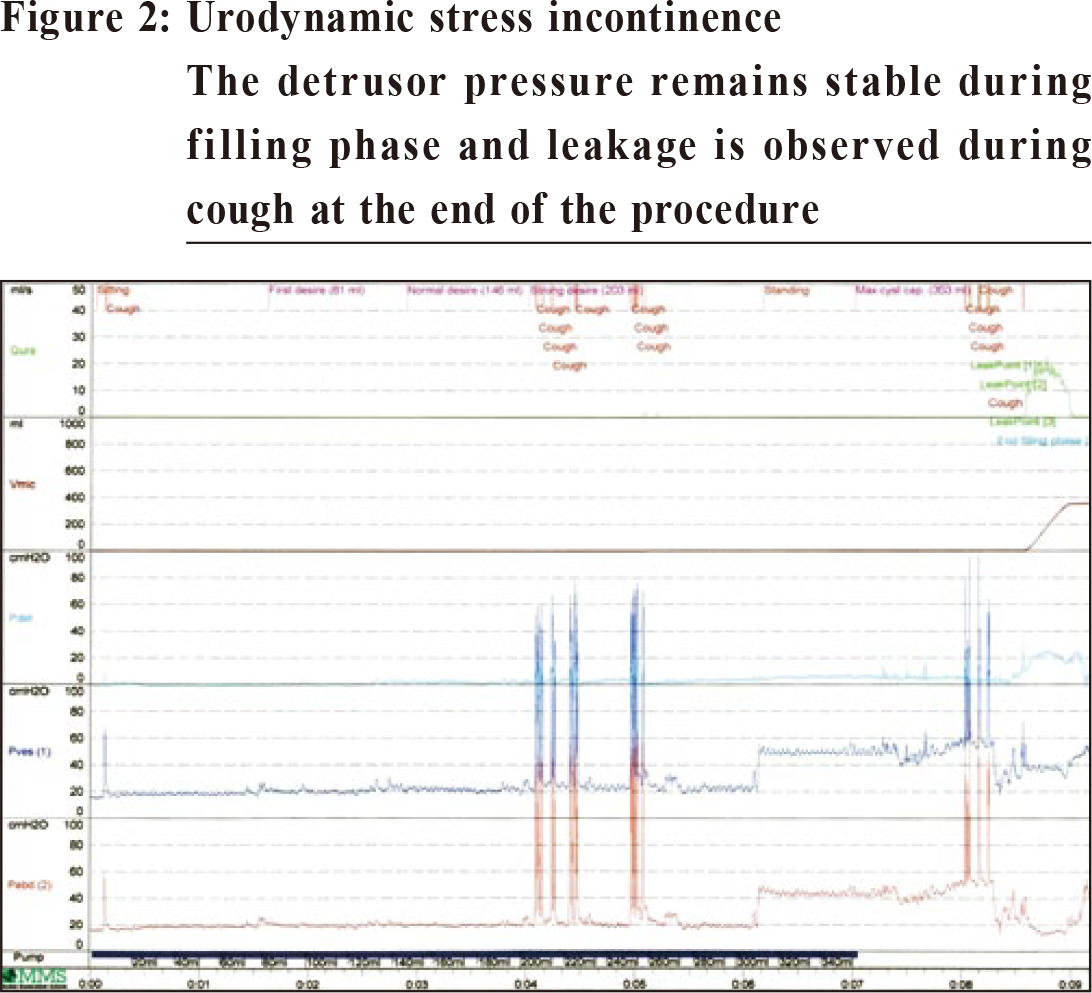
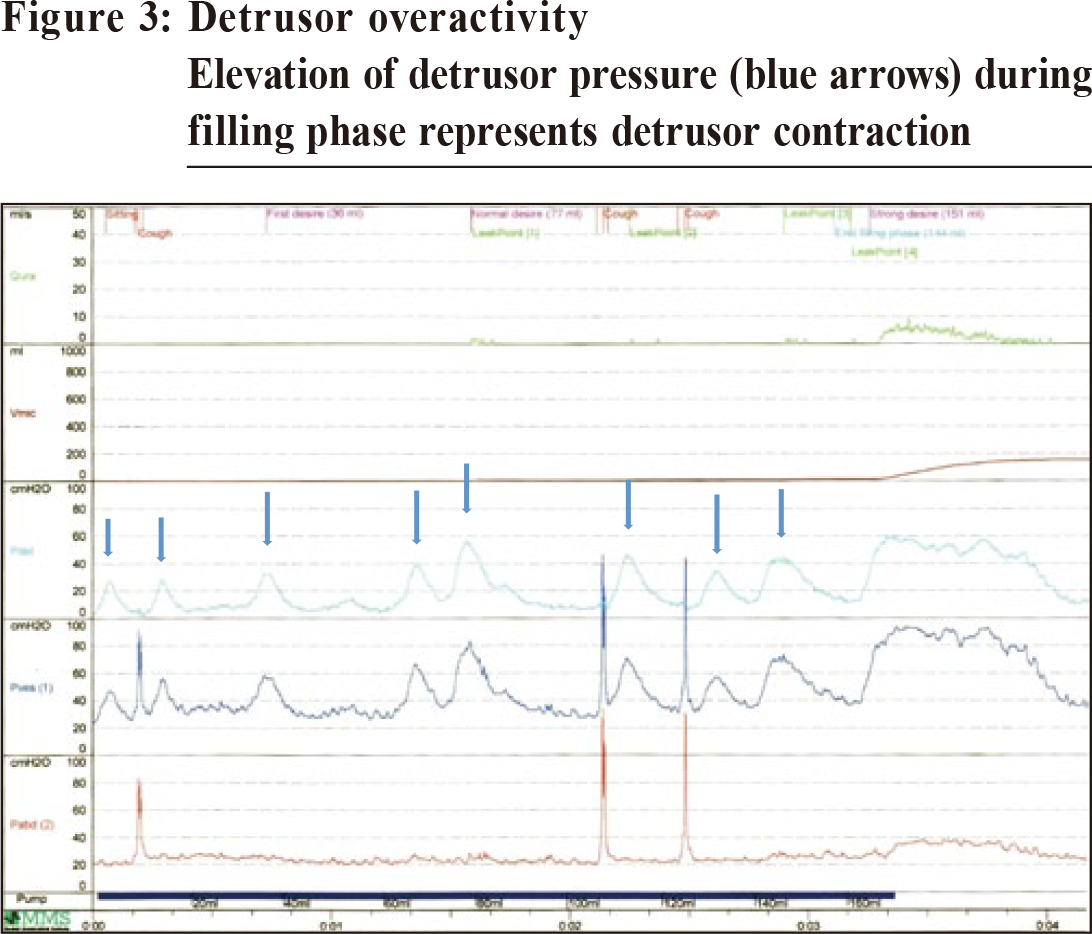
InvestigationsRenal function test and fasting blood glucose:Not a routine unless there is concern of severe urinary retention causing hydronephrosis or clinical suspicion of diabetics. Urinalysis:To rule out infection Bladder diary:Fluid intake, voiding time and quantities and episodes of urinary incontinence are recorded over a minimum of three days covering variations in their usual activities, such as both working and leisure days. Urodynamics:Recommended in patient with urinary incontinence in which the type is unclear; urge-predominant mixed incontinence; symptoms suggestive of voiding dysfunction; before stress incontinence surgery for patients with anterior or apical prolapse or patient required second incontinence surgery. UrodynamicsFigures 1 and 2 show the urodynamic pressure-flow study of a patient with stress incontinence and detrusor overactivity respectively. 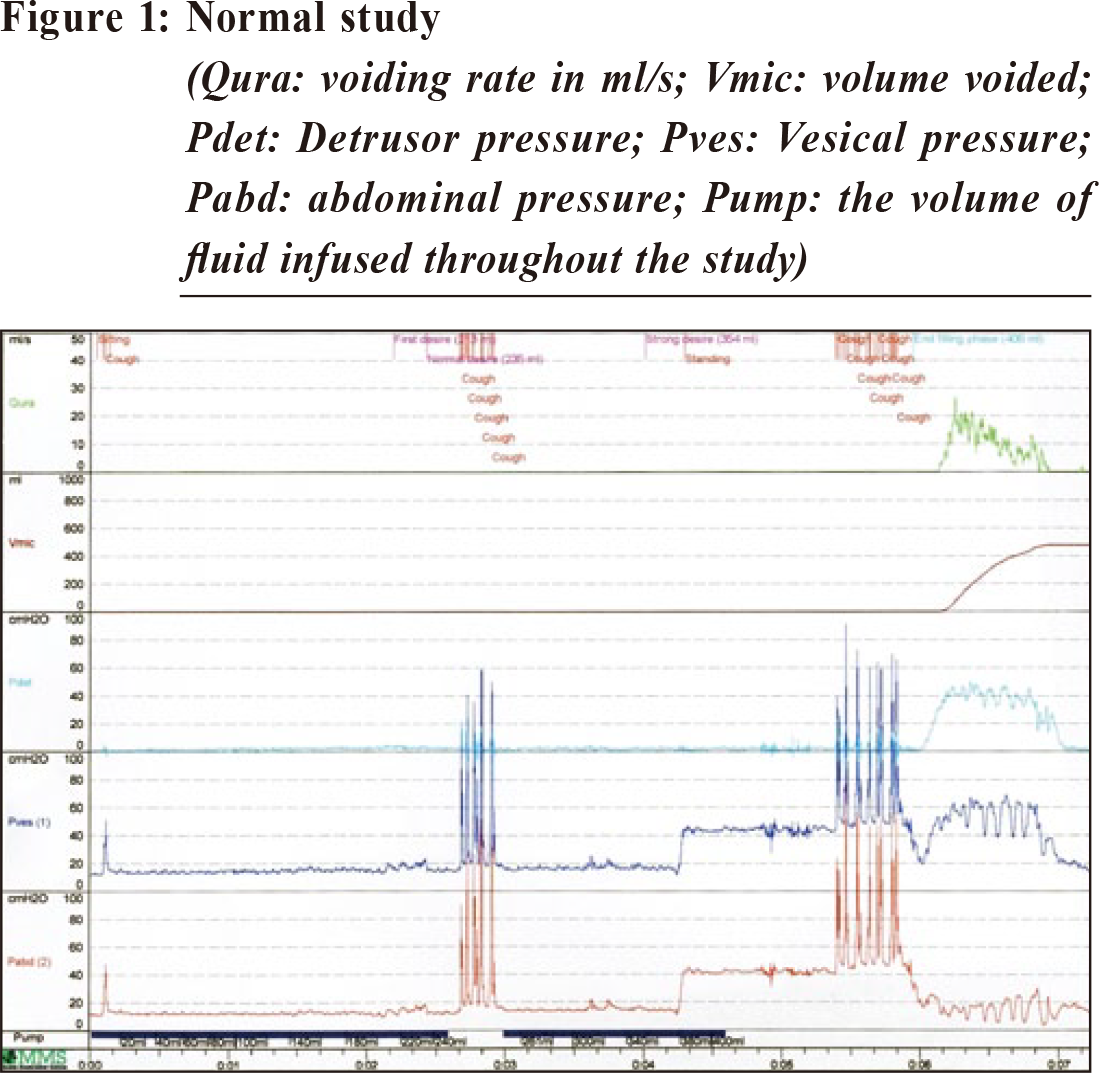
Conservative management for urinary incontinenceLifestyle modifications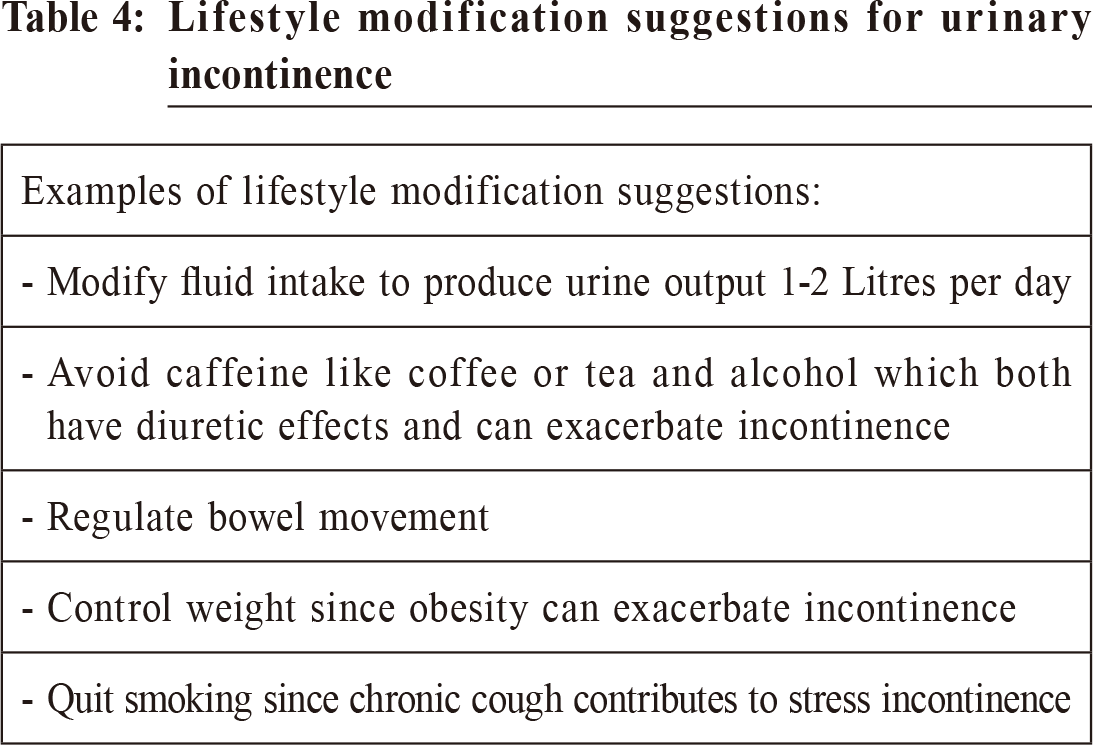
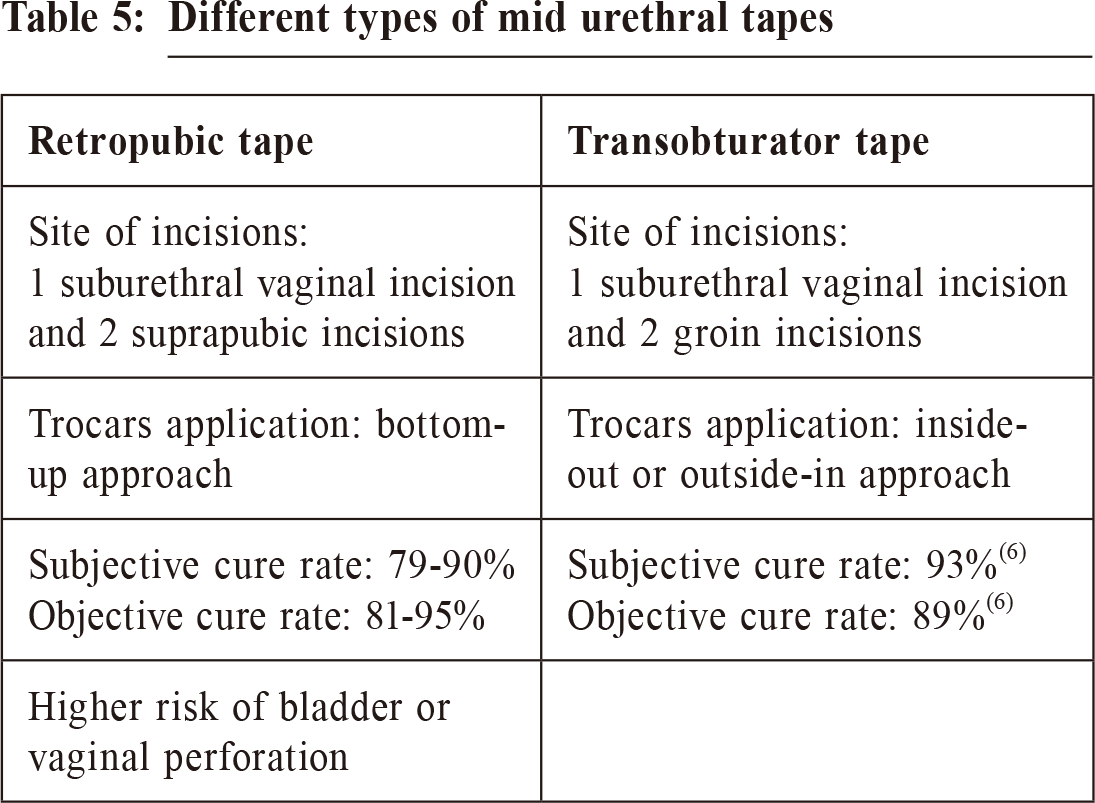
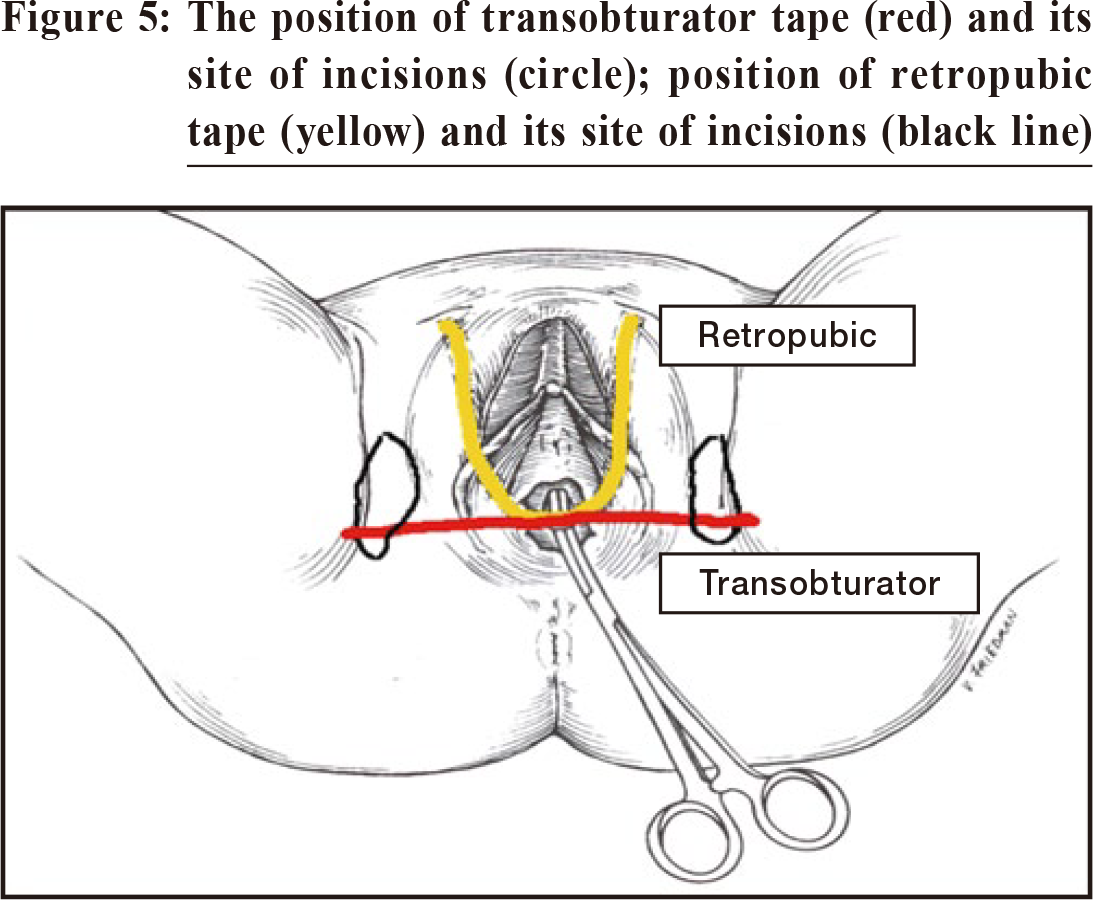
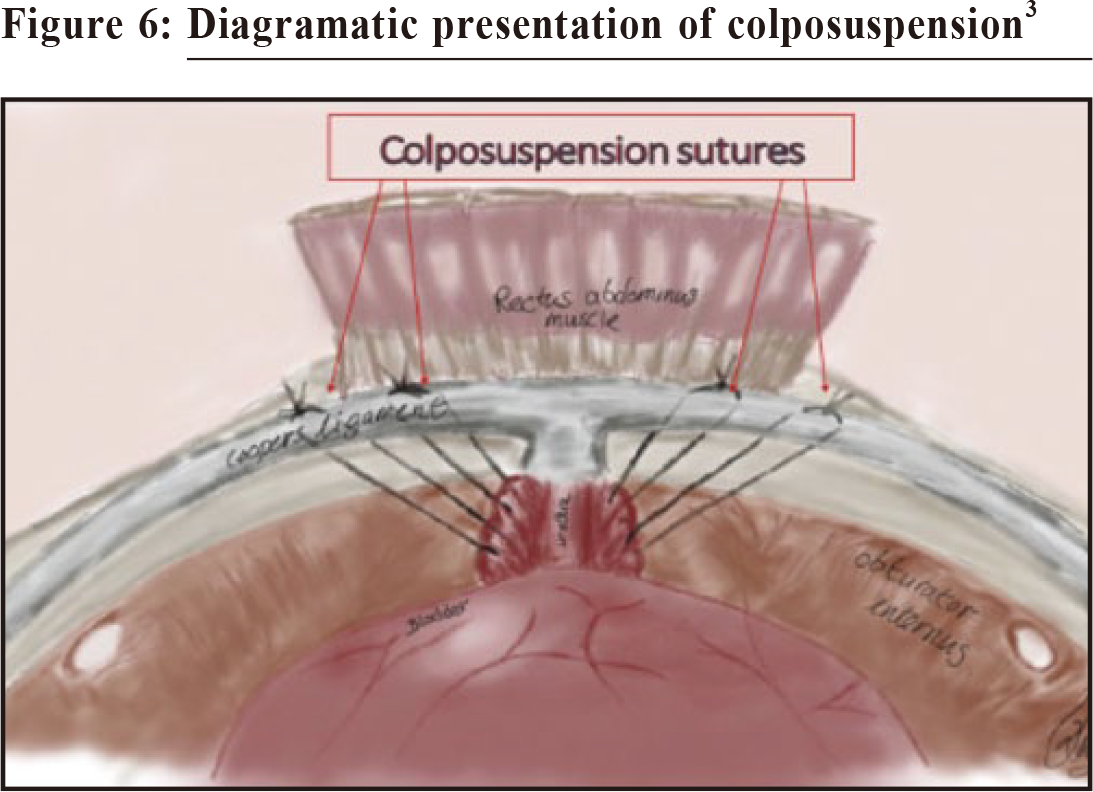
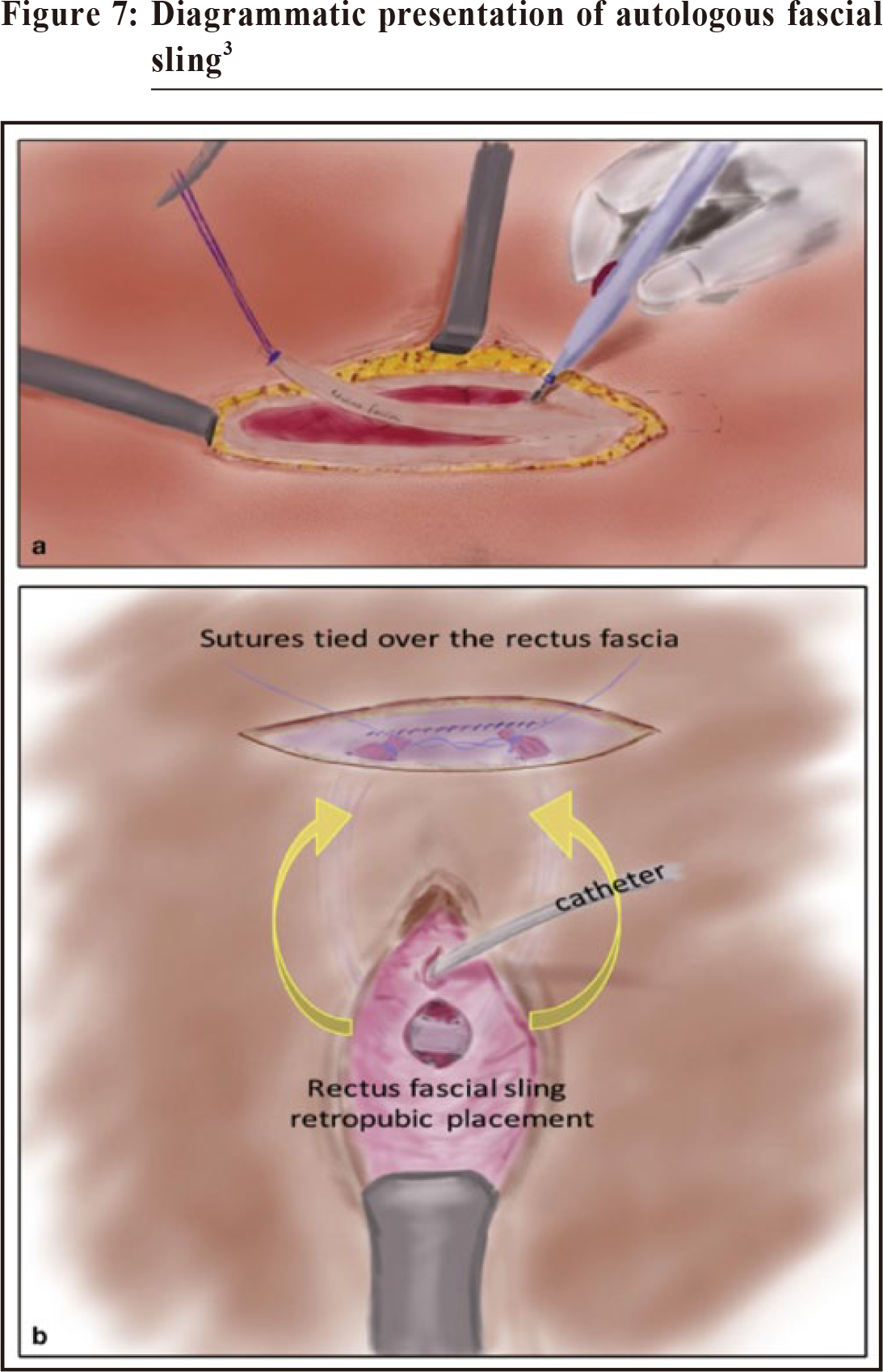
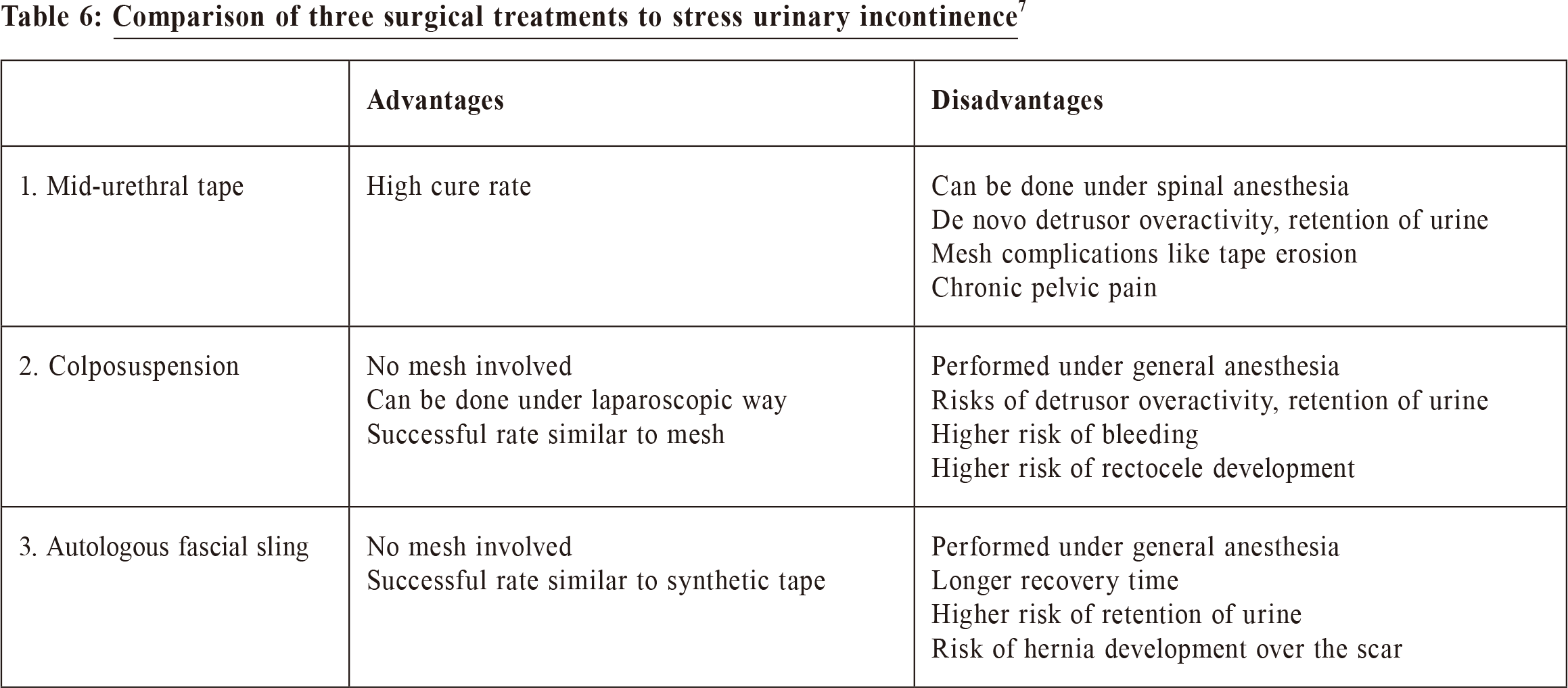
Pelvic floor exercise‘Squeeze and hold’ exercise is recommended. NICE guidelines recommend pelvic floor exercise consisting of at least 8 contractions 3 times per day for a minimum of 3 months, as a first line treatment for urinary incontinence. Electrical stimulation or biofeedback can be considered in women who cannot actively contract pelvic floor muscles in order to improve their compliance. Surgical and medical treatments3,4NICE guidelines5 recommend three types of surgical procedures for stress urinary incontinence:
Medical treatment for urge incontinence8,9Traditionally anticholinergic therapy is used for treatment of urge incontinence. It works by blocking the smooth muscle receptors in bladder and hence inhibiting the involuntary bladder contraction. Common side effects include dry mouth and constipation. Due to the presence of muscarinic receptors in the hippocampus and forebrain, this type of treatment may also affect the memory and cognition of the patients. Because the unknown long term effects of anticholinergic medicines, NICE guidelines state that oxybutynin, an anti-muscarinic, is contraindicated in frail elderly and full discussion with the women about the potential long term impact of anticholinergics is recommended before prescribing the drugs. Another group of drugs is Beta-3 agonists, Mirabegron (e.g. Betmiga), which use the sympathetic nerve pathway to stimulate beta-3 receptors in the bladder, causing smooth muscle relaxation. Since it does not block the muscarinic receptors, the risk of urinary retention and anticholinergic side effects is less. The main contraindication is uncontrolled hypertension. Care should be taken if patient is on digoxin. Before you start a drug, you should review the patient’s clinical condition e.g. poor bladder emptying and her present medications, counsel her on possible side effects and start with the lowest recommended dose. If the drug is effective and well-tolerated, do not change the dose or drug. 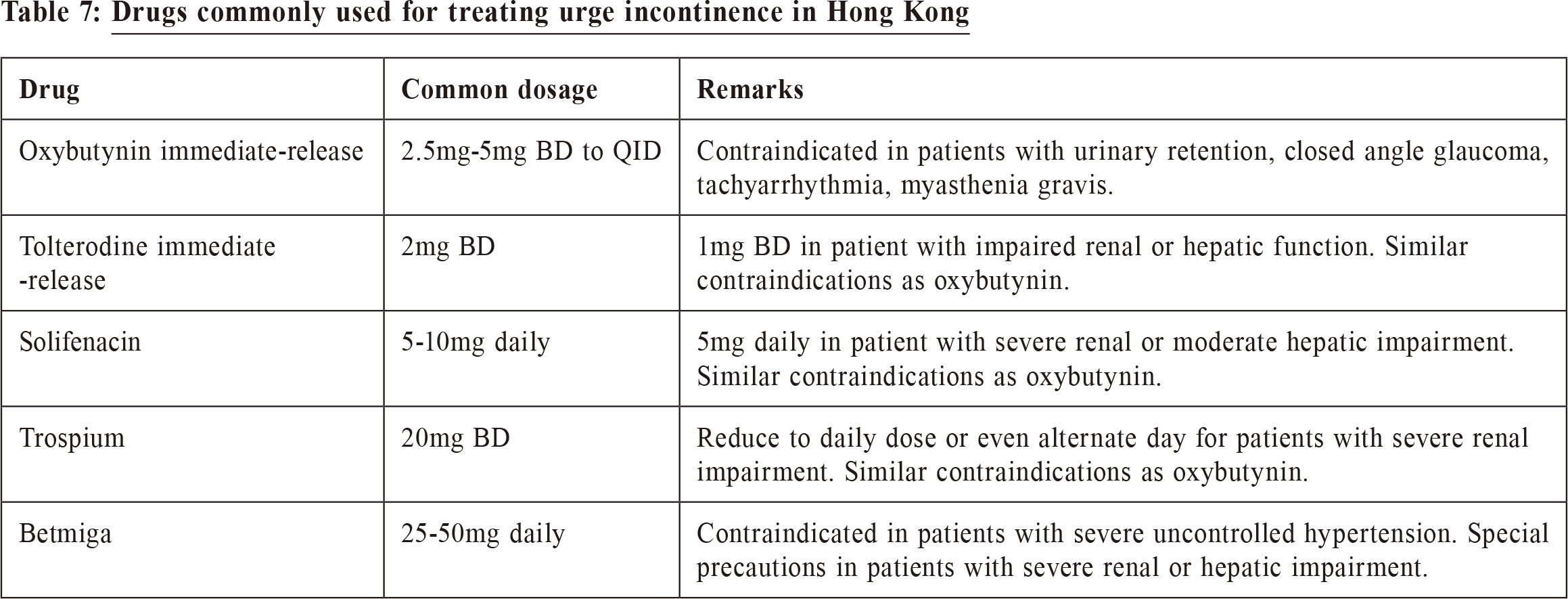
ConclusionUrinary incontinence is a common condition that women choose to accept the symptoms rather than actively seek treatment because they think it is a normal part of aging. We should try to correct this concept, and improve the quality of life of these patients.
Mandy CH Yu, MBChB(CUHK), MRCOG(UK), FHKAM(O&G), Cert HKCOG(Urogynaecology)
Correspondence to: Dr Mandy CH Yu, Department of Obstetrics and Gynaecology,
United Christian Hospital, 130 Hip Wo Street, Kwun Tong,
Hong Kong SAR.
References:
|
|