Smoking cessation during the COVID-19
epidemic ‒ A new mode of intervention
Raymond KS Ho 何健生,Helen CH Chan 陳靜嫻,Grace NT Wong 黃雅婷,Patrick WY Fok 霍偉賢
HK Pract 2022;44:116-124
Summary
Objective:
The objectives of this study were: (1) to
study the feasibility of “mail to quit” smoking service
delivery and its efficacy; (2) to collect the views of
the participants; and (3) to evaluate the impact of the
service on the participants.
Design:
Prospective cohort study.
Subjects:
Eligible smokers recruited from 1st December
2020 to 31st January 2021 were recommended to use
the “mail to quit” service.
Main outcome measures:
The outcome measures were:
quit rate at 26th week, participants’ satisfaction score and
opinion score on the “mail to quit” service. A pre-test and
post-test questionnaire on project impact was adopted
from Donald Kirkpatrick’s four levels of evaluation.
Results:
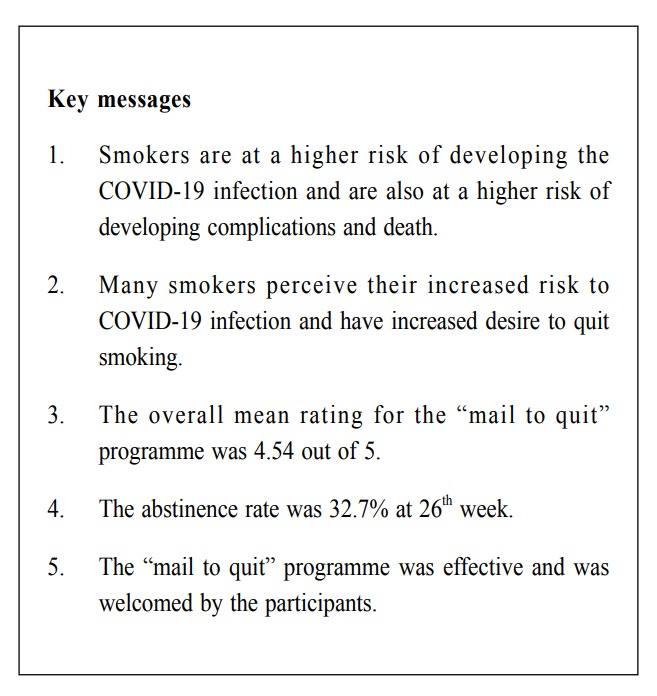
161 out of 215 smokers responded to our
survey, yielding a response rate of 74.88%. In the
area of impact assessment, self-perceived health, life
satisfaction score, knowledge gained, skill learned on
use of distraction method, buying cigarettes all showed
statistically significant improvement. The abstinence
rate was 32.7% at 26th week. The overall mean rating
for the “mail to quit” programme was 4.54 (SD 0.69).
Conclusions:
The “mail to quit” programme with
remote counselling during the COVID-19 pandemic was
a feasible and effective means to provide “smoking
cessation” intervention for smokers. It was well received
by smokers and had significant impact on their smoking
behaviour and knowledge gain.
摘要
目的 :
本研究的目標是:(1)研究“郵件戒煙”服務的可行性及有效性;(2)收集參與者的意見;以及(3)評估該服務。
設計 :
前瞻性群組研究
對象 :
招募從2020年12月1日至2021年1月31日符合條件的吸煙者使用“郵件戒煙”服務。
主要結果衡量標準 :
結果衡量標準是:第26周的戒煙率,參與者的滿意度得分和“郵件戒煙”服務的意見評分。關於專案測試前和測試後的影響,問卷採納了唐納德·柯克帕特里克的四個級別評估。
結果 :
215名吸煙者中有161人回覆了我們的調查,回覆率為74.88%。在影響評估、自我健康的認知、生活滿意度評分、獲得的知識、使用分心方法的技能、購買香煙都顯示出統計學上的顯著改善。第26周的戒煙率為32.7%。“郵件戒煙”計劃的總體平均評級為4.54(SD 0.69)。
結論 :
在新冠肺炎大流行期間,帶有遠端諮詢的“郵件戒煙”計劃為吸煙者提供了“戒煙”干預的可行性和有效性的手段。它深受吸煙者的歡迎,並對他們的吸煙行為和知識獲取產生了重大的影響。
Introduction
COVID-19 is a coronavirus outbreak that initially
appeared in December 2019 and it has then evolved
into a pandemic spreading rapidly worldwide.1 As of
17 April 2022, over 500 million confirmed cases and
over 6 million deaths have been reported globally as
reviewed by the WHO. This disease mainly affects
the lungs. Smokers are at a higher risk of developing
COVID-19 and are also at a higher risk of developing
severe COVID-19 complications and deaths.2 Smokers
may be at an increased risk of contracting the virus
due to reduced lung function, impaired immune
systems and cross-infection. Cigarette smoking also
increases the amount of forced vital capacity (FVC) and
stimulates hyperproliferation of the bronchial mucosal
glands, resulting in increased mucosal permeability,
excessive mucus production and inhibited clearance of
mucosal cilia, reducing the airway purification function
and harmful microorganism screening in the upper
respiratory system, leading to potential pulmonary
inflammation.3 A recent meta-analysis revealed that
current smoking increases the risk of severe COVID-19
infection by around twofold.4 Studies also suggested
that even 4 weeks of smoking cessation may decrease
the risk of adverse outcomes and respiratory failure
associated with COVID-19 infection.5
During this pandemic, the fear of contracting a
potentially fatal disease, confinement, the possibility of
being laid off and the stress from financial problems,
could increase the desire to smoke. However, smokers
may also perceive their increased risk to COVID-19
infection and its complications, hence may also increase
their desire to quit smoking.6
The need to remove the protective mask while
smoking can facilitate viral transmission. Some
governments have imposed a mandatory mask law, and
this can make smoking very inconvenient. In Hong
Kong, the SAR government had imposed a mandatory
mask law to curb the spread of COVID-19 infection.
In fact, some smokers had been fined because they
took off their masks to smoke in public. Hence the
COVID-19 pandemic presents a unique opportunity for
smoking cessation. In a survey by Elling et al, one-third
of the smokers were more motivated to quit smoking
due to the coronavirus.7
Tung Wah Group of Hospitals Integrated Centre on
Smoking Cessation (TWGHs ICSC) is a community-based
smoking cessation service funded by the Hong
Kong SAR Government. There are five centres in
our New Territories, and they provide free smoking
cessation services which include counselling and
pharmacotherapy to Hong Kong citizens. Counselling
is performed by experienced social workers who have
been trained in smoking cessation.
In view of the need for social distancing, staying at
home as much as possible and the potential increase in
smoking cessation demand, we initiated a “mail to quit”
programme offering the mailing of nicotine replacement
therapy (NRT) and phone or online counselling.
In the late 1990s, the International Society for
Mental Health Online (ISMHO) had already promoted
the use of online technologies amongst mental health
professionals. In 2001 comprehensive guidelines
were developed in the UK by the British Association
for Counselling and Psychotherapy (Goss et al.,
2001).8 Online counselling has numerous advantages.
It overcomes the need for travelling, enabling
psychological assistance and intervention without face-to-face contact. It is specifically beneficial for those
living in geographically remote areas. The visual
anonymity associated with telephone counselling can
decrease anxiety for the participants. They may be less
defensive and more willing to share their feelings and
difficulties.9,10 Reese et al. had studied the attractiveness
and client perception of telephone counselling in 2006
and gave a similar conclusion.11
Objective
The objectives of this study were:
-
to study the feasibility of this mode of service
delivery and its efficacy
-
to collect the views of the participants
-
to evaluate the impact of the service on the
participants
Methods
Study population
A prospective study was carried out to recruit
smokers to use the “mail to quit” services from 1st
December 2020 to 31st January 2021. The recruitment
part were smokers self-referred to smoking cessation
centres via telephone or QR code from advertisement
in Facebook, mini-buses, mobile truck in smoking hotspots
and smoking cessation hotlines operated by the
Department of Health. Participants could enrol in the
cessation services via telephone contact or QR code.
For those who used the QR code method, they would be
directed to a Google form so that they could fill in their
particulars, their smoking habits, and their preferred
time for future contacts by our counsellors. No personal
ID number was collected in the Google form and each
participant was assigned a clinic reference number
for identification. Participants should be able to read
and speak Chinese. Those who were aged less than 18
or above 60, allergic to nicotine replacement therapy
(NRT); had chronic medical or mental illness; recent
hospitalisation in the past six months, being pregnant or
practicing breast feeding and had contraindications for
the use of NRT were excluded. We limited participants
to these stringent criteria because it was a pilot study,
and we would like to play safe from the start. There
were multiple routes of recruitment because we would
like to recruit as many participants as far as possible.
Besides, we had to meet a performance pledge to
the Department of Health of HKSAR as there was a
significant drop in clinic visits due to the need for
social distancing.
Smoking cessation intervention
All eligible service users were invited to join the
study. A verbal consent for the study was explained
and obtained by counsellors over the phone at the first
intake. Information on the participants’ demographics,
smoking habits, past medical history were recorded.
Copies of consent forms were then mailed to the
participants, who were required to sign and return
the consent form to the investigators. After initial
assessment through the phone, two weeks supply of
the NRT were sent by mail to the eligible participants.
A phone call was made several days later to ascertain
the receipt of the NRT. Counselling, motivational
interviewing and cognitive behavioural therapy
were then given by remote counselling via phone or
communication software (WhatsApp or WeChat) about
twice weekly until the end of treatment which lasted
from 8 to 12 weeks. The mailing package included:
-
instructions for the use of NRT,
-
a briefing on the principle and use of NRT for
smoking cessation; the preparation needed and
ways to deal with craving,
-
NRT patch, gum or lozenges, depending on the
clinical conditions.
A guideline on the use of remote consultation as
adapted from the UK National Health Service (NHS)
2020 National Centre for Smoking Cessation and
Training was issued to all counsellors to follow.12 All
interventions and counselling sessions were similar
to our conventional method of smoking cessation
programme.
All those reported to have adverse reactions were
assessed by counsellors and referrals to our clinic
doctor were arranged when necessary.
Outcome measures
A questionnaire on the impact of the current
programme, adopted from Donald Kirkpatrick’s
framework (knowledge, skill, attitude, behavioural change,
self-rated life satisfaction, self-rate health, self-rated job
satisfaction and self-rated family life satisfaction) was
carried out before and at the end of treatment, (Pre-test
and Post-test).12 The outcome measures were quit rate
at 26th week, participants’ satisfaction rating and their
opinion on the “mail to quit” service.
The quit rate was defined as 7-day point prevalence
abstinence and those who could not be contacted or
defaulted would be considered as not quit based on
the intention to treat principle. In view of the online
consultation, no biochemical validation of abstinence
was performed.
Statistical analysis
Descriptive statistics were used for basic
demographics. Continuous variables were expressed as
mean ± standard deviation (SD). Categorical variables
were presented as numbers and percentages. McNemar’s
Chi square test, paired t-test and Fisher’s exact test were
used for pre- and post- intervention analysis of variables.
Results
Sample characteristics
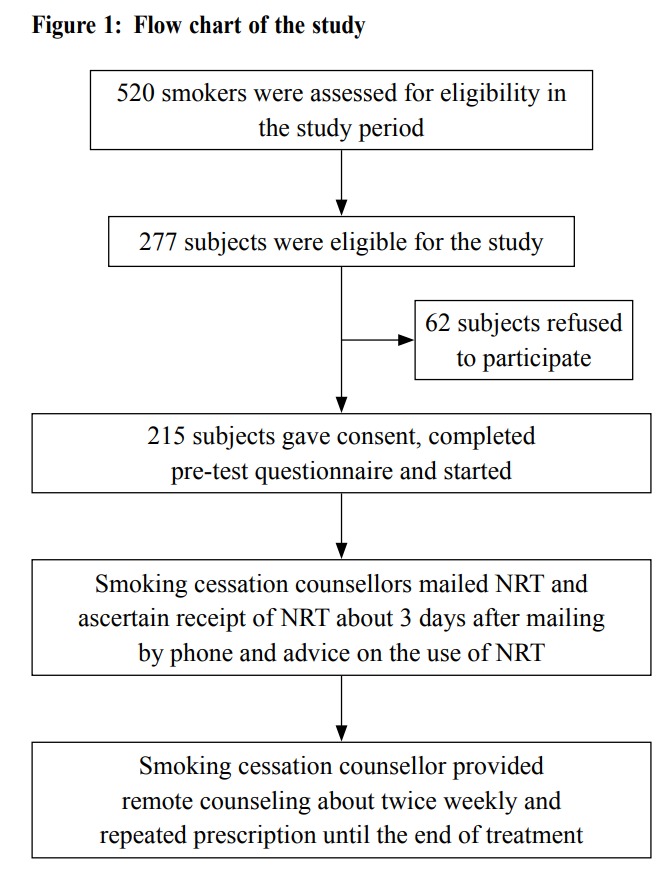
During the first intake, 215 subjects consented
to participate in the study (Figure 1). At the end
of treatment, 161 subjects responded to our survey,
yielding a response rate of 74.88%. The characteristics
of 215 and 161 participants were listed in Table 1.
More than 57% were in the age of 26 to 40 with a male
predominance. More than half of them were married
and more than 77% were employed. Most of them had
previous quit attempts, and about 56% lived in the
New Territories, a relatively remote area from the town
centre.
Impact assessment
Since only 161 subjects responded to our survey,
we limited this group to undergo pre- and post-treatment
analysis on the impact assessment and
their opinion on the “mail to quit” programme. In the
area of impact assessment, self-perceived health, life
satisfaction score, knowledge gained, skill learned on
the use of distraction method, buying cigarettes all
showed statistically significant improvement (Table 2).
There was no significant change in family relationship
and work efficiency.
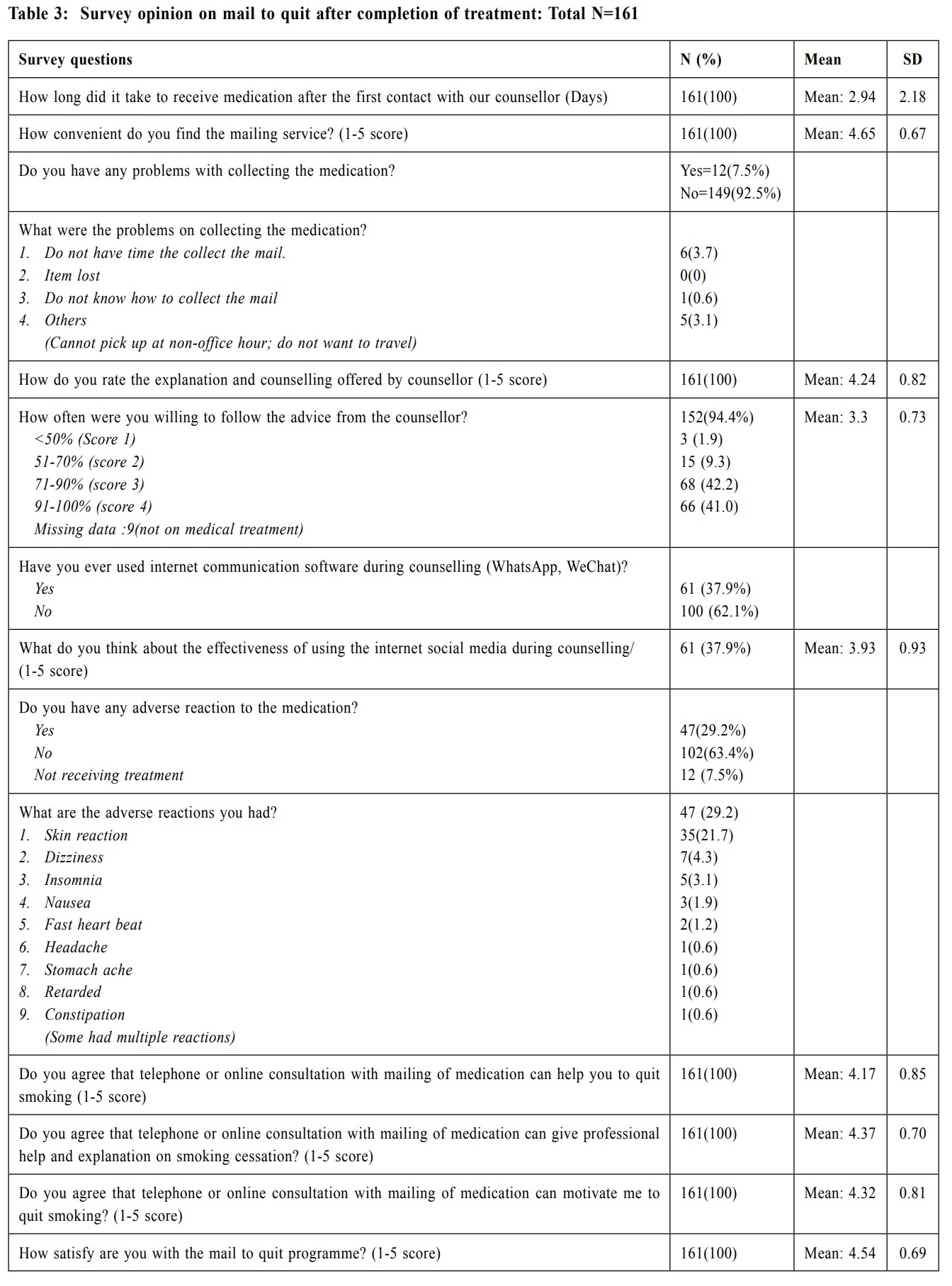
Opinion survey and abstinence rate
In the opinion survey, the mean score on the
convenience of “mail to quit” programme was 4.65 out
of 5 and this might be considered as remarkably high.
92.54% of participants did not have any problem in
collecting medication (Table 3). On average it took 2.94
days to secure the medication. 29.2% reported some
adverse reactions from NRT. This was similar to NRT
dispensed by conventional methods. All of the adverse
reactions were minor such as allergic dermatitis, and no
major adverse event was reported. The mean rating on
the explanation and counselling offered by counsellor
was 4.24 out of 5, and mean rating on the use of
social media for counselling service was 3.93 out of 5.
The mean rating on professional help and motivation
on smoking cessation were also high, 4.37 and 4.32
respectively. The overall mean rating for the “mail to
quit” programme was 4.54 out of 5 (SD 0.69).
There were 215 participants joining our treatment
programme initially and one withdrew later. due to
personal inconvenience. 70 participants reported total
abstinence (7-day point prevalence) at 26th week,
yielding a quit rate of 32.7%.
Discussion
Since the beginning of the COVID-19 pandemic
in February 2020 in Hong Kong, there was a dramatic
decrease number of smokers seeking smoking cessation
via our service in view of the need for social distancing
and fear of contracting the disease, despite a potential
increase in the need of smoking cessation from the
smokers. This pandemic provided us with an opportunity
to review our service and to modify our mode of service
delivery to meet the social distancing requirements. The
use of remote counselling together with mailing of NRT
was thought to be a useful alternative.
In our study, there was significant impact in terms
of self-rated health, life satisfaction score, knowledge
gain, skill and attitude change and behavioural
improvement. There were numerous studies on the
health impact and cost effectiveness of smoking
cessation programmes. However, we were not aware of
any study, either locally or overseas, on the impact of
a smoking cessation programme similar to our “mail to
quit” during the COVID-19 pandemic.
In the survey opinion with this programme, the
overall rating from the participants should be considered
as remarkably high. There was no excessive delay in
collecting the mail and more than 90% of participants
did not have any difficulty in getting the medication.
As to online counselling or telephone counselling, most
of them considered it to be effective, helpful, and able
to serve its purpose, and our counsellors were able to
motivate them to quit smoking. One point worth noting
is that the score on telephone counselling was higher
than counselling via communication software.
On the area of telephone counselling, a study
by An LC. et al. indicated that the telephone care
increased the use of behavioural and pharmacologic
assistance and led to higher smoking cessation rates,
compared to routine health care provider intervention.14
A meta-analysis review by Lichtenstein et al also
indicated that there was a significant increase in
cessation rates by proactive telephone calls compared
to control conditions.15 The abstinence rate at the 26th
week of the current study was 32.7% and this was
comparable to a study by Macleod et al16 who used
telephone counselling as an adjunct to nicotine patches
in smoking cessation and reported a quit rate of 30.7%
at 6 months. However, the methodology of this study
was totally different from ours. According to overseas
experience, the average abstinence rate at 26th week was
20-25%. On the other hand, our abstinence rate at 26th
week with conventional method over the past five years
was around 43%. This implied that the ‘’mail to quit’’
programme should be considered satisfactory, although
it was lower than our conventional method. This could
possibly be due to the fact that face-to-face counselling
was used in conventional method.
In our study, the ‘’mail to quit’’ service was carried
out via one-to-one communication rather than ‘’open’’
messaging, public sharing of information or group
counselling. We mailed NRT to the participants without
urging them to come to our clinics. This could save
their opportunity cost on travelling and time spent. This
was much welcomed by the participants as seen from
the result of this study. As to the efficacy of mailing of
NRT, a study by Cunningham et al has provided evidence
of the effectiveness of mailed nicotine patches without
behavioural support to promote tobacco cessation.17
Self-reported abstinence rates were significantly higher
among participants who were sent nicotine patches
compared with the control group (odds ratio, 2.65; 95%
CI, 1.44-4.89). In our study, we have not isolated the
effect of mailing NRT alone, although the combined
effect of remote counselling and mailing of NRT was
remarkable. Based on overseas and the present study,
the future of remote counselling on smoking cessation
appears favourable and effective.18,19
The users of remote counselling sampled in this
study found it appealing and attractive. It is particularly
convenient to those who have to work shift duties or
unconventional office hours, or those who cannot afford
to come to the clinics. The enrolment by QR code and
Google form can be conducted 24 hours a day, hence
making enrolment much easier. However, counselling
via telephone or communication software may not be
best for clients who prefer to see their therapist and for
clients who were experiencing severe problems such
as unstable mental condition. Another downside of
telephone consultation is that we could not detect any
non-verbal cues from the participants, their attention
span or their understanding during the consultation. In
real practice, some participants may be distracted by
something else during the consultation process. In the
present study, we have also excluded old- age clients,
clients with chronic medical illness and mental disease
to avoid risk and complications.
Limitations
There were a few limitations in this study. This is
an observational study on smokers who were relatively
healthy. They did not have any chronic medical
conditions or mental illness. They were adult smokers
who were aged 60 or below. Therefore, the result cannot
be extended to the whole smoking population. There
was no control group to compare with the effectiveness
of this mode of intervention and there were no
benchmarks for the scores. There are many facets of
impact assessment and we only limited it to the Donald
Kirkpatrick’s four levels of evaluation.20,21,22 Our survey
questionnaire was self-devised with reference from
Donald Kirkpatrick’s method, hence there was no gold
standard. The quit rate is self-reported abstinence and
there is no biochemical validation, although consensus
statements indicate that biochemical validation of tobacco
cessation may not be required in the present study.23
Conclusion
In conclusion, the “mail to quit” programme with
remote counselling during the COVID-19 pandemic
is a feasible and effective means to provide smoking
cessation intervention for smokers without chronic
medical illness with a satisfactory abstinence rate. It is
feasible in terms of administrative procedure, solving
technical issues and setting up guideline for remote
consultation and smoker’s acceptance. It reduces the
risk of social contacts and social exposure during
travelling, hence reducing the risk of contracting the
virus. There is significant impact on the participants,
both in terms of quitting, behavioural change, and
knowledge gain. The programme is perceived to be
very convenient, helpful and useful and is well received
by the smokers. A further large scale control study is
worthwhile to validate our findings.
Ethical approval and consent from participants
This study was approved by the Research Ethics
Committee of the Tung Wah Groups of Hospitals (No.
R2021007). Written informed consent was obtained from
all participants prior to their enrolment in the study.
Funding
There is no special funding source for this study.
The smoking cessation service was funded by the
Department of Health HKSAR Government.
Potential competing interest
Nil declared.
Acknowledgement
We thank all staff involved in this project.
References
-
Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential
domestic and international spread of the 2019-nCoV outbreak originating
in Wuhan, China: a modelling study. Lancet. 2020;395(10225): 689-697.
doi:10.1016/S0140-6736(20)30260-9.
-
Vardavas CI, Nikitara K. COVID-19 and smoking: a systematic review of
the evidence. Tob Induc Dis. 2020;18(3):20. doi: 10.18332/tid/119324.
-
Xie J, Zhong R, Wang W, et al. COVID-19 and Smoking: What Evidence
Needs Our Attention?. Front Physiol. 2021;12:603850. doi:10.3389/
fphys.2021.603850
-
Zhao Q, Meng M, Kumar R, et al. The impact of COPD and smoking
history on the severity of Covid-19: A systemic review and meta-analysis. J
Med Virol. 2020;1-7. doi:10.1002/jmv.2588.
-
Eisenber SH, Eisenberg MJ. Smoking Cessation During the COVID-19
Epidemic. Nicotine & Tobacco Research. 2020; 22(9): 1664-1665. https://
doi.org/10.1093/ntr/ntaa075
-
Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect:
correlation, causation, and context across stages of smoking. Psychol Bull.
2003;129(2):270-304. doi:10.1037/0033-2909.129.2.270
-
Elling JM, Crutzen R, Talhout R, et al. Tobacco smoking and smoking
cessation in times of COVID-19. Tobacco prevention & cessation. 2020; 6:39.
https://doi.org/10.18332/tpc/122753
-
Goss S., Anthony K., Jamieson A, et al. Guidelines for Online Counselling
and Psychotherapy. Rugby: BACP. 2001.
-
Chester A, Glass GA. Online counselling: A descriptive analysis of therapy
services on the Internet. British Journal of Guidance & Counselling. 2006;
34(2): 145-160. doi : 10.1080/03069880600583170
-
Wellman B. “An electronic group is virtually a social network.” Culture of
the Internet. 1997;4:179-205.
-
Reese RJ, Conoley CW, Brossart DF. The Attractiveness of Telephone
Counseling: An Empirical Investigation of Client Perceptions. Journal of
Counseling & Development. 2006; (84):54-60.
-
Montgomery S and Papadakis S. Remote consultations: Delivering
behavioural support and supply of NRT. 2020 National Centre for Smoking
Cessation and Training About the National Centre for Smoking Cessation.
https://www.ncsct.co.uk/usr/pub/Remote%20consultations.pdf
-
Praslova L. Adaptation of Kirkpatrick’s four level model of training criteria
to assessment of learning outcomes and program evaluation in Higher
Education. Educ Asse Eval Acc. 2012;22:15–225. https://doi.org/10.1007/
s11092-010-90987
-
An LC, Zhu SH, Nelson DB, et al. Benefits of Telephone Care Over Primary
Care for Smoking Cessation A Randomized Trial. Arch Intern Med. 2006;
166:536-542.
-
Lichtenstein E, Glasgow RE. Telephone counseling for smoking cessation:
rationales and meta-analytic review of evidence. Health Education and
Research Theory & Practice. 1996; 11(2): 243-257.
-
Macleod ZR, Arnaldi VC, Adams IM, et al. Telephone counselling as an
adjunct to nicotine patches in smoking cessation: a randomized controlled
trial. Medical Journal of Australia. 2003;179(7):349–352. doi:10.5694/
j.13265377.2003.tb05590
-
Cunningham JA, Kushnir V, Selby P, et al. Effect of Mailing Nicotine
Patches on Tobacco Cessation Among Adult Smokers. A Randomized
Clinical Trial. JAMA Intern Med. 2016;176(2):184-190. doi:10.1001/
jamainternmed.2015.7792
-
Mermelstein R, Hedeker D, Wong SC, et al. Extended telephone counseling
for smoking cessation: Does content matter? Journal of Consulting and
Clinical Psychology. 2003; 71: 565–574.
-
Lynch DJ, Tamburrino MB, Nagel R, et al. Telephone counseling for patients
with minor depression: Preliminary findings in a family practice setting. The
Journal of Family Practice. 1997;44;293–298.
-
Reno JP. Managing for Service Effectiveness in Social Welfare
Organizations. Social work. 1987;32(5):377–381. https://doi.org/10.1093/
sw/32.5.377
-
Vanclay F, Esteves AN, Aucamp I, et al. Social Impact Assessment:
Guidance for assessing and managing the social impacts of projects.
International Association for Impact Assessment. 2015.
-
Lee EKM, Lee H, Kee CH, et al. Social Impact Measurement in Incremental
Social Innovation. Journal of Social Entrepreneurship. 2019;12(1):69-86.
doi: 10.1080/19420676.2019.1668830
-
SRNT Subcommittee on Biochemical Verification. Biochemical verification
of tobacco use and cessation. Nicotine Tob Res. 2002;4(2):149-159.
Raymond KS Ho,
MRCP (UK), FHKAM (Family Medicine), FHKAM (Medicine)
Medical officer,
Tung Wah Group of Hospitals, Integrated Centre on Smoking Cessation
Helen CH Chan,
BSW, M.Soc.Sc. MPH
Supervisor,
Tung Wah Group of Hospitals, Integrated Centre on Smoking Cessation
Grace NT Wong,
RSW, BSW
Counsellor,
Tung Wah Group of Hospitals, Integrated Centre on Smoking Cessation
Patrick WY Fok,
RSW, BSW
Assistant Supervisor,
Tung Wah Group of Hospitals, Integrated Centre on Smoking Cessation
Correspondence to:
Dr. Raymond KS Ho, 10/F Tung Chiu Commercial Centre,
193-197 Lockhart Road, Wanchai, Hong Kong SAR.
E-mail: kinsang.ho@tungwah.org.hk
|
