Application of ambulatory blood pressure
monitoring in public primary care clinics in
Hong Kong: what do primary care doctors
need to know?
Kwai-sheung Wong 黃桂嫦,Ka-ming Ho 何家銘,Yim-chu Li 李艷珠,Catherine XR Chen 陳曉瑞
HK Pract 2022;44:81-89
Summary
Objective:
To delineate the indications for ordering
ambulatory blood pressure monitoring (ABPM) in
public primary care setting and to explore patient
characteristics and results of the ABPM.
Design:
Cross-sectional descriptive study.
Subjects:
All patients who have had ABPM performed
from 1/12/2016 to 30/11/2017 in five General Outpatient
Clinics.
Main outcome measures:
The indications for
performing the ABPM, demographics of patients
undergoing ABPM and the results of ABPM were
studied.
Results:
There were 323 patients with ABPM done
within the study period with valid results. 64% were
female and 36% were male, and the average age was
64 ± 12 (19 to 94 years old). 67 (21%) with diabetes
mellitus and 53 (16%) with impaired glucose tolerance
or impaired fasting glucose.
For the indications for ABPM, 150 (46%) were
for establishing diagnosis of hypertension (HT) and
173 (54%) were for monitoring of blood pressure (BP)
control among hypertensive patients.
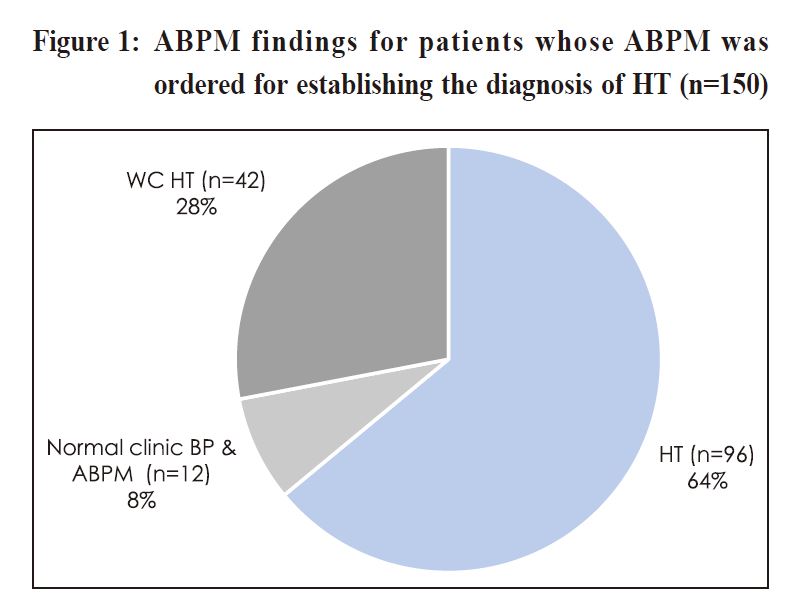
Among the diagnosis of HT group, 96 (64%) were
confirmed with the diagnosis of HT, 42 (28%) were
found to have white-coat HT only.
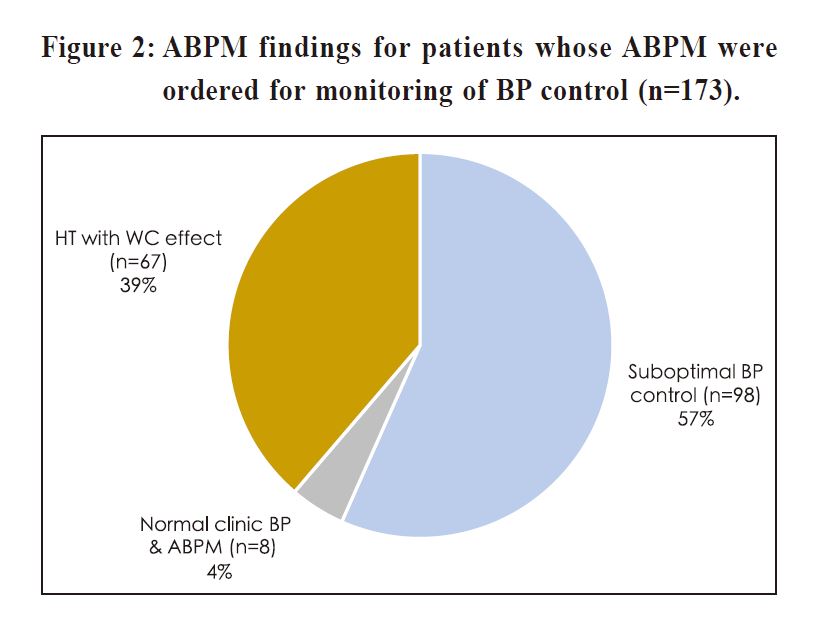
For the monitoring of BP control group among HT
patients, 98 (57%) were noted to have suboptimal BP
control and 67 (39%) were found to have white-coat effect.
Among the 65 patients whose ABPM had been
ordered although their clinic BPs being normal, 18 (28%)
were diagnosed to have masked HT and 19 (29%) were
diagnosed to have masked uncontrolled HT.
Conclusions:
ABPM greatly helped the diagnosis and
management of different types of HT in primary care.
Keywords:
Ambulatory blood pressure monitoring,
hypertension, primary health care
摘要
目的 :
規劃在公共基層醫療環境中24小時動態血壓監測
(ABPM)的用途,並探索24小時動態血壓監測病人的特徵
和結果。
設計 :
橫斷面式描述性研究。
對象 :
從2016年12月1日至2017年11月30日期間,所有在
五個普通科門診診所進行了24小時動態血壓監察的病人。
主要結果測量 :
研究了進行廿四小時動態血壓監察
的原因、病人的人口統計學特徵及結果。
結果 :
在研究期間,有323位進行了廿四小時動態血
壓監察的病人的結果為有效。64%為女性,36%為男
性,平均年齡為64±12歲(19至94歲。67人(21%)患有
糖尿病,53人(16%)患上葡萄糖耐性障礙或空腹血糖
偏高。
至於進行二十四小時動態血壓監察的原因,150名
病人(46%)用於確定高血壓(HT)的診斷,173名病人
(54%)用於監測高血壓患者的血壓(BP)控制。
關於血壓高的的診斷中,96名病人(64%)被診斷為血
壓高,42(28%)被發現只有白袍高血壓。
關於血壓高病人的控制監察方面,98名病人(57%)的
血壓控制不理想,而67名病人(39%)被發現具有白袍
效應。
儘管診所血壓正常,但仍然進行二十四小時動態血
壓監察的65名患者中,18名(28%)被診斷出患有隱性
高血壓,19名(29%)被診斷出患有不受控制的隱性高血壓。
結論 :
廿四小時動態血壓監察有效地幫助了不同種類
高血壓的診斷和治療。
關鍵詞 :
廿四小時動態血壓監測、高血壓、基層醫療
Introduction
Hypertension (HT) is a common chronic disease
affecting more than 20% of adults globally1 and more
than 27% of Hong Kong (HK) people aged 15-84.2 It
is also one of the most common clinical conditions
encountered in primary care. Numerous studies have
shown that HT is one of the major cardiovascular risk
factors.3,4 For every 10 mmHg reduction in systolic
blood pressure (BP), the risk of major cardiovascular
disease events reduced significantly by 20%, leading
to a significant 13% reduction in all-cause mortality.5
Therefore, proper diagnosis and management of HT is
an important mission for primary care doctors.
Traditionally, HT is diagnosed based on office
or clinic BP readings. Recent studies have revealed
that ambulatory blood pressure monitoring (ABPM)
could provide better prognostic information about
cardiovascular disease than office BP measurement.6,7
As ABPM can provide multiple BP measurements
away from the medical environment, it gives a clearer
picture of the patient’s BP profile over a 24-hour period
including both awake and sleep time. Such valuable
information cannot be offered by office BP and home
BP measurements. This allows the identification
of individuals white-coat HT (WC HT), HT with
white-coat effect (HT with WC effect), masked HT and
masked uncontrolled HT. Therefore, some prestigious
international guidelines on management of HT have
recommended the use of ABPM in establishing the
diagnosis of HT or monitoring BP control in existing
hypertensive patients.8,9.10 Indeed, ABPM has been
shown to be cost-effective both in specialist services
and in primary care, with large amount of resources
being saved due to more rational drug prescribing
and better BP control.11 However, despite all of this
evidence, the application of ABPM in primary care is
still suboptimal. For example, a review of ABPM use
in 11 Asian regions including China, Japan, Korea and
Singapore published in the year 2019 noted that ABPM
was seldom available in primary care clinics.12 It is
therefore not surprising to find that ABPM has been
underused in the primary care setting.
ABPM services has been introduced to public
General Outpatient Clinics (GOPCs) of Kowloon Central
Cluster (KCC) under the Hospital Authority of Hong
Kong (HAHK) since 2015. It assists in the diagnosis of
HT in suspected hypertensive patients and monitoring of
BP control in hypertensive patients. Until this moment,
the service utilisation and the results of the ABPM
performed in local primary care clinics had not been
widely studied. To fill in this knowledge gap, this study
aims to delineate the indications for ordering ABPM in
the public primary care setting and to explore the patient
characteristics and the results of the ABPM. We believe
that the results of our study will provide important
background information for the use of ABPM in public
primary care clinics and enlighten family physicians on its
proper application and interpretation in HT management.
Methods
Study Design:
Cross-sectional descriptive study carried out at
public primary care clinics
Subjects:
All patients with ABPM done within the period
from 1/12/2016 to 30/11/2017 in five GOPCs of KCC
under the Hospital Authority of HK were included. It
was estimated that around 14000 hypertensive patients
attended these clinics in the period. ABPM would be
ordered in GOPC directly by the attending doctors if
indicated. Patients who were intolerant to ABPM or
whose ABPM data was invalid were excluded.
Ambulatory blood pressure monitoring
ABPM measures blood pressure monitoring
patients’ BP during a 24-hour period. “ABPM awake”
and “ABPM sleep” were defined according to the
patients’ schedule. All patients who have undergone
ABPM were asked about the awake and sleep time
and these data were entered into an ABPM software
(cardioversions 1.16.6). They were advised not to do
vigorous exercise during ABPM. Awake BP readings
were measured in 30-minutes intervals. Sleep readings
were measured in 45-60-minutes intervals, depending
on the total number of sleeping hours, with a minimum
of 7 measurements during sleep. The minimum awake
measurements should not be less than 20. The ABPM
would be considered as invalid if the overall successful
measures were less than 70% of all readings.13
Indications for ambulatory blood pressure monitoring
ABPM is usually indicated in the following
scenarios in our clinics based on the recommendations
from the NICE guidelines8:
-
To establish the diagnosis of HT, especially
if patients do not have out-of-office BP
measurements.
-
To monitor the BP control among
hypertensive patients, such as those with
unusual discrepancy between their clinic BP
measurement and home BP measurement,when
there are symptoms suggestive of hypotension,
or when evaluating drug resistant HT.
Sample size calculation
The prevalence of white-coat HT in the community
was reported to be 20 – 25% in the literature.14
Assuming the proportion of white-coat HT is 25% in
primary care clinics, margin of error being 5% and
confidence level of 95%, by using the formula:
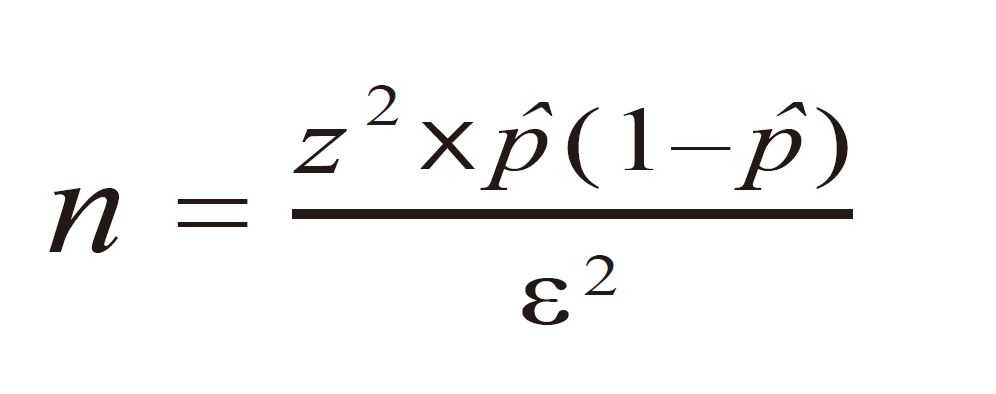
(https://www.calculator.net/sample-size-calculator.html; z is the z
score, ε is the margin of error and p̂ is the population proportion),
the required sample size is 289. To allow room for case
exclusion (~15%), 340 samples were included in the study.
Determination of variables
All relevant clinical data were retrieved from the
Clinical Management System (CMS) of HAHK. The
demographic data of the patients including age, gender
and comorbidities with diabetes (DM) or pre-diabetes
including impaired fasting glucose and impaired glucose
tolerance were retrieved. The patients’ BP reading on
the date of ABPM ordered, the indications of the ABPM
and the final diagnosis after the ABPM was done were
also collected. According to the latest NICE guideline8
and American Diabetes Association guideline in
202015,cinic BP is defined as normal if the reading is
<140/90mmHg either in the presence or absence of DM.
Statistical analysis
Statistical analysis was performed using the
Statistical Package for the Social Sciences (Windows
version 26.0; SPSS Inc, Chicago [IL], US). All
continuous variables are expressed as mean ± standard
deviation. Categorical data are reported as number and
percentages. Chi-square test was used for comparing
the categorical variables. A P-value of less than 0.05 is
considered as statistically significant.
Results
349 patients had ABPM performed during the one-year
study period, among which 26 patients (7%) were
excluded from data analysis as their ABPM results
were invalid. Table 1 summarised the characteristics
of the remaining 323 patients (93%) included in the
data analysis. Among them, 208 (64%) were female
and 115 (36%) were male. They were aged 19 - 94
years old, with the mean age being 64 ± 12. Their mean
clinic systolic BP was 151 ± 18 mmHg and mean clinic
diastolic BP was 81 ± 12 mmHg. 65 patients (20%)
were found to have normal clinic BP readings at the
time when ABPM was ordered. Furthermore, 67 (21%)
were found to have concomitant DM and 53 (16%) with
pre-diabetes including impaired glucose tolerance or
impaired fasting glucose. The average waiting time for
the ABPM service was 26 days.
As to the indications for ABPM, 150 (46%) were
for establishing a diagnosis of HT and 173 (54%)
were for monitoring of BP control among confirmed
HT patients. For those whose ABPM were ordered for
diagnosing of HT, 96 (64%) were confirmed to have a
diagnosis of HT, 42 (28%) were found to have white-coat
HT, i.e. elevated clinic BP with normal ABPM
and 12 (8%) were found to be totally normotensive
( Figure 1). The age and gender distribution among the
subgroups were comparable ( Table 2).
For those whose ABPM were indicated for
monitoring of BP control among hypertensive patients,
98 (57%) were noted to have suboptimal BP control
and 67 (39%) were hypertensive patients with white-coat
effect, i.e. elevated clinic BP but normal ABPM in
treated HT individuals (Figure 2). Again, the subgroup
analysis as shown in Table 3 revealed that their age and
gender condition were comparable.
Sixty-five patients had ABPM ordered although
their clinic BPs were normal (<140/90mmHg). Among
them, 37 (57%) were found to have elevated ABPM,
with 18 (28%) having masked HT and 19 (29%) having
masked uncontrolled HT ( Figure 3).
Discussion
Although wide evidence from literature has
confirmed the benefit of ABPM in establishing the
diagnosis of HT and the management of different types
of HT, its application in primary care is still far from
satisfactory. For example, a cross-sectional survey of
more than 400 primary care doctors in HK in 2019
found that there was a significant underutilisation of
ABPM, with only 1.6% doctors using this method to
diagnose HT and 4.1% using this for management of
HT.16 In our study, due to limited resource in the public
primary care system, only 349 cases had ABPM done
during the one-year study period and this figure was
definitely suboptimal in view of the large numbers
of HT patients management in the GOPCs. We hope
our study would help delineate the role of ABPM by
reviewing the application of ABPM in local primary
care clinics and therefore advocate its use among all
primary care doctors in HK.
Our study reveals that nearly one third of untreated
individuals were noted to have white-coat HT and
more than one third of hypertensive patients were
found to have white-coat effect. These findings are
consistent with a local study done in 2007 showing
that 28.2% of all HT patients had white-coat HT in
primary care.17 Similarly, in another local study done
by Chiang et al in 2013, 30% of treated hypertensive
patients in a public GOPC were found to have white-coat
effect.18 Currently, there is insufficient evidence
from randomised controlled trials to determine whether
white-coat HT warrants treatment.19 Dietary advice
and lifestyle modifications were recommended as the
mainstay of treatment for white-coat HT.20 With the
help of ABPM, over-diagnosis of HT could be avoided
in nearly 30% of cases and therefore prevent the wrong
labelling of “HT” among this group. Similarly, the use
of ABPM helps ease the worry of those HT patients
with W-C effect and subsequently avoid the unnecessary
medication augmentation. This is particularly important
as otherwise the patients will be at risk of hypotension
due to overtreatment and be susceptible to the potential
side-effects from drug treatment. All these findings have
corroborated the importance of doing ABPM before
establishing the diagnosis of HT or when white-coat
effect is suspected among treated HT patients.
Importantly, more than half of the patients were
found to have suboptimal BP control in the group of
hypertensive patients whose ABPM were ordered for
monitoring of BP control. This result is consistent with
findings from another study showing that more than
40% of patients labelled as having “HT with white-coat
effect” were actually having suboptimal BP control in
the local primary care clinics.21 This finding should alert
primary care doctors to the importance of conducting
ABPM for confirming the BP control status before
the clinical decision of “satisfactory control” is made
liberally. Although regular home BP monitoring (HBPM)
could help confirm the white-coat effect among
hypertensive patients too, self-reporting bias, patients
with impaired cognition and the lack of monitoring
during the sleep time by typical HBPM machine may
prompt the use of ABPM rather than HBPM.20 In view
of the fact that poorly controlled BP will significantly
increase hypertensive patient’s cardiovascular risks,
family physicians should carefully review their BP
control status during every follow-up visit and refer the
case to have ABPM if in doubt.
It is alarming to note that quite a number of
patients referred to ABPM with normal clinic BP were
found to have either masked HT (28%) or masked
uncontrolled HT (29%). A local study by CM Ng et
al involving type 2 diabetic patients who were not on
any antihypertensive in a tertiary clinic found that the
prevalence of masked HT was 18% by ABPM.22 The
high percentage of masked HT or masked uncontrolled
HT of our study might be explained by several reasons.
Firstly, when ABPM was referred for patients whose
clinic BP was normal, their home BP readings were
usually elevated. The discrepancy between the clinic
BP and home BP readings would prompt the attending
doctor to further assess their BP control by ABPM.
As the BP machines in the study clinics are under
regular maintenance and validation service provided
by the Hospital Authority, we assume the clinic BP
machines and measurements were accurate in our study.
Secondly, ABPM would be ordered for patients having
early development of cardiovascular complications or
chronic kidney disease (CKD) with seemingly well
controlled HT. This is a sensible choice as many such
patients were later confirmed to have masked HT
or masked uncontrolled HT by ABPM and therefore
warranting closer BP monitoring and stricter control.
Such people usually have more metabolic risk factors
and asymptomatic organ damage than those who are
truly normotensive.23 This is particularly important in
view of the large amount of evidence showing that
masked HT significantly increases the cardiovascular
morbidity.24,25 The long-term risk of developing
sustained HT, DM, or left ventricular hypertrophy in
masked hypertensive patient is 2 to 3 times greater than
that of individuals with normal in- and out-of-office
BP.26 With all these findings, we would like to appeal to
all primary care doctors to enhance the use of out-ofoffice
BP measurements including ABPM when there is
reasonable doubt on the BP control although the clinic
BP is normal. An accurate and timely assessment of
BP control could prevent or delay the development of
cardiovascular complications.
Limitations of the study
There are some limitations in this study. First, the
study was carried out in one single cluster of HAHK,
therefore these results from the public primary health
care sector might not be applicable to the private
sector or secondary care. In addition, only 323 cases
who fulfilled the ABPM referral criteria and with valid
ABPM results were included in the data analysis,
therefore selection bias might exist. Nevertheless, as
the data included all patients who had done ABPM
from five primary care clinics in HAHK during the
one-year study period, these data may give a realistic
representation of ABPM service performed in the
public primary care settings and had provided important
background information for future service enhancement.
Secondly, apart from DM and pre-diabetes, data on other
comorbidities such as ischemic heart disease, stroke or
CKD etc. had not been collected. It is therefore hard to
determine the correlations between the ABPM findings
with the cardiovascular or renal complications. Future
studies with more comprehensive data collection will be
needed to further explore this important aspect. Thirdly,
due to feasibility reasons, not all participants were able
to do the ABPM on the same day and their average
waiting time was 26 days. Patient’s clinic BP on the
date when ABPM was ordered might be substantially
different from the date when ABPM was performed.
Having said so, since most cases who attended the
GOPCs were comparatively stable cases and therefore
the four weeks’ time interval is a reasonable timeframe
where patients’ clinical condition would unlikely to
have dramatically changed. Lastly, because of the crosssectional
nature of the study, we were unable to adjust
for potential unmeasured confounders and therefore no
temporal or causal relationship could be established.
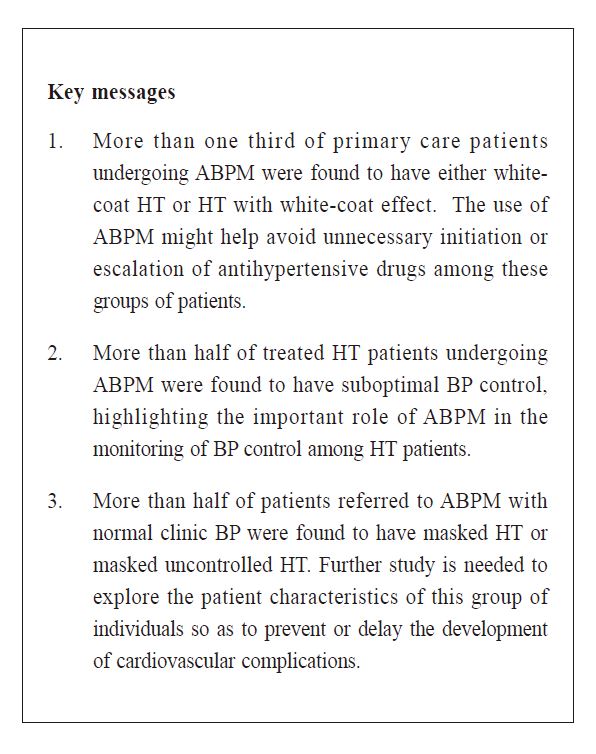
Conclusion
Our study successfully delineated the indications
for ordering ABPM in the public primary care setting,
explored the patient characteristics and the results of
the ABPM. ABPM was used for both establishing the
diagnosis of HT and monitoring of BP in hypertensive
patients. More than one third of primary care patients
undergoing ABPM were found to have either white-coat
HT or HT with white-coat effect. The use of ABPM
might help avoid unnecessary initiation or escalation of
antihypertensive drugs among these groups of patients.
In addition, more than half of treated HT patients
undergoing ABPM were found to have suboptimal
BP control, highlighting the important role of ABPM
in the monitoring of BP control among HT patients.
Furthermore, more than half of patients referred to
ABPM with normal clinic BP were found to have
masked HT or masked uncontrolled HT. Further study
is needed to explore the risk factors contributing to the
development of masked HT and to prevent or delay the
development of cardiovascular complications among
this group of patients.
Acknowledgements
We would like to thank all clinic staff of Department
of Family Medicine & GOPCs, KCC of the HAHK for
their professional service and unfailing support to this
service review on ABPM use, without which this project
would not have been accomplished.
References
-
NCD Risk Factor Collaboration. Worldwide trends in blood pressure from
1975 to 2015: a pooled analysis of 1479 population-based measurement
studies with 19·1 million participants. Lancet. 2017; 389: 37–55.
-
Department of Health. Report on Population Health Survey 2014/15. 2017.
Department of Health. Hong Kong SAR.
-
GBD 2016 Risk Factors Collaborators. Global, regional, and national
comparative risk assessment of 84 behavioural, environmental and
occupational, and metabolic risks or clusters of risks, 1990–2016: a
systematic analysis for the Global Burden of Disease Study 2016. Lancet.
2017; 390: 1345–1422.
-
Eleni Rapsomaniki, Adam Timmis, Julie George, et al. Blood pressure and
incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years
lost, and age-specific associations in 1.25 million people. Lancet. 2014; 383:
1899–1911.
-
Dena Ettehad, Connor A Emdin, Amit Kiran, et al. Blood pressure lowering
for prevention of cardiovascular disease and death: a systematic review and
meta-analysis. Lancet. 2016; 387: 957–967.
-
Yang W, Melgarejo JD, Thijs L, et al. Association of Office and Ambulatory
Blood Pressure with Mortality and Cardiovascular Outcomes. JAMA.
2019;322(5):409–420.
-
Piper MA, Evans CV, Burda BU, et al. Diagnostic and predictive accuracy
of blood pressure screening methods with consideration of rescreening
intervals: a systematic review for the U.S. Preventive Services Task Force.
Ann Intern Med. 2015;162(3):192-204.
-
National Institute for Clinical Excellence (NICE). Hypertension in adults:
diagnosis and management, NICE Clin Guidel. 2019. Available from https://
www.nice.org.uk/guidance/ng136/resources/hypertension-in-adults-diagnosis-and-
management-pdf-66141722710213.
-
Nerenberg KA, Zarnke KB, Leung AA, et al. Hypertension Canada’s 2018
guidelines for diagnosis, risk assessment, prevention, and treatment of
hypertension in adults and children. Can J Cardiol. 2018;34:506–525.
-
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/
ACPM/AGS/ APhA/ASH/ASPC/NMA/PCNA guideline for the prevention,
detection, evaluation, and Management of High Blood Pressure in adults: a
report of the American College of Cardiology/American Heart Association
task force on clinical Pr. J Am Coll Cardiol. 2018;71:e127–248.
-
O'Brien E. Twenty-four-hour ambulatory blood pressure measurement in
clinical practice and research: a critical review of a technique in need of
implementation. J Intern Med. 2011 May;269(5):478-495.
-
Shin, J, Kario, K, Chia, Y-C, et al. Current status of ambulatory blood
pressure monitoring in Asian countries: A report from the HOPE Asia
Network. J Clin Hypertens. 2020; 22: 384.
-
Parati G, Stergiou G, O'Brien E, et al. European society of hypertension
practice guidelines for ambulatory blood pressure monitoring. J Hypertens.
2014; 32: 1359-1366.
-
Pickering TG, Hall JE, Appel LA, et al. Recommendations for blood
pressure measurement in humans and experimental animals: Part 1: blood
pressure measurement in humans: a statement for professionals from the
Subcommittee of Professional and Public Education of the American Heart
Association Council on High Blood Pressure Research. Hypertension 2005;
45:142–161.
-
Introduction: Standards of Medical Care in Diabetes-2020. Diabetes Care.
2020 Jan;43(Suppl 1): S1-S2.
-
Lee EKP, Choi RCM, Liu L, et al. Preference of blood pressure measurement
methods by primary care doctors in Hong Kong: a cross-sectional survey.
BMC Fam Pract. 2020; 21 (1):95.
-
Tam TKW, Ng KK, Lau CM. What are the predictors of white-coat hypertension
in Chinese adults? Hong Kong Practitioner 2007. Nov;29:411-418.
-
Chiang LK, Ng L. Ambulatory blood pressure monitoring (ABPM) for
hypertension management in primary care setting: an experience sharing
from Kwong Wah Hospital. HK Pract 2013;35:5-11.
-
Nuredini G, Saunders A, Rajkumar C, et al. Current status of white
coat hypertension: where are we? Ther Adv Cardiovasc Dis. 2020 Jan-
Dec;14:1753944720931637.
-
Williams B, Mancia G, Spiering W, et al. Authors/Task Force Members:.
2018 ESC/ESH Guidelines for the management of arterial hypertension: The
Task Force for the management of arterial hypertension of the European
Society of Cardiology and the European Society of Hypertension: The Task
Force for the management of arterial hypertension of the European Society
of Cardiology and the European Society of Hypertension. J Hypertens. 2018
Oct;36(10):1953-2041.
-
Chou SCW, Chau CKV, Yeung KK, et al. White coat effect can be an
illusion that may possibly result in sub-optimal blood pressure control? HK
Pract 2017;39:129-143.
-
Ng CM, Yiu SF, Choi KL, et al. Prevalence and significance of white-coat
hypertension and masked hypertension in type 2 diabetics. Hong Kong Med J.
2008;14(6):437-443.
-
Tientcheu D, Ayers C, Das SR, et al. Target Organ Complications and
Cardiovascular Events Associated With Masked Hypertension and White-
Coat Hypertension: Analysis From the Dallas Heart Study. J Am Coll
Cardiol. 2015 Nov 17;66(20):2159-2169.
-
Palla M, Saber H, Konda S, et al. Masked hypertension and cardiovascular
outcomes: an updated systematic review and meta-analysis. Integr Blood
Press Control. 2018;11:11-24.
-
Banegas JR, Ruilope LM, de la Sierra A, et al. Relationship between clinic
and ambulatory blood-pressure measurements and mortality. N Engl J Med
2018;378:1509–1520.
-
Mancia G, Verdecchia P. Clinical value of ambulatory blood pressure:
evidence and limits. Circ Res. 2015 Mar 13;116(6):1034-1045.
Kwai-sheung Wong,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Associate Consultant,
Department of Family Medicine and General Outpatient Clinics, Kowloon Central Cluster,
Hospital Authority Hong Kong
Ka-ming Ho,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Associate Consultant,
Department of Family Medicine and General Outpatient Clinics, Kowloon Central Cluster,
Hospital Authority Hong Kong
Yim-chu Li,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Chief of Service, Consultant,
Department of Family Medicine and General Outpatient Clinics, Kowloon Central Cluster,
Hospital Authority Hong Kong
Catherine XR Chen,
PhD (Medicine), MRCP (UK), FRACGP, FHKAM (Family Medicine)
Consultant,
Department of Family Medicine and General Outpatient Clinics, Kowloon Central Cluster,
Hospital Authority Hong Kong
Correspondence to:
Dr Kwai-sheung Wong, Department of Family Medicine and
General Out-patient Clinic, Room 807, Block S, Queen Elizabeth
Hospital, 30 Gascoigne Road, Kowloon, Hong Kong SAR.
E-mail: wks638@ha.org.hk
|
