Barriers to exercise participation among
older Chinese adults attending a primary
care clinic in Hong Kong
Olivia B Y Choi 蔡寶瑜,David K K Wong 王家祺,Man-kuen Cheung 張文娟
HK Pract 2021;43:21-32
Summary
Objective:
To explore the level of physical activity (PA)
and the barriers to exercise participation among the
older adults attending a university primary care clinic in
Hong Kong.
Design:
Cross-sectional questionnaire survey
Subjects:
Patients aged 60 or above attending a
university primary care clinic in Hong Kong
Main outcome measures:
Level of PA as measured
by the validated short version of International Physical
Activity Questionnaire (IPAQ), self-perceived internal
and external barriers to PA
Results:
Overall, 20% (47/235) of respondents had low
level of PA. The three most common internal barriers to
PA were found to be: “too tired” (59%, 139/235), “too
lazy” (52%, 122/235), and “medical problem” (47%,
111/235). The most common external barriers were:
“bad weather” (49%, 116/235), “lack of time” (37%,
87/235), and “no one to exercise with” (28%, 65/235)
Conclusions:
The study has identified the most
common barriers to exercise participation among the
older adults attending a university primary care clinic.
Healthcare providers can address these barriers and
develop strategies for the implementation of exercise
programmes in coming years.
Keywords:
exercise barriers, physical activity, older
adults, Hong Kong
摘要
目 標 :
探討在香港某所大學基層醫療診所就醫的老年患者
的身體活動(PA)情況和妨礙他們參加身體鍛煉的因素。
設計:橫斷面問卷調查
設計 :
橫斷面問卷調查
對象 :
在香港某所大學基層醫療診所就醫的60歲及以上
患者。
主要測量內容:
以經驗證的簡版《國際身體活動問卷》
(IPAQ)評估身體活動水準以及自我認為的妨礙鍛煉的
內、外部因素。
結果 :
總體而言,20%(47/235)的應答者身體活動
水準較低。妨礙鍛煉的三個最常見內部因素為“太
累”(59%,139/235)、“太懶”(52%,122/235)、“醫療
問題”(47%,111/235);三個最常見外部因素為“天氣不
好”(49%,116/235)、“沒時間”(37%,87/235)和“沒有
鍛煉夥伴”(28%,65/235)。
結論 :
本研究指出了某所大學基層醫療診所妨礙老年患
者鍛煉的最常見因素,醫護人員可藉此而制定未來開展
身體鍛煉的更佳策略。
關鍵字:
妨礙鍛煉的因素、身體活動、老年人、香港
Introduction
Background
Life expectancy of Hong Kong people rank
amongst the longest in the world. According to the
health facts released by Department of Health in 20191
,
the expectancy of life at birth for men and women in
Hong Kong was 82.2 years and 87.6 years respectively.
Because of the aging population, Hong Kong is facing
more non-communicable diseases (NCD) such as heart
disease, diabetes and cancer. This presents a serious
public health concern. In 2018, the Department of
Health and Food & the Hong Kong Health Bureau
developed a strategic health framework to prevent and
control NCD by 2025.2
One of the targets is to reduce
physical inactivity.
American College of Sports Medicine has launched
a global initiative called “Exercise is Medicine”. The
aim of this is to make both physical activity assessment
and exercise promotion the standard of clinical care.
Primary care physicians are encouraged to work with
their patients to incorporate exercise into their lifestyles.
In The University of Hong Kong (HKU), the University
Health Service (UHS) and the Centre of Sports (CSE)
have collaborated to support this initiative. In order to
have successful implementation of this initiative, full
understanding of the exercise barriers in our elderly
population is crucial in order to modify their exercise
behaviour. Although many studies have explored
the barriers to PA, there are limited local studies on
older adults in the Hong Kong primary care setting.
Therefore, more local research in this field is warranted.
Objecttive
Our study aims to (1) assess the amount and
intensity of physical activity of the older adults who
attend a certain university primary care clinic; (2)
identify the internal and external barriers that may
hinder their participation in exercise.
Methods
Study design
This study was a cross-sectional, anonymous,
helper-assisted questionnaire survey. UHS attendees
who were Cantonese speaking and aged 60 or above
were invited to participate in this study during the data
collection period from November 2019 to January 2020.
The following groups of patients were excluded from
the study: (1) those who declined to take part or would
not give consent to the study; (2) those who could not
understand Cantonese; (3) those who were cognitively
impaired (as documented in their case notes); and (4)
those who had completed the questionnaires before.
The questionnaires would be distributed by healthcare assistants or registered nurses to suitable candidates
before their consultations. The patients would be asked
to complete the questionnaire with the assistance of a helper at the clinic. Two retired registered nurses were
recruited as voluntary helpers for this study. They were
required to attend a briefing session before the start
of the study in order to ensure that they had (1) clear
understanding of the definition of moderate and vigorous
activities; (2) full understanding of the questions; and (3)
complete understanding of the data collection procedure.
Close supervision and support were provided by
the principal investigator during the data collection
period. The completed questionnaires were collected by
the voluntary helpers and subsequently handed over to
the principal investigator for analysis. The completion
of the survey took approximately 10 minutes.
Study population and sampling
The participating clinic serves university students,
staff, dependants and retirees. The study population was
Cantonese-speaking clinic attendees aged 60 or above.
There is no general agreement on the definition of
“older adults” as aging is a dynamic process, and often
the definition is linked to the retirement age. The cutoff of age 60 was chosen as it is the normal retirement
age of university staff. The clinic population of those
aged 60 or above is approximately 4715. For sample
size estimation, the formula for cross-sectional studies
was used, where sample size (SS) = Np(1-p)]/ [(d2
/
Z2
1-α/2*(N-1)+p*(1-p)] [9]. Given a population size (N)
of 4715, a hypothesised proportion (p) of 0.2, and a
margin of error (d) of 0.05, the sample size required
was 234 with 95% confidence level.
Survey instrument
The short version of International Physical Activity
Questionnaire (IPAQ) was used to assess the level of
PA in the last 7 days. The validity and reliability of the
IPAQ had been tested in 12 countries among adults aged
18 – 6510, as well as in Hong Kong.11 Further studies12-13
evaluated the validity and reliability of IPAQ used in
the elderly, and it was concluded that the short version
of IPAQ was a useful and valid tool for assessing PA
among elderly adults.
The IPAQ used in our study was the short Chinese
version (IPAQ-C) originally translated by Macfarlane
et al11 according to the procedures recommended by the
International Consensus Group for the Development of
the IPAQ and with cultural adaptations made. It involved
translation and back translation from the original English
version. The IPAQ-C was shown to be valid and reliable
for assessment in older Chinese adults.14
The barriers to exercise were assessed with a list of
items developed after review of previous studies, including
the focus group discussion by Larkin et al. in 200515, a
Hong Kong study by Chou et al in 200816 and a study by
Justine et al. in 2013.17 The final questionnaire consisted
of 18 questions that gave a comprehensive cover of the
perceived exercise barriers in older adults. The barriers
could be broadly divided into internal and external.
External barriers were those one might not be able to
control, and internal barriers were those which could be
determined by one’s own decisions.17-18 Participants were
asked to rate the barriers on a 4-point Likert scale (1 =
Not at all, 2 = Rarely, 3 = Occasionally, 4 = Always)
The content validity of each question was rated
on a 4-point Likert scale (not relevant, somewhat
relevant, quite relevant, and highly relevant). Based
on the proportion of experts who rated a question as
quite or highly relevant, the item-level content validity
index (CVI) was computed.19 The item-level CVIs of
all the questions were rated 1.00, thus the scale-level
CVI computed was also 1.00. Some wordings of the
questions were changed after review in order to make
it more reader-friendly. Pilot testing was performed
in 20 patients from different backgrounds before the
questionnaire was finalised.
Statistical analysis
Data was analysed using the open source software
“R” for statistical computing version 3.4.4 (2018-
03-15).20 Frequency tables were computed to check
for range and completeness. Descriptive statistics
were computed to summarise and express the data
in percentages, with calculated means and standard
deviations where applicable.
A multiple logistic regression analysis explored the
demographic predictors to low level of physical activity.
Mann-Whitney U-test was used to compare the mean
Likert score on the barriers between those with low level
of PA and those with adequate level of PA. Mann-Whitney
U-test is preferred over t-test because the variables in
the two groups were not normally distributed. Statistical
significance was established at P < .05 for all tests.
Ethical consideration
This was an anonymous study. Participation was
voluntary and involved minimal risk. Those who agreed
to participate were deemed to have given consent for
their data to be used for research purposes. Refusal to
participate would not incur any negative consequences and
would have no impact on their medical care. Approval from
the Human Research Ethics Committee of The University
of Hong Kong was received before commencement of data
collection (Reference: EA 1910031).
Result
A total of 252 questionnaires were distributed and
240 were returned, which yielded a response rate of
95.2%. Among the returned questionnaires, five were
excluded from analysis due to grossly incomplete data (e.g.
missing most demographic data or a whole section of the
questionnaire). A total of 235 completed questionnaires
were used for final analysis. This represented about 5% of
the clinic population of those aged 60 and above (N=4715).
Socio-demographics
The characteristics of the respondents were shown
in Table 1. 53.2% (125/235) of the respondents were
female and 46.8% (110/235) were male. Approximately
half of the respondents were in the age group 60-64
(48.1%, 113/235). This survey was taken in a university
clinic setting. The respondents spanned all education
levels but about half of them completed tertiary or even
higher education (53.6%, 126/235). Majority of the
respondents were retirees (63.8%, 150/235). Although
77% (181/235) suffered from chronic medical conditions
requiring regular follow-up or treatment, more than half
of the respondents rated their own health as good, very
good or excellent (62.1%, 146/235), and only 3.4%
(8/235) rated their health as poor.
Level of physical activity
The respondents’ level of PA was assessed using
the short version of IPAQ. According to the IPAQ
scoring protocol 21, the total metabolic equivalent
(MET) score of each participant was calculated and the
participants were then categorised into three groups
according to their level of PA. The criteria of moderate
and high level of PA required total activity of at least
600 and 3000 MET-minutes/week respectively. Anyone
with a total activity below 600 MET-minutes/week was
categorised as low level.
Table 2shows the types and level of PA of our
study population. 20% (47/235) of the respondents had
low level of PA. 64.7% (152/235) had moderate level of
PA and 15.3% (36/235) had high level of PA. Walking
was the most common form of activity in all groups.
The percentage of contribution by walking in the low,
moderate and high-level activity groups were 81.3%,
65.2% and 57.6% respectively.
Demographic predictors of low level of physical activity
Multiple logistic regression analysis (Table 3) was
computed to explore the impact of various demographic
data on the respondents’ level of PA. PA level below
600 METS/min per week was used as the target
variable. After adjusting for other covariates, overall the
demographic variables were not very strong predictors
of low-level exercisers. They had minimal impact on the
level of PA except for age group 70-74 which showed a
significant P value of .034.
Barriers to exercise
Figure 1shows the ranking of the internal barriers
to exercise participation among the respondents. The
three most common internal barriers to exercise are “too
tired” (59%), “too lazy” (52%), and “health problem”
(47%). And the three most common external barriers are
shown inFigure 2. They are “bad weather” (49%), “lack
of time” (37%), and “no one to exercise with” (28%).
Among all the barriers, the least likely ones are “feeling
shy” (8%), “cost” (12%), “interfere with work” (13%),
and “lack of transportation” (19%).
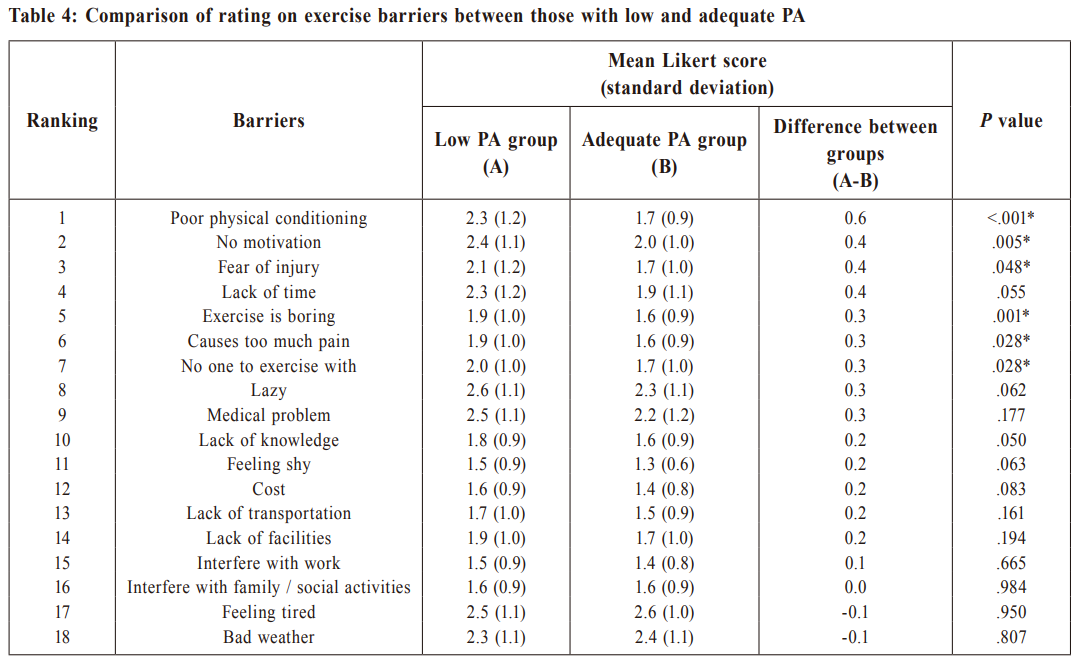
Comparison of impact of barriers between those with
low and adequate level of PA
According to the IPAQ scoring protocol21, anyone
with a total activity below 600 MET-minutes/week was
categorised as low level of PA. Table 4 shows the result
of the Mann-Whitney U-test comparing the mean Likert
score on the barriers between those with low level of
PA and those with adequate level of PA. Significant
differences were found for the following barriers with
P value < .05, which means that they are the important
barriers to the low-level exercisers: (1) poor physical
conditioning; (2) no motivation; (3) exercise is boring;
(4) fear of injury; (5) causes too much pain; and (6) no
one to exercise with.
Discussion
Principal findings
About 20% of the respondents were found to be
underactive, defined as less than 600 MET-min/ week.
This result is similar to the report published by the
Hong Kong Department of Health in 2015.8
Among
all the activities, it is worth noting that walking was
found to be the most common physical activity and
it contributed to about 63% of the total METS in our
study population. This was also observed in the Deng
et al.’s study14, in which the METS contributed by
walking was around 75%. Walking is a common form
of activity because it is simple and easily accessible.
A Japanese Study22 on elderly men without critical
illness found that walking for 2 or more hours per
day could lower the all-cause mortality. Thus, walking
should be promoted in the underactive elderly adults
because it can easily be fitted into their daily routine. In
addition, walking has a lower rate of injury.23 However,
multi-parameter exercise programme should also be
considered, including muscle strengthening and balance
exercise as advised by the World Health Organisation.24
studies showed that multi-component exercise
intervention could improve the balance and mobility25;
and help to prevent falls in older adults.26-27
Our study also illustrated the most common internal
and external exercise barriers.
The most common internal barriers were “too
tired”, “too lazy”, and “medical problem”. In Justine
et al’s study17, 51.7% respondents also considered
“too tired” as an important barrier to participation in
exercise among older adults. Therefore, the exercise
programme introduced to older adults should be
individualised. Introductory short sessions can be
considered to avoid exhaustion of the participants and
the intensity and duration of the exercise programme
can be adjusted accordingly.
Feeling too tired or being too lazy may also reflect
a lack of motivation, which is a significant determinant
of exercise participation28 and exercise adherence. 29
Lack of motivation was considered as a barrier in 37%
of our respondents. Motivation can certainly affect
behaviour. The question is how we can motivate people
to exercise. One study showed that participation in
sports during adolescent was associated with a higher
level of physical activity in later adulthood.30 Therefore,
exercise programme should be promoted early in life.
Larkin et al15 performed a qualitative study on 86
adults aged 65 or above using in-depth interview to
identify their perceived barriers to exercise. They found
that the most prevalent perceived barrier to exercise
among the respondents was "medical problem" (38%).
Our study had similar findings. As it is common for
those with chronic illness to believe that exercise may
do more harm than good, effective management of
their medical problems is essential. In addition to this,
primary care physicians should also give clear and
proper guidance on exercise programmes. The exercise
prescription should be tailor-made for the individual
and it should include the type, frequency, duration and
intensity.31 This is particularly important for low-level
exercisers. As shown in our study, these patients had
more fears of injury and more doubts in their ability to
undertake physical activity.
Among the external barriers, “bad weather”, “lack
of time”, “no one to exercise with” were found to be
significant barriers in our study. Studies other than ours
had shown that “lack of facilities” was a significant
external barrier16-17 but not in ours. This could be related
to the easy access to sports facilities at our University
for staff and retirees. The free access introduced in
2018 has further encouraged more staff and retirees to
participate in exercise and has made “cost” less of a
concern. In fact, cost was found to be one of the least
common barriers in our study.
In Chou et al’s study16, 38% of Chinese respondents
agreed or strongly agreed that “too hot” or “too cold”
was a barrier to do exercise. In our study, 49% of the
respondents believed that weather was a barrier to
exercise. Thus, indoor or home exercises programme
should be promoted among the older adults so that
their participation will be less likely to be affected by
adverse weather.
“Lack of time” was another major barrier found in
our study. This is consistent with previous research.16-17
Some studies found that small bouts of exercise can be
beneficial32 and improve adherence.33 This can be an
alternative for those who believe that they have little
time for exercise.
“Lack of transportation” was not found to be a
crucial barrier in our study. It makes sense as Hong Kong
has a highly sophisticated transport network, and this
makes most of the sporting facilities easily accessible.
In addition, our study showed that the most common
exercise was walking which can be performed anywhere.
By comparing between those with low level of
PA and those with adequate PA, we found that certain
exercise barriers had more significant impacts on the
low-level exercisers. In order to overcome the barrier
“no one to exercise with”, more group exercise classes
can be planned. Ideally, the class should be led by an
experienced fitness instructor, who can give proper
advice to the participants on how to improve their
fitness and how to prevent injury. That would help to
attenuate the concerns of “poor physical conditioning”
and “fear of injury”. Other benefits of group class
include making new friends among the participants and
making exercise less boring. Peer support may also
improve the motivation and adherence to the exercise
programme. In relation to the concern of “causing too
much pain”, apart from proper advice on warm up and
cool down, healthcare providers can explain to the
participants that the pain is only temporary and the
long-term benefits of exercise outweigh the pain.
Relevance to clinical setting
At HKU, the UHS has collaborated with the CSE
to support the initiative “Exercise is Medicine”. In order
for the implementation to be successful, our doctors
and our sport coaches should acknowledge the concerns
of the older adults and ensure that the prescriptions
are practical and achievable. There is no one-size-fitsall approach, especially in those with chronic medical
conditions. With the information obtained from this
study, we can develop better strategies in exercise
promotion among the older adults. The programmes
organised should be accessible, inexpensive and
enjoyable, e.g. easy trail walks. Proper guidance is
essential and small bouts of exercise can be considered.
If the above pilot programme is successful, it can then
be extended to the community
Strengths and limitations
Although many overseas studies were performed
to explore the barriers to PA or exercise, there are not
many local studies involving older Chinese adults in
Hong Kong, especially in the primary care setting. A
high response rate of 95% was achieved in our study.
Retired nurses were recruited to assist the completion
of the questionnaires and supervision was also given to
them in order to obtain high quality data.
As the study was taken in a university clinic,
the data is skewed towards more educated and
affluent patients, therefore the study’s external
validity is reduced. As the physical activity level
was self-reported, reporting bias was possible. More
accurate level of PA can be obtained if pedometer or
accelerometer are used for assessment of PA but it
would require more resources. Our study only explored
the exercise barriers, nevertheless it is also important
to explore the motivators as they can be inter-related.
Exercise behaviour can be affected by both. Therefore,
further study such as a focus group discussion can be
considered to explore the motivators of exercise.
Conclusion
Despite awareness of the various documented health
benefits, some older adults still do not have adequate
PA. This study highlighted the most common barriers
which may hinder their participation in exercise. In the
university setting, by acknowledging the above, the
UHS can work with the CSE to develop better exercise
programmes for their elderly staff and retirees. Physical
activity assessment and exercise promotion should be
part of the standard of primary care. In the community
setting, the same practice should be applied but that
will require collaboration between the government, nongovernment organisations, medical and non-medical
professionals. More resources should be allocated to
develop appropriate exercise programmes to promote
healthy aging. These will benefit the general population
in the long run and hence lessen the medical burden to
the society.
Acknowledgement
We would like to thank Mr. Tommy Lai for his
assistance in statistical analyses, and all the clinic staff
for their assistance during the research period.
Olivia B Y Choi, MBBS (New South Wales), FRACGP, MSpMed (New South Wales)
Physician
University Health Service, The University of Hong Kong
David K K Wong,MBChB (CUHK), FRACGP, FHKCFP, FHKAM (Family Medicine)
Physician
University Health Service, The University of Hong Kong
Man-kuen Cheung,MBBS (HK), FRACGP, FHKCFP, FHKAM (Family Medicine)
Director
University Health Service, The University of Hong Kong
Correspondence to: Dr Olivia B Y Choi, University Health Service, 2/F Meng Wah
Complex, The University of Hong Kong, Pokfulam, Hong Kong SAR
E-mail: ochoi14@hku.hk
References:
-
Department of Health facts of HK 2019. Available from: https://www.dh.gov.hk/english/statistics/statistics_hs/files/Health_Statistics_pamphlet_E.pdf
[accessed 2020 March 8]
-
Department of Health. Towards 2025 – Strategy and action plan to prevent
and control NCD in Hong Kong. 2018. Available from: https://www.chp.gov.
hk/files/pdf/saptowards2025_fullreport_en.pdf [accessed 2020 March 8]
-
Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health
in older adults: recommendation from the American College of Sports
Medicine and the American Heart Association. Med Sci Sports Exerc.
2007;39(8):1435-1445.
-
Hamer M, Lavoie KL, Bacon SL. Taking up physical activity in later life &
healthy. Br J Sports Med. 2014;48:239-243.
-
Vagetti GC, Barbosa Filho VC, Moreira NB, et al. Association between
physical activity and quality of life in the elderly: a systematic review, 2000-
2012. Braz J Psychiatry. 2014;36(1):76-88.
-
McPhee JS, French DP, Jackson D, et al. Physical activity in older age:
perspectives for healthy ageing and frailty. Biogerontology. 2016;17(3):567-580.
-
Alty J, Farrow M, Lawler K. Exercise and dementia prevention. Pract
Neurol. 2020;20(3):234-240.
-
Department of Health. Action plan to promote healthy diet & physical activity
participation in HK, 2015. Available from: https://www.change4health.gov.hk/
filemanager/common/image/strategic_framework/action_plan/action_plan_e.pdf
[accessed 2020 March 8]
-
Dean A, Sullivan K, Soe M. Open source epidemiologic statistics for public
health. OpenEpi. 2013. Available from: https://www.openepi.com/Menu/OE_
Menu.htm [accessed 2020 March 1]
-
Craig CL, Marshall AL, Sjöström M, et al. International physical activity
questionnaire: 12-country reliability and validity. Med Sci Sports Exerc.
2003;35(8):1381-1395.
-
Macfarlane DJ, Lee CC, Ho EY, et al. Reliability and validity of the Chinese
version of IPAQ (short, last 7 days). J Sci Med Sport. 2007;10(1):45-51.
-
. Tomioka K, Iwamoto J, Saeki K, et al. Reliability and validity of the
International Physical Activity Questionnaire (IPAQ) in elderly adults: The
Fujiwara-kyo Study. J Epidemiol. 2011;21(6): 459-465.
-
Chun MY. Validity and reliability of Korean version of International Physical
Activity Questionnaire short form in the elderly. Korean J Fam Med.
2012;33(3):144-151.
-
Deng HB, Macfarlane DJ, Thomas GN, et al. Reliability and validity of the
IPAQ-Chinese: the Guangzhou Biobank Cohort study. Med Sci Sports Exerc.
2008;40(2):303-307.
-
Larkin JM, Black DR, Blue C, et al. Perceived barriers to exercise in people
65 and older: recruitment and population campaign strategies. Medicine &
Science in Sports & Exercise. 2005;37(suppl 5):S12.
-
Chou KL, Marfaclane DJ, Chi I, et al. Barriers to exercise scale for chinese
older adults. Topics In Geriatric Rehabilitation. 2008;24(4):295-304.
-
Justine M, Azizan A, Hassan V, et al. Barriers to participation in physical
activity and exercise among middle-aged and elderly individuals. Singapore
Med J. 2013;54(10):581-586.
-
Korkiakangas EE, Alahuhta MA, Laitinen JH. Barriers to regular exercise
among adults at high risk or diagnosed with type 2 diabetes: a systematic
review. Health Promot Int. 2009;24(4):416-427.
-
Polit DF, Beck CT. The content validity index: are you sure you know
what's being reported? Critique and recommendations. Res Nurs Health.
2006;29(5):489-497.
-
R core team. R: A Language and Environment for Statistical Computing.
Vienna, Austria. R foundation for Statistical Computing. 2019. Available
from: https://www.R-project.org [accessed 2020 March 8]
-
. Patterson E. International physical activity questionnaire scoring protocol.
2010. Available from: https://sites.google.com/site/theipaq/scoring-protocol
[accessed 2020 March 3]
-
Zhao W, Ukawa S, Kawamura T, et al. Health benefits of daily walking on
mortality among younger-elderly men with or without major critical diseases
in the new integrated suburban seniority investigation project: a prospective
cohort study. Journal of Epidemiology. 2015;25(10):609-616.
-
Powell KE, Heath GW, Kresnow MJ, et al. Injury rates from walking,
gardening, weightlifting, outdoor bicycling, and aerobics. Med Sci Sports
Exerc. 1998;30(8):1246-1249.
-
World Health Organization. Global recommendations on physical activity for health
65 years and above. 2011. Available from: https://www.who.int/dietphysicalactivity/
publications/recommendations65yearsold/en/ [accessed 2020 March 8]
-
Bird M, Hill KD, Ball M, et al. The long-term benefits of a multi-component
exercise intervention to balance and mobility in healthy older adults. Arch
Gerontol Geriatr. 2011;52(2):211-216.
-
. Ishigaki EY, Ramos LG, Carvalho ES, et al. Effectiveness of muscle
strengthening and description of protocols for preventing falls in the elderly:
a systematic review. Braz J Phys Ther. 2014;18(2):111-118.
-
Karlsson MK, Magnusson H, von Schewelov T, et al. Prevention of falls in
the elderly--a review. Osteoporos Int. 2013;24(3):747-762.
-
Sherwood NE, Jeffery RW. The behavioral determinants of exercise: implications
for physical activity interventions. Annual Review of Nutrition. 2000;20(1):21-44.
-
Chao D, Foy CG, Farmer D. Exercise adherence among older adults:
challenges and strategies. Control Clin Trials. 2000;21(5 Suppl):212S-7S.
-
Tammelin T, Näyhä S, Hills AP, et al. Adolescent participation in sports and
adult physical activity. Am J Prev Med. 2003;24(1):22-28.
-
Department of Health. Exercise prescription doctor’s handbook. 2012.
Available from: https://www.chp.gov.hk/archive/epp/files/DoctorsHanbook_
fullversion.pdf [accessed 2020 October 17]
-
Murphy MH, Hardman AE. Training effects of short and long bouts of brisk
walking in sedentary women. Med Sci Sports Exerc. 1998;30(1):152-157.
-
Jakicic JM, Winters C, Lang W, et al. Effects of intermittent exercise and
use of home exercise equipment on adherence, weight loss, and fitness in
overweight women: a randomized trial. JAMA. 1999;282(16):1554-1560.
|
