A clinical audit on secondary preventive care
in patients with ischaemic heart disease in a
public primary care clinic in Hong Kong
Yin-mei Liu 廖燕媚, Chi-hang Lau 劉知行, Catherine XR Chen 陳曉瑞, Yim-chu Li 李艷珠
HK Pract 2022;44:106-115
Summary
Objective:
To audit the secondary preventive care in
patients with ischaemic heart disease (IHD) managed in
a public primary care clinic in Hong Kong.
Method: Study design:
Clinical audit with comparison
of two samples from a case series at different time
points.
Setting:
A public General Outpatient Clinic
(GOPC) in the Hospital Authority of Hong Kong.
Subject:
All stable IHD patients who had been regularly followed-up
at Robert Black GOPC during the audit cycle were
recruited. Evidence-based audit criteria and performance
standards were set after reviewing data from local and
overseas audit studies and latest international guidelines.
Phase 1 evaluation was performed from 1st June 2017
to 31st December 2017, and areas of deficiency were
identified. Active interventions were implemented for
12 months and Phase 2 evaluation was carried out
from 1st January 2019 to 31st July 2019. Chi-square test
and student’s t test were used to detect statistically
significant changes between Phase 1 and Phase 2.
Results:
Phase 1 data showed pronounced deficiencies
in the assessment and control of cardiovascular disease
(CVD) risk factors. For CVD risk factor control, only 34%
and 18.4% of patients can achieve the optimal blood
pressure (BP) control target and lipid control target
respectively. The glycaemic control rate was 49.3%
among patients with diabetes mellitus (DM). Following
active intervention, marked improvements in outcomes
were observed. Phase 2 data showed that optimal
BP control rate and lipid control rate were achieved
in 58.5% and 58.4% of targeted patients respectively
(P<0.001), while the optimal glycaemic control rate was
improved to 70.5% (P=0.008).
Conclusions:
Through the process of identifying
deficiencies and implementing effective enhancement
strategies in managing IHD patients in public primary
care clinics, the control of CVD risk factors had been
significantly improved. It is postulated that the mortality
and morbidity of IHD patients would be reduced in the
long run.
摘要
目的 :
在香港醫院管理局轄下一所普通科診所對非急性缺
血性心臟病患者的二級預防進行循證審計。
方法 :
所有患有缺血性心臟病而病情穩定的病人,
如於審計週期內有於柏立基普通科門診定期覆診並
符合研究標準,將被納入本審計。本審計所取用的
準則與標準均於參照了本地及國際的審計與最新的
臨床指引之後釐定。透過於2017年6月1日到2017年
12月31日進行的第一週期評估,識別了處理不足之
處。再進行了12個月的積極改進,而第二期週期評
估於2019年1月1日至2019年7月31日進行。卡方檢驗
和學生檢驗被用於檢測第一期與第二期評估之間的
統計學顯著變化。
結果 :
第一期週期數據顯示了在心血管高危因素的評估和控制方面都存在明顯的不足。分別只有34%
及18.4%的病人能達到血壓及血脂的控制目標,而
49.3%的糖尿病患者能達致理想的血糖控制。經過
積極改進後,達到了明顯的改善。第二週期的數據
顯示分別有58.5%及58.4%的病人能達到血壓及血脂
的控制目標(p <0.001),而理想血糖控制率則上升至
70.5% (P=0.008)。
結論 :
通過於公營普通科門診識別對缺血性心臟病患
者二級預防的不足之處,再實施有效的管理策略,可
以顯著改善心血管高危因素的控制。據推測,此類心
臟病患者長遠之死亡率和發病率將降低。
Introduction
Ischaemic heart disease (IHD) is an important
disease both in Hong Kong (HK) and worldwide.
Its incidence is increasing and it is associated with
significant morbidity and mortality. The World Health
Organization ranked IHD as the top cause of global
death in 2016.1 It caused more than 0.36 million deaths
in the United State in 20152 and contributed around 1.8
million deaths annually (20% of all death) in Europe.3
In Hong Kong, the number of in-patient discharges
and deaths due to IHD had risen by 45% in the past
decades.4 Local data in HK in 2017 showed there were
3,867 deaths (8.4% of all registered deaths) attributed
to IHD.5
There is strong evidence supporting comprehensive
risk factors modification via lifestyle changes and
medical treatment can help decrease mortality, reduce
risks of subsequent cardiac events, and improve quality
of life.6,7 However, quality of secondary preventive care
of IHD patients was far from optimal. A clinical audit
carried out in South Auckland in 2001 revealed that a
large proportion of post-IHD patients were not receiving
optimal care, with only 45% of dyslipidaemia, 39%
of diabetic and 59% of hypertensive patients having
achieved the desired treatment target. Only 34% of
patients were prescribed Angiotensin-converting Enzyme
Inhibitor (ACEI), and 29% patients were not prescribed
statins even when they were indicated.8 Another study
in the United State also revealed an underuse of statin
in post-IHD patients, with statin prescribed in 58.4% of
patients only.9
Previously, IHD management is mainly the
responsibility of cardiologists in the specialist setting.
With the increasing service demand in IHD care due
to an aging population and in view of the robust
development of family medicine in Hong Kong, more
IHD patients are advised to have continued care
by primary care doctors upon their discharge from
hospitals. For example, according to the preliminary
data from the Head Office of the Hospital Authority
(HAHO), over 50, 000 IHD cases are now being looked
after by family physicians in the General Outpatient
Clinics (GOPCs) of HA. In addition, over 50 percent
of attendances at the clinic where the author is working
are due to chronic disease management, with 6 percent
of chronic disease attendances being attributed to IHD.
Therefore, it is of paramount importance that IHD
care at the primary care clinics is regularly reviewed
to ensure that effective preventive measures are taken.
Having said so, local data on the performance of
secondary preventive care of IHD patients managed
in the public primary care settings is still lacking
until now. In view of this, this study aims to audit the
management of IHD cases from a primary care clinic of
HA and to work out improvement strategies. We believe
that by improving the standard of care of IHD patients
managed in the community via the audit approach, the
disease burden including the mortality and morbidities
of CVD could be greatly reduced in the long run.
Objective
Implications for clinical practice or policy
This clinical audit demonstrated common problems
encountered in secondary preventive care of patients
with non-acute ischaemic heart disease. Through the
process of clinical audit via a team approach targeting
at clinic, doctor, nurse and patient levels, noticeable
improvement in patient care was achieved.
Methods
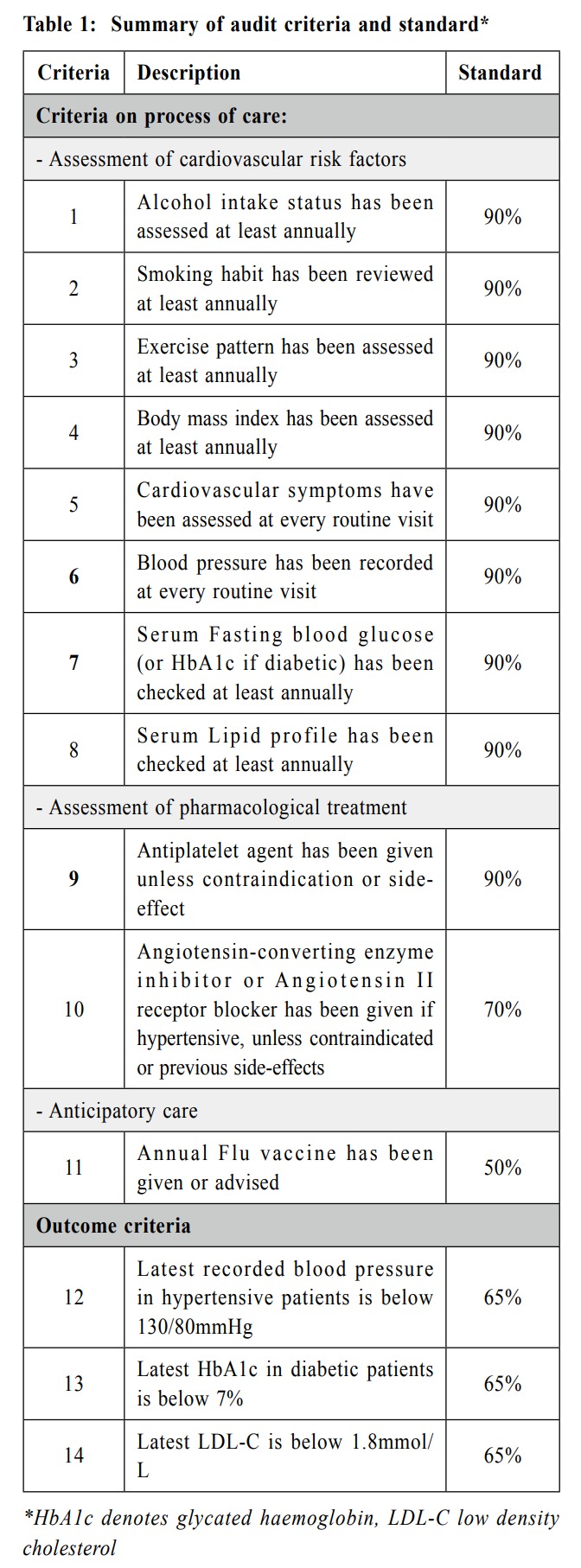
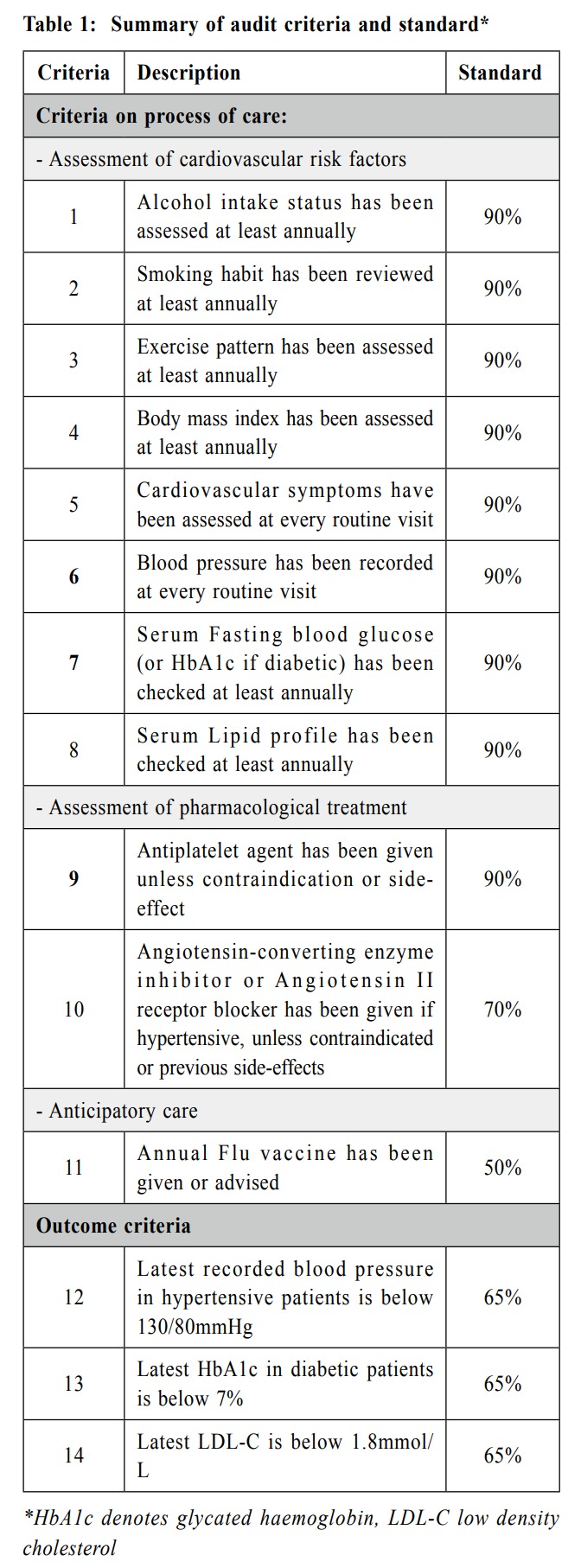
Setting audit criteria and justification of audit standards
Guidelines on IHD management published in
the recent 10 years were identified from the PubMed
(https://pubmed.ncbi.nlm.nih.gov/). After thorough
literature review, the following evidence-based audit
criteria and performance standards were adopted for this
IHD audit (Table 1).
The criteria were adopted from the following
evidence-based international guidelines:
-
Dyslipidaemias 2016 (Management of) ESC
Clinical Practice Guidelines” published by
European Society of Cardiology.10
-
AHA/ACCF secondary prevention and risk
reduction therapy for patients with coronary
and other atherosclerotic vascular disease:
2011 updated" by American College of
Cardiology Foundation and American Heart
Association.11
Criteria 1-8 were classified as ‘must do’ criteria
with the standard set at 90%, as these are important for
CVD risk factor or symptom identification for which
subsequent effective secondary prevention strategies
could be adopted. For criteria 12-14 (to assess outcome
performance on blood pressure, glucose, and lipid
control), the standard was set at 65% with reference to
local audit protocols on management of HT and DM12,13,
local audit and cohort study on secondary prevention
of stroke in primary care14,15, and regular reviews of
BP, lipid and glycaemic control in hypertensive and
diabetic patients in the primary care performed by the
HA. Table 1 summarised the criteria and standard of
this audit.
Audit subjects
All patients with stable non-acute IHD coded by
International Classification of Primary Care (ICPC) K74
(IHD with angina) and K76 (IHD without angina) who
have been regularly followed-up at our Robert Black
GOPC during the audit cycle (phase 1 from 1 Jun 2017
to 31 Dec 2017 and phase 2 from 1 Jan 2019 to 31
July 2019) were included. Non-acute IHD refers to a
reversible supply/demand mismatch related to ischemia, a
history of myocardial infarction, or the presence of plaque
documented by catheterisation or computed tomography
angiography. Patients were considered stable if they
were asymptomatic or their symptoms were controlled
by medications or revascularisation.16 Exclusion criteria
were patients followed-up by Medical Outpatient Clinic
(MOPC), patients with sporadic consultation, wrongly
diagnosed patients, acute IHD, or those certified dead.
First-phase data collection
Totally 499 stable IHD patients were identified in
the first cycle. Assuming the confidence level being
95% and confidence interval being 5%, by using the
formula:
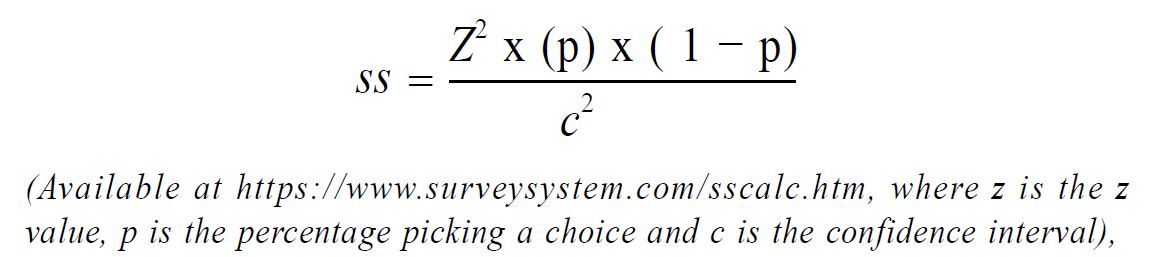
a sample size of 217 was needed. To allow room for
case exclusion, a total of 228 were selected. Therefore,
228 randomly chosen number from 1 to 499 were
generated using an online computer programme “Research
Randomizer” available at https://www.randomizer.
org/#randomize.17 Among the 228 patients included,
11 patients were excluded according to the exclusion
criteria, with 3 patients being followed-up in MOPC, 2
patients with wrong diagnosis, 2 patients with sporadic
consultation and 4 patients certified dead. The remaining
217 cases were included in the data analysis.
Implementing changes and intervention:
1st January 2018 to - 31st December 2018
After reviewing areas of deficiencies, a clinic team
approach with changes targeting at different levels were
adopted. Educational seminar was arranged for doctors,
with updated international guidelines and deficiencies in
disease management reviewed. Audit criteria summary
was affixed on the desk of all consultation rooms for
easy reference. Specific management plan was inputted
in the reminder in the CMS (Clinical Management
System) to facilitate communication with doctors.
Progress of intervention was reviewed via the monthly
clinic meetings.
At the nurse level, nurses were reminded to review
the patient’s lifestyle risk factors in particularly smoking
status, drinking habit and exercise pattern. Patient
counselling and education would be provided and were
based on updated guidelines. Possible deficiencies and
corresponding implementation strategies are summarised
in Table 2.
Second-phase data collection and analysis
504 IHD patients in total were found to have
regular follow-up in the clinic during the second cycle.
A sample size of 218 was needed to achieve the same
confidence level and interval as described in the first
cycle. To allow room for case exclusion, 233 cases
were randomly selected from the case cohort for review.
Among them, 15 patients were excluded (4 patients
followed-up in the MOPC, 3 patients with wrong
diagnosis, 3 patients with sporadic consultation and 5
patients certified dead) and the remaining 218 cases
were included in the data analysis.
Determination of variables
The patient’s age, gender, smoking and drinking
status, body mass index (BMI), blood pressure (BP),
haemoglobin A1c (HbA1c) level if diabetic and lipid
profile were retrieved from the Clinical Management
System (CMS). The most recent clinic BP or blood test
were used for analysis if more than one reading or test
had been performed during the study period. The BMI
was calculated as body weight/body height2 (kg/m2).
Data analysis
SPSS software (version 25) was then used for data
analysis. The chi-square test was used to analyse the
categorical variables and paired student’s test was used
for continuous variables to identify the differences of
the measurements between the two phases. P value
<0.05 is considered as statistically significant.
Results
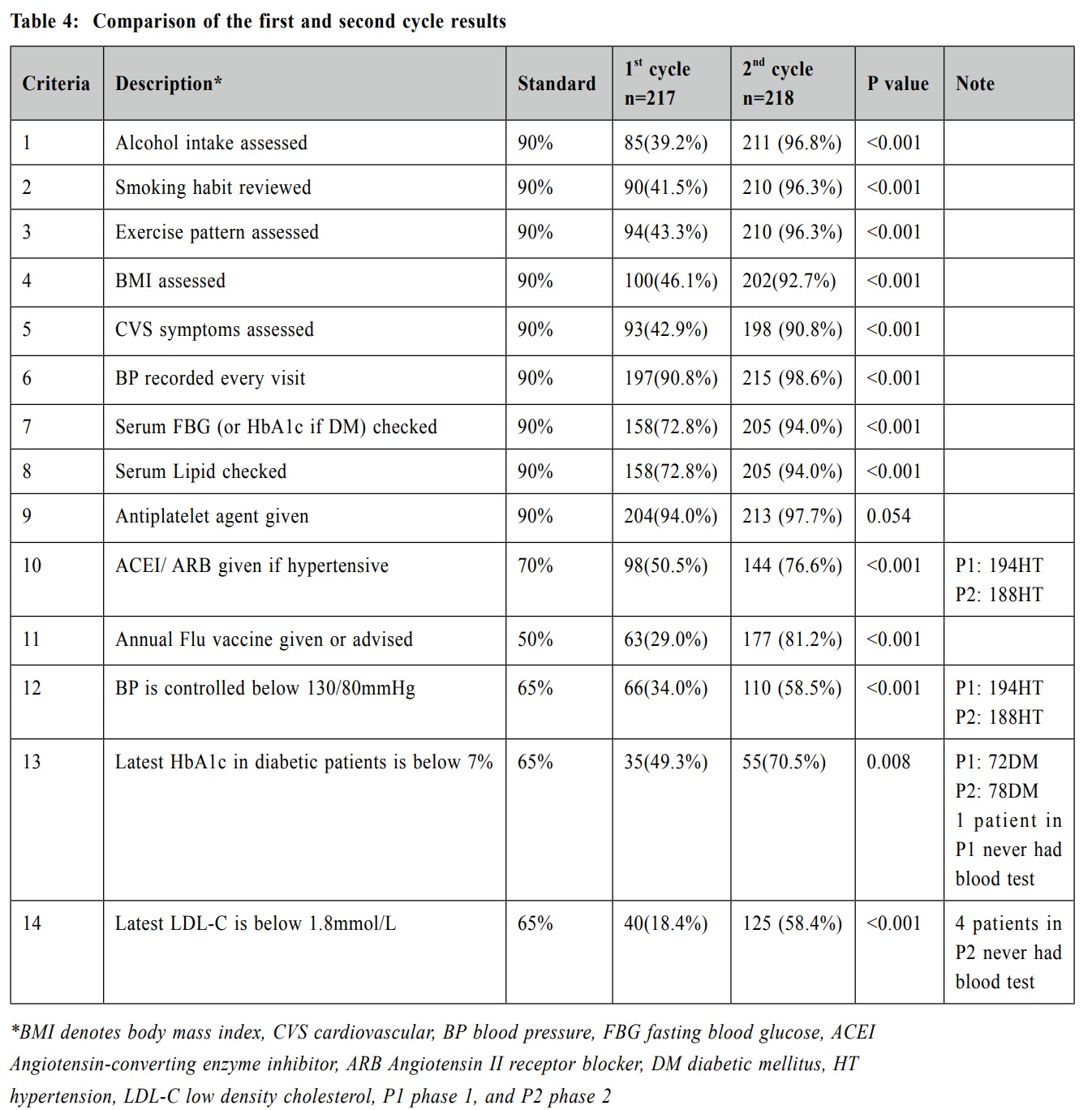
Table 3 summarises the demographic characteristics
of IHD patients recruited into the two phases. Their
background demographic parameters were comparable.
A comparison of the performance achieved in the two
phases is summarised in Table 4. Proper assessment of
CVD risk factor in phase 1 was far from satisfactory,
with inadequate documentation of alcohol use (39.2%),
smoking status (41.5%), exercise pattern (43.3%), BMI
(46.1%), cardiovascular symptoms (42.9%), blood sugar
(72.8%) and lipid profile (72.8%). Satisfactory BP,
glycaemic and lipid control were attained only in 34.0%
of the hypertensive, 49.3% of the diabetic and 18.4% of
dyslipidaemia patients respectively. Annual flu vaccine
was only given or advised in 29.0% of patients. Criteria
that met standard set included recording of BP (90.8%)
and anti-platelet given (94.0%).
After 12 months of active intervention and
implementation of changes, marked improvement in
most of these criteria was demonstrated in phase 2.
All of the 11 process criteria in the second cycle met
the desired standard. (criteria 1-11, all p value <0.001
except p value=0.054 concerning use of anti-platelet
agents). Optimal BP and lipid control were achieved in
58.5% and 58.4% of the targeted patients respectively
(P<0.001). 70.5% diabetic patients reached the set
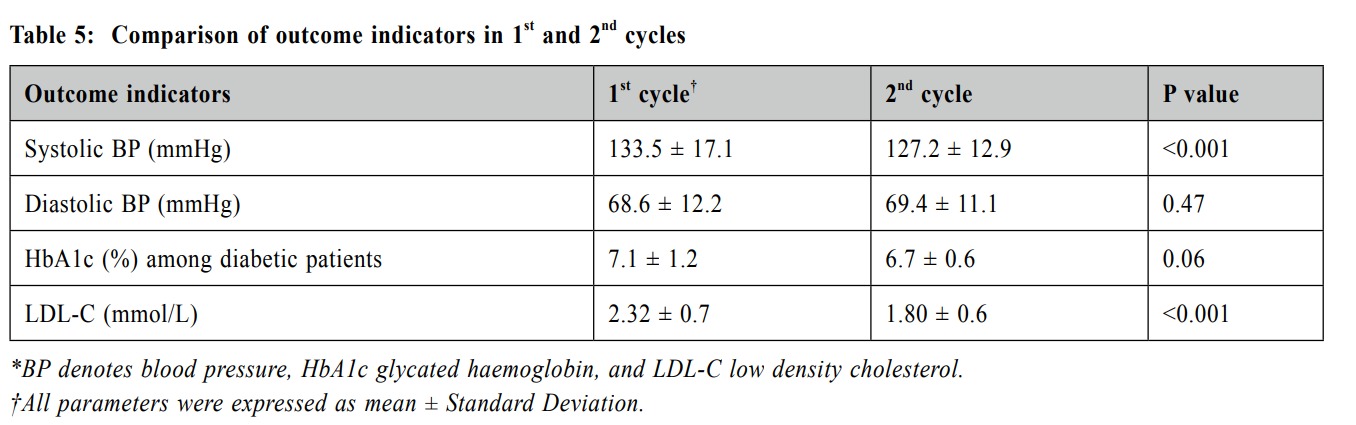
standard (P=0.008). Table 5 summaries the comparison
of outcome indicators in 1 st and 2 nd cycle.
Discussion
This study was the first local clinical audit on
secondary prevention of stable IHD in a public primary
care setting and has provided important background
information on IHD management in the community.
-
Criteria that did not meet standard in phase 1,
then met in phase 2:
Criteria 1-4
(assessment of drinking status, smoking
status, exercise pattern and BMI)
Assessment of these CVD risk factors was far
from optimal. Doctors’ lack of awareness on these
assessment and limited consultation time were
the main reasons. Following active intervention,
doctors’ awareness was enhanced and significant
changes were achieved. Similar standard was met
in other local studies. A local stroke audit achieved
a standard of >90% on evaluation of these risk
factors15. A local cohort study on stroke prevention
protocol also reached a standard of >90%, with the
exception of the assessment rate of BMI which was
79.3%14.
Criterion 5
(assessmenton cardivoascular symptoms)
Only 93 patients (42.9%) were properly
assessed about their CVS symptoms during the
first cycle. Most doctors expressed that they would
routinely discuss CVS symptoms with their patients
during their consultations. The low performance
index was likely due to poor documentation. Target
standard was reached in phase 2 (90.8%, P<0.001).
Criteria 7 & 8
(FBG/ HbA1c and fasting lipid checked)
Although not meeting the desired standard,
a relative good performance of 72.8% was found
in phase 1. Doctors were aware of the importance
of regular blood test but there was no consensus
on the regularity of blood test, with some doctors
checking it annually, some checking every two
years. Some doctors were less motivated to offer
blood test to the elderlies aged 90 or above, with
14.3% and 12.8% of IHD patients being 90 years
old or above in phase 1 and phase 2 respectively.
Some patients refused blood test due to busy
schedule or lack of awareness on the importance of
regular blood test.
After the concerted effect, the set standard was
met in phase 2. A local stroke audit also achieved
a standard of 91% in annual checking of glycaemic
and lipid control in the second phase15. Internal
data in HA showed 94.1% of diabetic patients had
HbA1c hecked within one year. Another local study
on the quality of diabetic care also showed it could
achieve >90% annual monitoring of lipid.18
Criterion 10
(use of ACEI/ ARB in hypertensive patients)
Only 50.5% of hypertensive patients fulfilled
this criterion in phase 1. This is consistent with
findings from the Hong Kong Cardiovascular
Task Force Risk Management Program showed
that 63.5% of hypertensive patients under medical
treatment were put on ARB.19 Some doctors were
not aware of recommendations on first line anti-hypertensive
agents indicated for IHD patients,
therefore knowledge gaps exist. Some doctors were
hesitant to switch current anti-hypertensive to ACEI/
ARB due to worrying about possible side-effects and
the inconvenience to monitor the renal function after
initiating ACEI or ARB. Furthermore, some patients
refused to change medications as they felt well with
their current regimen, or the BP control was already
optimal even without ACEI or ARB. Doctors were
more confident in initiating ACEI/ ARB following
active staff education and engagement. The set
standard was achieved in
phase 2.
Criterion 11
(seasonal influenza vaccine (SIV) was given or advised)
Only 63 (29.0%) IHD patients received SIV
in phase 1. This is partly explained by the fact that
many patients were still reluctant to receive the SIV
due to a fear of the side effects. In addition, patients
aged below 65 years without social benefit were
not eligible for the free SIV under the government
vaccination program (GVP) before 2018/2019, which
means that many indicated patients have to receive
the SIV out of their own pocket money. Fortunately,
GVP in 2018/19 extended its coverage to include
patients aged 50 or above, with subsidy for
injection in the private sector, and therefore much
more patients could benefit from this new scheme.
Doctors were also more aware of the importance
of flu vaccination and proactively promote it to
indicated patients. With all these facilitating factors,
the SIV coverage was much improved in phase 2
and the set standard was reached. This is consistent
with findings from an audit on secondary preventive
care of IHD in primary care performed in the United
Kingdom, where 67.0% of IHD patients got SIV
after the intervention.20
Criterion 13
(HbA1c <7% if diabetic)
49.3% of diabetic patients reached the
target HbA1c in phase 1. A large proportion of
patients were elderly with other co-morbidities
such as chronic kidney disease, stroke or vision
impairment, which might limit their choice of
oral hypoglycaemic agents and also their ability
to handle insulin injections. Doctors also tend to
accept looser glycaemic control in the elderly in
view of their higher risk of hypoglycaemia. After
educational activities, doctors were more familiar
with the recommended pharmacological agents,
and treatment targets for HbA1c. They were more
motivated to adjust medication to achieve better
cardiovascular risks factor control. 55 (70.5%)
patients achieved satisfactory glycaemic control in
phase 2 following these interventions, which was
slightly better than those achieved via other local
data noted. A local stroke audit reached a standard
of 62% in the second phase.15 The latest DM review
in the HA showed 58.8% and 62.9% of DM patients
in the HA overall and the author’s cluster achieved
HbA1c <7% respectively during the same period.
B.
Criteria that did not meet standard in both
phase 1 and phase 2:
Criteria 12 (BP < 130/80mmHg if hypertensive)
Only 66 (34.0%) hypertensive patients achieved
the target BP control in phase 1, which was
increased to 58.5% in phase 2 (P<0.001). Although
the improvement is prominent, there is still room
for further enhancement when compared with other
local data. For example, hypertensive review in
the HA has revealed a 79.5% achievement rate
of BP below 140/90mmHg among HT patients
during the same period. A local stroke audit aimed
BP <140/90mmHg for hypertensive cases and a
standard of 73% was achieved in the second phase.
Target BP < 130/80mmHg was set for diabetic
patients in the same audit and 61% of patients
had attained this target.15 A hypertension audit in
Malaysia reached 59% of standard in achieving BP
< 140/90 mmHg and < 130/80 mmHg in DM/ renal
impairment.21 Data in Canada showed BP control
rate at 60.1% in DM patients.22
The reasons accountable for this relative
suboptimal performance is multifactorial. On the
one hand, some doctors were not aware of the latest
guidelines on BP management for IHD patients
and therefore still took 140/90 mmHg as the target
BP. In addition, some doctors were concerned
about the risk of hypotension and fall in elderly
patients so they were less stringent on this target.
This is particularly a concern as a high proportion
of IHD patients were of an advanced age with
multiple comorbidities. Indeed, guideline from
American Heart Association suggests that patients
with frequent falls, advanced cognitive impairment
and multiple comorbidities may be at risk of
adverse outcomes with intensive BP lowering.23
An observational study showed an increased risk
of serious fall injury associated with the use of
antihypertensives in older adults, especially those
with a history of fall injury.24 Some patients and
their families also had similar concerns and they
refused to step up anti-hypertensives. HT with
whitecoat effect or whitecoat HT may also be one
of the reasons of not achieving the set standard,
however this was not assessed in this study.
Criterion 14 (LDL <1.8mmol/ L)
Only 40 (18.4%) IHD patients achieved target
LDL control in phase 1. Some doctors were not
aware of the treatment target of LDL level in
IHD patients. Some doctors were not initiating or
adjusting the dose of statin because of therapeutic
inertia, with only 72.4% of patients being put
on statin. Patients’ non-adherence to secondary
prevention treatment may also contribute to the
low LDL control rate. Indeed, several studies have
demonstrated that high levels of non-adherence
of cardiovascular medications exist among IHD
patients.25-27 For example, a meta-analysis revealed
low adherence rate of 54% for statins and 59% for
antihypertensives, in patients with CVD.26 Another
cross-sectional study in United Kingdom showed
rate of non-adherence to at least one secondary
prevention medicine in IHD patients was 43.5%.27
Though the standard was not reached in
phase 2, there was still significant improvement
in the lipid control rate from 18.4% to 58.4%.
Doctors were more knowledgeable on statin use
and they initiated the use of statin earlier apart
from offering advice on lifestyle modification. The
prescription rate of statin increased from 72.4%
in phase 1 to 83.5% in phase 2. However, doctors
expressed concern over the side-effects related to
high intensity statin use in older patients and they
tend to accept looser control with their LDL level.
What’s more, some doctors were less motivated to
intensify treatment when patients’ LDL level was
close to target. These doctors’ behavioural patterns
were well demonstrated in some local studies.
A local retrospective analysis in 2003 revealed
significantly lower prescription rate of lipid
lowering agents in patients aged 90 or above28,
while another study showed that therapeutic inertia
was common in the management of patients with
known CVD and a closer-to-normal LDL level.29
C.
Criteria that met the standard in both phase 1 and phase 2:
Criteria 6
(BP recorded) and Criterion 9 (antiplatelet agents given)
More than 90% of patients had BP recorded
in every routine visit. After review of consultation
notes and interview with doctors involved, we
found that some were missed due to patients’
refusal or busy consultation. These data
demonstrated that almost all primary care doctors
were well aware of the importance of regular BP
monitoring and the use of antiplatelet therapy in
the secondary prevention of patients with IHD.
Limitations of the audit
Firstly, as the study was conducted in public
primary care clinics of the HA, selection bias might
exist. The results from this study may not be applicable
to the secondary care setting or the private sector.
Nevertheless, these data should realistically represent
the IHD care in public primary care settings and provide
groundwork for future service enhancement. Secondly,
as the subject inclusion relied highly on the proper ICPC
coding and CMS documentation, patients not properly
coded or miscoded would be missed. The result may not
reveal the real clinical situation if the clinical assessment
were poorly documented in the CMS. Thirdly, some
factors that might affect patients’ cardiovascular
outcome were not assessed in this audit. For instance,
patients’ drug compliance, dietary habit and use of
allied health service etc. were not included in the data
analysis. Lastly, only short-term outcomes were assessed
in this audit and long-term outcome parameters like IHD
recurrence rate and mortality rate were not evaluated. In
addition, the relatively short implementation phase (12
months) might not be long enough for some criteria to
achieve the target standard.
Conclusion
Ischaemic heart disease is a common and important
disease worldwide and it causes significant morbidity
and mortality. Optimal control of CVD risk factors and
use of anti-platelet agents, statins and ACEIs or ARBs
are proven to be effective in reducing CVD related
morbidity and mortality. This clinical audit showed
significant improvement in both the process of care and
outcome of secondary preventive care among patients
with IHD managed in primary care. Future audit
focusing on the long-term outcomes such as recurrent
cardiac events and CVD related mortality should be
performed for better evaluation on the quality of care
provided to patients with IHD.
Acknowledgement
We would like to thank all medical and nursing
staff of the Department of Family Medicine & GOPCs,
Kowloon Central Cluster of the HA for their unfailing
effort and support to this clinical audit.
References
-
Top 10 causes of death [Internet]. [cited 2019Aug1]. Available from: https://
www.who.int/gho/mortality_burden_disease/causes_death/top_10/en/
-
Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke
statistics - 2018 update: A report from the American Heart Association. Vol.
137, Circulation. 2018. 67–492.
-
Nichols M, Townsend N, Scarborough P, et al. Cardiovascular disease
in Europe 2014: epidemiological update. European heart journal.
2014;35(42):2950-2959.
-
Hospital Authority Strategic Service Framework for coronary heart disease
[Internet]. [cited 2019Aug2]. Available from: http://www.ha.org.hk/ho/
corpcomm/Strategic%20Service%20Framework/Coronary%20Heart%20
Disease.pdf
-
Major Causes of Death [Internet]. [cited 2019Jul27]. Available from: https://
www.healthyhk.gov.hk/phisweb/en/healthy_facts/disease_burden/major_
causes_death/
-
A Matter of Your Heart: Coronary Heart Disease. [Internet]. [cited
2019Aug2]. Available from: https://www.chp.gov.hk/files/pdf/ncd_watch_
jul2015.pdf
-
Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/
SCAI/STS Guideline for the Diagnosis and Management of Patients With
Stable Ischemic Heart Disease. Circulation. 2012;126(25).
-
El-Jack S, Kerr A. Secondary prevention in coronary artery disease patients
in South Auckland: moving targets and the current treatment gap [Internet].
The New Zealand medical journal. U.S. National Library of Medicine;
2003 [cited 2019Aug11]. Available from: https://www.ncbi.nlm.nih.gov/
pubmed/14615806
-
Gamboa C, Safford M, Levitan E, et al. Statin Underuse and Low Prevalence
of LDL-C Control Among U.S. Adults at High Risk of Coronary Heart
Disease. The American Journal of the Medical Sciences. 2014;348(2):108-114.
-
Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS Guidelines for the
Management of Dyslipidaemias. European Heart Journal. 2016;37(39):2999-3058.
-
Smith SC, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary
prevention and risk reduction therapy for patients with coronary and other
atherosclerotic vascular disease: 2011 update: a guideline from the American
Heart Association and American College of Cardiology Foundation
endorsed by the World Heart Federation and the Preventive Cardiovascular
Nurses Association. Journal of the American college of cardiology.
2011;58(23):2432-2446.
-
Primary Care Office. Clinical Audit – Examples on Diabetes and
Hypertension Audit Making Use of the Reference Frameworks. [Internet]
Hong Kong; 2015. [cited 2019Jul29]. Available from: https://www.fhb.gov.
hk/pho/rfs/english/pdf_viewer.html?file=download67&title=string82&titletext
=string53&htmltext=string53&resources=12_en_Clinical_Audit
-
Primary Care Office. Hong Kong Reference Framework for Diabetes Care
for Adults in Primary Care Settings. [Internet]. Hong Kong; 2015. [cited
2019Aug4]. Available from: https://www.pco.gov.hk/english/resource/files/e_
diabetes_care_patient.pdf
-
Choi Y, Han J, Li R, et al. Implementation of secondary stroke prevention protocol
for ischaemic stroke patients in primary care. Hong Kong Medical Journal. 2015.
-
Chen CX, Chan SL, Law TC, et al. Secondary prevention of stroke: an
evidence-based clinical audit in the primary care. Hong Kong Medical
Journal. 2011 Dec;17(6): 469-477.
-
Braun MM, Stevens WA, Barstow CH. Stable coronary artery disease:
Treatment. American Family Physician. 2018;97(6):376–384.
-
Urbaniak, G. C., & Plous, S. (2013). Research Randomizer (Version 4.0)
[Computer software]. Retrieved on June 22, 2013, from http://www.randomizer.org/
-
Wong KW, Ho SY, Chao DV. Quality of diabetes care in public primary care
clinics in Hong Kong. Family Practice. 2012 Apr;29(2):196-202.
-
Cheung BMY, Cheng CH, Lau CP, et al. 2016 consensus statement on
prevention of atherosclerotic cardiovascular disease in the Hong Kong
Population. Hong Kong Medical Journal. 2017;:191–201.
-
Dunkley A, Stone M, Squire I, et al. An audit of secondary prevention of
coronary heart disease in post acute myocardial infarction patients in primary
care. Quality in Primary Care. 2006;14(1).
-
Chan SC, Chandramani T, Chen TY, et al. Audit of hypertension in general
practice. The Medical journal of Malaysia. 2005 Oct; 60(4):475-482.
-
Padwal RS, Bienek A, Mcalister FA, et al. Epidemiology of Hypertension in
Canada: AnUpdate. Canadian Journal of Cardiology. 2016;32(5):687–694.
-
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/
ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention,
Detection, Evaluation, and Management of High Blood Pressure in Adults.
Journal of the American College of Cardiology. 2018;71(19):e127.
-
Tinetti ME, Han L, Lee DSH, et al. Antihypertensive Medications and
Serious Fall Injuries in a Nationally Representative Sample of Older Adults.
JAMA Internal Medicine. 2014Jan;174(4):588.
-
Kolandaivelu K, Leiden BB, Ogara PT, et al. Non-adherence to cardiovascular
medications. European Heart Journal. 2014;35(46):3267–3276.
-
Chowdhury R, Khan H, Heydon E, et al. Adherence to cardiovascular
therapy: a metaanalysis of prevalence and clinical consequences. European
Heart Journal. 2013Jan;34(38):2940–2948.
-
Khatib R, Marshall K, Silcock J, et al. Adherence to coronary artery disease
secondary prevention medicines: exploring modifiable barriers. Open Heart.
2019;6(2).
-
Kung K, Lam A, Li KT. The use and efficacy of statins in Hong Kong
Chinese dyslipidaemic patients in a primary care setting. The Hong Kong
Practitioner. 2005;27:450-454.
-
Man FY, Chen CX, Lau YY, et al. Therapeutic inertia in the management
of hyperlipidaemia in type 2 diabetic patients: a cross-sectional study in the
primary care setting. Hong Kong Medical Journal. 2016 Aug;22(4):356-364.
Yin-mei Liu,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Resident Specialist,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority Hong Kong
Chi-hang Lau,
MBChB (CUHK), FHKCFP, FRACGP, FHKAM (Family Medicine)
Private practitioner,
Catherine XR Chen,
MRCP (UK), PhD (Med, HKU), FRACGP, FHKAM (Family Medicine)
Consultant,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority Hong Kong
Yim-chu Li,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Chief of Service,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority, Hong Kong.
Correspondence to:
Dr. Liu Yin Mei, KCC FM & GOPC Department Office. Rm 622,
Nursing Quarter, Queen Elizabeth Hospital, 30 Gascoigne Road,
Kowloon, Hong Kong SAR.
E-mail: lym873@ha.org.hk
|
