Dental considerations in older adults attending
the primary care clinic
Katherine CM Leung 梁超敏
HK Pract 2023;45:105-111
Summary
Oral health is part of our general health. Older adults
attending the primary care medical clinic often require
dental care as well. Many of them present with dental
caries, periodontal diseases and tooth-loss due to
worsened physical health and other cumulative damage
brought by previous dental diseases.
The elderly patients may also be suffering from
systemic diseases and/or conditions which may have
direct impact on their dental conditions. This article
draws the attention of physicians, who are treating their
older patients, to major dental diseases as well as the
interactions between systemic diseases and/or other
medical conditions with their dental conditions.
Therefore, dental and medical professionals should work
closely together to provide collaborative patient care.
Keywords: Older adults, dental diseases, primary care
摘要
口腔健康是整體健康的一部分。尋求基層醫療的老年人通
常也需要牙科護理。由於身體健康變差和牙齒受先前的牙
患累積的破壞,他們大都患有齲齒( 蛀牙) 、牙周病和缺
牙。他們也可能患上一些可直接影響口腔健康的疾病。本
文提請治療老年人的醫生注意主要的牙齒疾病及其與身體
疾病的相互作用。牙醫和醫生應攜手合作給予病人全面的
照顧。
關鍵詞:老年人,牙齒疾病,基層醫療
Introduction
Oral health is part of our general health. Older
people receiving medical care often require dental
care as well. With increased dental awareness and
better access to dental care, the elderlies tend to retain
more teeth into their later years of life. However, the
dental condition of the older patients is often far from
satisfactory, due to their worsening physical conditions
and cumulative damage caused by dental diseases in
their past. Furthermore, degenerative changes, chronic
diseases and their treatments received can negatively
affect their oral health.
Two major dental diseases that cause eventual tooth
loss if left untreated are dental caries and periodontal
disease. Both diseases are to a large extent induced by
dental plaque accumulation.
Dental plaque
Dental plaque is a collection of microorganisms
found on a tooth surface as a biofilm, embedded in
a matrix of polymers of host and bacterial origin.1
It accumulates preferentially at stagnant areas such
as proximal surfaces between teeth, underneath
fixed dental prostheses and on the fitting surface of
removable dentures, as these sites are normally less
affected by the flushing effect of saliva and tongue
movement. Dental calculus is formed when the
minerals from saliva calcify the dental plaque. The
surface of dental calculus is rough and further attracts
plaque deposition.
Dental diseases
(a) Dental caries
Dental caries is a transmissible bacterial
disease process caused by acids from bacterial
metabolism diffusing into enamel and dentine
and dissolving the mineral.2 It is a major non-communicable
disease affecting the vast majority
of older adults. The estimated annual increments
of coronal3 and root4 caries are 0.86 and 0.5
surfaces respectively. A recent systematic review
highlighted that the trend of dental caries had
shifted from children to adults with the third peak
of caries emerging at around the age of 70, due
to the appearance of root caries.5 People who are
older, of lower socioeconomic status, tobacco users
and those with more severe gingival recession
and poorer oral hygiene have a higher risk of root
caries.6
Demineralisation of tooth substances occurs
when bacteria metabolise sugar in the mouth
to produce acid that demineralises the tooth
substances. This happens when food containing
carbohydrate is being consumed. This process
can be reversed by remineralisation of the
affected tissues naturally by salivary minerals
or therapeutically by fluoride. However, if
remineralisation does not happen due to persistently
low pH of the oral cavity e.g. frequent meals, or
unavailability of fluoride, the enamel breaks down
and cavities appear, and the infection can spread
to the underlying dentine. This causes sensitivity,
or sharp and mild to moderate degree of pain
when the patient consumes cold and sweet food
and beverage. The carious sites appear brown or
black with visible pits or cavities. Restoration
of the carious lesions is necessary to remove the
infected tooth substance, and to prevent plaque
accumulation and food stagnation to facilitate
proper toothbrushing.
When the infection spreads further to the
vascularised and innervated dental pulp, it causes
pulpal inflammation and necrosis. The severe
and spontaneous dental pain can keep the patient
awake. Dental abscesses may also develop. At
this stage, root canal treatment will be needed. It
is noteworthy that caries damages the tooth and
the restorative procedures can further weaken it,
risking its fracture upon receiving masticatory load.
Fluoride is an effective anti-caries agent which
halts demineralisation and promotes remineralisation
of enamel and dentine.7 Dentists usually apply
fluoride varnish, containing 22600 ppm fluoride,
2-4 times a year for caries prevention and arrest
of early lesions. In the past decade or two, silver
diamine fluoride (SDF) became the gold standard
for root caries prevention and treatment.8 It is also
effective in the remineralisation of deep carious
lesions on the occlusal surface and the treatment of
hypersensitive dentine. Among the professionally
applied topical fluorides, an annual application
of 38% SDF solution combined with oral health
education has been shown to be the most effective
way of dental root caries prevention.9
(b) Periodontal disease
Plaque-related gingivitis occurs when dental
plaque accumulates along the gingival margin over
days or weeks without disruption or removal while
non plaque-related gingival diseases can arise due
to various causes10-11 including genetic disorders
such as hereditary gingival fibromatosis, specific
infections, e.g. candidiasis, autoimmune diseases
of the skin and mucous membrane, such as lichen
planus, herpes simplex I & II, and leukaemia. The
initial phase of plaque-related periodontal disease
is gingivitis which involves host-immune response
to dental plaque. Healthy gingiva appears pink
and firm, and attaches closely to teeth, whilst it
reddens, swells, sores and bleeds on probing in
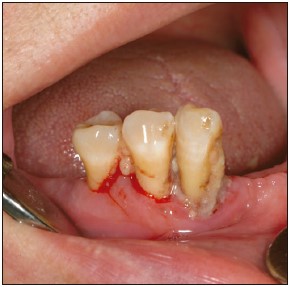
gingivitis (Figure. 1).
Figure 1:
This patient suffers from periodontal disease.
Heavy plaque deposition around the gingival
margin, bleeding on probing and recession of
the gingiva exposing the root surfaces can be
seen.
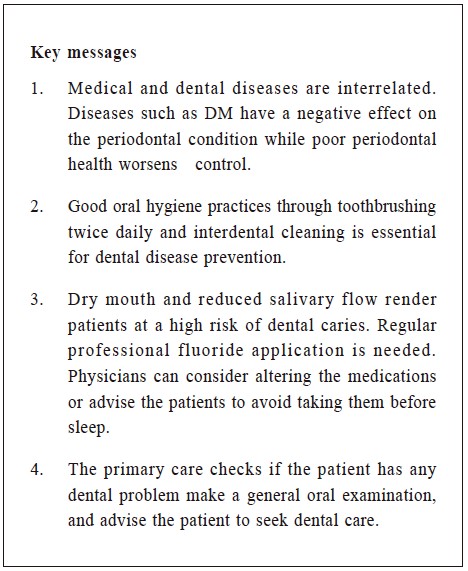
Figure 2:
Dental caries attack the lingual surface of the
lower anterior teeth of a Sjögren’s syndrome
sufferer. These sites are usually protected by
a continuous flow of saliva.
Certain drugs and smoking habits can modify
the host response to dental plaque. For example,
patients taking calcium channel blockers, antiepileptics
and immunosuppressants may show
abnormal gingival enlargement.12 Smokers usually
exhibit less gingival bleeding, greater alveolar bone
loss and clinical attachment loss. The treatment
response is suboptimal and healing is impaired.13 This
implies that periodontal diseases are more difficult
to detect and the treatments are less effective.
Plaque-related gingivitis can be resolved when
dental plaque is removed. However, if it is allowed
to accumulate for a long time, apical movement of
the gingival margin will lead to gingival recession
and hence root surface exposure. The root surface
dentine is prone to caries. The tooth may become
hypersensitive and present with pain or discomfort
to cold and other stimuli such as sour food.
The advanced stage of periodontal disease,
or periodontitis, is irreversible. The clinical signs
include increased probing depth, clinical attachment
loss, and tooth mobility and displacement.
Periodontal abscess with pus draining may be
present. In severe cases, the tooth may self-exfoliate.
The patient often complains of halitosis,
tooth mobility, poor masticatory efficiency,
chewing discomfort, and food packing.
Oral hygiene practice
The key prognostic factor of periodontal disease
is dental plaque accumulation. Therefore, good oral
hygiene practice that includes toothbrushing twice
daily and interdental cleaning are necessary. Non-surgical
periodontal therapy including scaling and root
planning aims to remove dental calculus and smoothen
the root surfaces to enable the resolution of gingivitis.
As an adjunct measure, 0.2% chlorhexidine digluconate
mouthwash may be prescribed.14 However, its long-term
use is not recommended due to side effects like
a change in taste, staining of the teeth, the gingiva
and the dental appliances, irritation and superficial
desquamation of the oral mucosa. Oral antibiotics may
sometimes be necessary to eliminate causative bacteria.
For periodontitis, surgical periodontal treatment
involves flap surgery to expose root surfaces for
scaling and root planing. For cases with severe gingival
recession and bone resorption, grafting of soft tissues
or bone and guided bone regeneration to cover exposed
roots for aesthetics and to enhance bony support may
also be performed.
Dental plaque is a causative factor in both dental
caries and periodontal diseases. Proper oral hygiene
measures cannot be overemphasised. Mechanical plaque
removal by toothbrushing with regular fluoridated
toothpaste (1000-1450 ppm fluoride) twice daily is
mandatory. In high caries-risk cases, dentists may
recommend using high-fluoride (5000 ppm fluoride)
toothpaste. Interdental cleaning can be carried out with
the use of dental floss or an interdental brush.
Assisted toothbrushing is required for patients who
have problems with self-care. For those whose manual
dexterity has deteriorated, a modified toothbrush to
improve handgrip or the use of an electric toothbrush
may be helpful.
The inter-related medical and dental conditions
Medical and dental conditions are often interrelated.
Some chronic systemic diseases commonly seen in older
adults can directly affect the oral tissues. Medications
that modify the immune / inflammatory response or
reduce salivary flow can complicate oral health problems.
Dry mouth and reduced salivary flow
Saliva exerts an important protective effect on
the oral cavity through its flow and composition. Its
mineralising, buffering and antimicrobial properties
are crucial for preventing dental caries and providing
resistance to dental infections. Degenerative changes
of the salivary glands, diseases such as diabetes
mellitus and Sjögren’s syndrome15, head and neck
radiotherapy16, and an array of medications17 including
the antidepressants and some diuretics, can reduce
saliva secretion. Compositional change of the saliva to
low bicarbonate and phosphate concentration impairs its
buffering capacity. A longer time is needed to neutralise
the oral acid, hence inducing a higher caries risk.18
Although xerostomia, a condition when there is
a sensation of oral dryness resulting from diminished
saliva production, seldom presents as the main concern
for patients seeking medical or dental care. it can affect
up to one-third of older adults worldwide.19 Complaints
of xerostomia may be subtle and indirect: for example,
choking when dry food is taken, dry cough, the tongue
sticking to removable dentures. These problems can
be avoided by not taking dry food or by having a sip
of liquid when taking dry food. Since xerostomia is
a subjective feeling, its presence can often be missed
without asking the question, “do you feel your mouth is
dry?”.20
Clinically, saliva with decreased salivary flow is
viscous, sticky, frothy and bubbly. Those patients often
present with heavier dental plaque deposition, greater
number of dental caries and the lesions are located at
sites generally not susceptible to decay such as the
lower lingual region (Figure. 2), and more missing
teeth, worse periodontal condition and heavily restored
dentition, when compared to those with normal salivary
flow rate. Their oral mucosa looks dry and friable and
the tongue may appear dry and lobulated. They are
also more prone to oral mucosal infections such as oral
candidiasis. They may also experience difficulties in
speaking, swallowing, taste alteration and have burning
mouth syndrome. Their oral health-related quality of
life is also reduced.
Dentists usually detect oral dryness by testing if the
oral mucosa sticks to the dental mirror. Commercially
available test kit can be used to check the unstimulated
and stimulated salivary flow rates, and the pH and
buffer capacity.
Some patients may develop a habit of consuming
acidic food and drinks to stimulate salivary flow. This
habit should be deterred because it can lead to tooth
erosion. Tooth surface loss does not only jeopardise the
aesthetics when the anterior teeth become shortened, it can
also cause hypersensitivity or pain which may, depending
on its severity, require root canal treatment. Restoration
of the teeth can be complicated because of reduced
clinical crown height and lack of interocclusal space.
Medical physicians can consider prescribing
medications which are less xerogenic. However, if such
alternative medicines are unavailable, it is useful to
advise the patients to take the causative medications
during the day when activities in the oral cavity are at
the maximum, and avoid taking them before sleep when
the salivary flow rate is low, and also the number of
bacteria in saliva increases rapidly at night.21
Various palliative and preventive measures,
including pharmacologic treatment with salivary
stimulants, saliva substitutes, and the use of sugar-free
chewing gum/lozenges may alleviate some symptoms of
dry mouth and may improve the patient’s quality of life.
Diabetes mellitus patients
Diabetes mellitus (DM) is a common endocrine
disorder in older adults. DM is linked to many different
dental problems and conditions such as periodontal
disease, delayed wound healing, taste alteration and
dental infections. The relationship between DM and
periodontal disease is bi-directional.22 Diabetic patients
have a higher risk of periodontitis, and their periodontal
conditions worsen control of diabetes treatments, while
people with periodontitis have an elevated risk for
dysglycaemia and insulin resistance. There is a high
association/risk between poor periodontal conditions
and diabetes complications.23
In addition, hyperglycaemia, hyperinsulinemia
and dyslipidaemia cause increased oxidative stress,
inflammation, increased sympathetic activity, and
impaired insulin signalling in the salivary glands,
resulting in salivary gland dysfunction and the flow of
saliva is reduced.24 Diabetic patients often complain of
xerostomia. Reduced salivary flow also promotes dental
plaque accumulation and therefore further worsens their
periodontal health, making them more prone to dental
caries and oral mucosa infection.25 DM patients who use
removable dentures are more susceptible to traumatic
ulcers of the oral mucosa at the denture-bearing area
than non-DM denture wearers, probably due to slower
healing or delayed wound repair.
The current consensus guidelines advocat e
improving early diagnosis, prevention and co-management
of diabetes and periodontitis.23 DM patients
are advised to maintain good oral hygiene not only
for preventing periodontal disease but also for better
glycaemic control. Regular dental visits for denture
maintenance to avoid denture trauma are necessary.
Stroke, dementia and muscular disease
Sufferers of these conditions often have deterioration
in self-care ability. They require assistance to carry out
basic daily living activities. People with dementia usually
present with poor oral hygiene, heavy dental plaque
deposition, gingival bleeding, periodontal pockets, mucosal
lesions and reduced salivary flow.26 For stroke survivors,
apart from increased dental plaque accumulation, poorer
periodontal health and infection of the oral mucosa, they
also show impairment in mastication and swallowing
which restricts their food intake.27 Sarcopenia patients
with low muscle strength combined with poor manual
dexterity may find it challenging to grip the clasps of
a removable denture for its retrieval. In addition, their
neuromuscular control for stabilising a complete denture,
especially on the lower arch, may be compromised.
They require a longer training time to cope with new
dentures. Likewise, tooth loss is common in older
adults with sarcopenia. Compounded by the loss of
strength of the masticatory muscles, many sarcopenic
individuals experience problems with mastication.
Masticatory function and diet
Masticatory function is an important factor
influencing the quality of life in older adults.28 A
recent systematic review pointed out that masticatory
performance is significantly reduced in older adults with
sarcopenia, diabetes, chronic obstructive pulmonary
diseases, and functional dyspepsia.29
The diet of people with deteriorated masticatory
function is typically soft, low in fibre content, and high in
carbohydrates and fat.30 This type of diet poses a high risk
for many chronic diseases including atherosclerosis and
cancer.31 Moreover, deterioration in masticatory muscle
strength and salivary flow may result when jaw activity
is reduced. High carbohydrate content of meals and
increased meal frequency result in a prolonged and ample
substrate supply for cariogenic and caries-producing
bacteria, hence, increasing the risk of dental caries.
Tooth-loss and teeth replacement
Tooth-loss is the endpoint of dental disease, as a
result of the severe and cumulative destruction of the
tooth or its supporting structures. After tooth extraction,
teeth adjacent to the extraction site may drift towards
each other and the opposing tooth may over-erupt. Loss
of teeth can adversely affect aesthetics, speech, and
chewing function.
Edentulism (or total teeth loss) also affects
oral food intake, and in the long run, can lead to
malnutrition. Moreover, tooth loss has a negative impact
on social life, self-esteem and oral-health related quality
of life.32 Older adults with multiple missing teeth also
have a higher risk of dementia than those with more
teeth.33 Unwanted tooth movement also affects oral
intake, and in the long run, can lead to malnutrition.
Replacement of missing teeth
Not all missing teeth needs to be replaced. For
example, dentists seldom replace the missing third molars
and, in some cases, even the second molars are not
replaced. Nonetheless, missing teeth need to be replaced
for restoring aesthetics and function, and maintaining
arch integrity to prevent unwanted tooth movement
due to the loss of neighbouring or opposing teeth.
Dental prostheses are commonly used for tooth
replacement. In Hong Kong, about two-thirds of the
older population wear some type of dental prostheses.34
Dental prostheses can either be fixed or removable
and are supported by natural teeth, mucosa or dental
implants. Dental prostheses are considered a plaque
retentive factor since the artificial material attracts
plaque accumulation and there are many stagnant areas
underneath the prosthesis where dental plaque and food
debris can accumulate. Additional effort has to be paid
to maintain cleanliness of the prostheses in addition to
the daily oral hygiene procedures of the natural teeth.
Dental implants expand the treatment modality
for tooth replacement and have become popular in the
past decade or two. Success of dental implant therapy
relies on careful patient selection which takes into
account their medical and dental conditions, as well
as compliance with oral hygiene measures. Diabetic
patients showed more marginal bone loss than non-diabetic
patients, albeit no significant difference in the
rate of implant failure.35
For diabetes mellitus patients, their condition
has to be well controlled before considering implant
therapy. BRONJ (Bisphosphonate-related osteonecrosis
of the jaw), after implant surgery and other oral and
maxillofacial surgeries have been reported in patients
receiving bisphosphonate treatment. Poor oral hygiene
is one of the risk factors. If this occurs, the oral
surgeon needs to remove the implant and resect the
necrotic bone.36 To prevent BRONJ, discontinuation of
bisphosphonate may be necessary before implant surgery
and maintenance of good oral hygiene is required.
In busy primary care clinics
In a busy primary care clinic, the primary care
physician may ask if the patient has any discomfort
with the teeth and oral tissues, and take a general
examination of the oral cleanliness by observing the
extent of dental plaque deposition on an annual basis.
Advise the patients to see a general dental practitioner
for a comprehensive dental examination if the oral
hygiene is sub-optimal or if they have any oral and
dental discomfort. It is recommended that patients with
medical disease should visit a dentist at least half-yearly
for check-ups and preventive care which include
scale and polish, fluoride application and adjustment of
dental prostheses if needed.
Conclusion
Older adults are often simultaneously affected by
medical and dental diseases. These diseases are interrelated.
It is prudent for physicians to be aware of
the common dental diseases and how they affect the
progress of medical diseases. Likewise, dentists should
also be cognizant of the patients’ medical conditions so
as to provide timely and appropriate treatment for them.
Dental and medical professionals need to collaborate
to provide suitable and well-planned treatment for the
benefit of our patients.
References
-
Marsh PD. Dental plaque as a microbial biofilm. Caries Res. 2004;38(3):204-211.
-
Featherstone JD. Dental caries: a dynamic disease process. Australian dental
journal. 2008;53(3):286-291.
-
Griffin SO, Griffin PM, Swann JL, et al. New coronal caries in older adults:
implications for prevention. J Dent Res. 2005;84(8):715-720.
-
Hariyani N, Setyowati D, Spencer AJ, et al. Root caries incidence and
increment in the population - A systematic review, meta-analysis and metaregression
of longitudinal studies. J Dent. 2018;77:1-7.
-
Kassebaum NJ, Bernabe E, Dahiya M, et al. Global burden of untreated caries:
a systematic review and metaregression. J Dent Res. 2015;94(5):650-658.
-
Zhang J, Leung KCM, Sardana D, et al. Risk predictors of dental root caries:
A systematic review. Journal of dentistry. 2019;89:103166.
-
Chu CH, Mei ML, Lo EC. Use of fluorides in dental caries management.
Gen Dent. 2010;58(1):37-43; quiz 4-5, 79-80.
-
Hendre AD, Taylor GW, Chavez EM, et al. A systematic review of
silver diamine fluoride: Effectiveness and application in older adults.
Gerodontology. 2017;34(4):411-419.
-
Zhang J, Sardana D, Li KY, et al. Topical Fluoride to Prevent Root Caries:
Systematic Review with Network Meta-analysis. J Dent Res. 2020;99(5):506-513.
-
Chapple ILC, Mealey BL, Van Dyke TE, et al. Periodontal health and
gingival diseases and conditions on an intact and a reduced periodontium:
Consensus report of workgroup 1 of the 2017 World Workshop on the
Classification of Periodontal and Peri-Implant Diseases and Conditions. J
Clin Periodontol. 2018;45 Suppl 20:S68-S77.
-
Hanisch M, Hoffmann T, Bohner L, et al. Rare Diseases with Periodontal
Manifestations. Int J Environ Res Public Health. 2019;16(5).
-
Kinane DF, Marshall GJ. Periodontal manifestations of systemic disease.
Australian dental journal. 2001;46(1):2-12.
-
Rivera-Hidalgo F. Smoking and periodontal disease. Periodontol 2000.
2003;32:50-58.
-
Van Strydonck DA, Slot DE, Van der Velden U, et al. Effect of a chlorhexidine
mouthrinse on plaque, gingival inflammation and staining in gingivitis
patients: a systematic review. J Clin Periodontol. 2012;39(11):1042-1055.
-
Leung KCM, McMillan AS, Leung WK, et al. Oral health condition and
saliva flow in southern Chinese with Sjogren's syndrome. International
dental journal. 2004;54(3):159-165.
-
Pow EH, McMillan AS, Leung WK, et al. Salivary gland function and
xerostomia in southern Chinese following radiotherapy for nasopharyngeal
carcinoma. Clinical oral investigations. 2003;7(4):230-234.
-
Wolff A, Joshi RK, Ekstrom J, et al. A Guide to Medications Inducing
Salivary Gland Dysfunction, Xerostomia, and Subjective Sialorrhea: A
Systematic Review Sponsored by the World Workshop on Oral Medicine VI.
Drugs R D. 2017;17(1):1-28.
-
Bardow A, Moe D, Nyvad B, et al. The buffer capacity and buffer systems
of human whole saliva measured without loss of CO2. Arch Oral Biol.
2000;45(1):1-12.
-
Pina GMS, Mota Carvalho R, Silva BSF, et al. Prevalence of hyposalivation
in older people: A systematic review and meta-analysis. Gerodontology.
2020;37(4):317-331.
-
Thomson WM. Dry mouth and older people. Australian dental journal.
2015;60 Suppl 1:54-63.
-
Sotozono M, Kuriki N, Asahi Y, et al. Impact of sleep on the microbiome of
oral biofilms. PloS one. 2021;16(12):e0259850.
-
Preshaw PM, Alba AL, Herrera D, Jepsen S, et al. Periodontitis and diabetes:
a two-way relationship. Diabetologia. 2012;55(1):21-31.
-
Sanz M, Ceriello A, Buysschaert M, et al. Scientific evidence on the
links between periodontal diseases and diabetes: Consensus report and
guidelines of the joint workshop on periodontal diseases and diabetes
by the International Diabetes Federation and the European Federation of
Periodontology. J Clin Periodontol. 2018;45(2):138-149.
-
Ittichaicharoen J, Chattipakorn N, Chattipakorn SC. Is salivary gland
function altered in noninsulin-dependent diabetes mellitus and obesity-insulin
resistance? Arch Oral Biol. 2016;64:61-71.
-
Dorocka-Bobkowska B, Zozulinska-Ziolkiewicz D, Wierusz-Wysocka B,
et al. Candida-associated denture stomatitis in type 2 diabetes mellitus.
Diabetes Res Clin Pract. 2010;90(1):81-86.
-
Delwel S, Binnekade TT, Perez R, et al. Oral hygiene and oral health in
older people with dementia: a comprehensive review with focus on oral soft
tissues. Clinical oral investigations. 2018;22(1):93-108.
-
Kwok C, McIntyre A, Janzen S, et al. Oral care post stroke: a scoping
review. J Oral Rehabil. 2015;42(1):65-74.
-
Ikebe K, Hazeyama T, Morii K, et al. Impact of masticatory performance
on oral health-related quality of life for elderly Japanese. Int J Prosthodont.
2007;20(5):478-485.
-
Fan Y, Shu X, Leung KCM, et al. Associations of general health conditions
with masticatory performance and maximum bite force in older adults:
A systematic review of cross-sectional studies. Journal of dentistry.
2022;123:104186.
-
Wakai K, Naito M, Naito T, et al. Tooth loss and intakes of nutrients and
foods: a nationwide survey of Japanese dentists. Community Dent Oral
Epidemiol. 2010;38(1):43-9.
-
Walls AW, Steele JG, Sheiham A, et al. Oral health and nutrition in older
people. J Public Health Dent. 2000;60(4):304-30.
-
Nordenram G, Davidson T, Gynther G, et al. Qualitative studies of patients'
perceptions of loss of teeth, the edentulous state and prosthetic rehabilitation: a
systematic review with meta-synthesis. Acta Odontol Scand. 2013;71(3-4):937-951.
-
Fang WL, Jiang MJ, Gu BB, et al. Tooth loss as a risk factor for dementia:
systematic review and meta-analysis of 21 observational studies. BMC
Psychiatry. 2018;18(1):345.
-
Department of Health. Oral Health Survey 2011. Hong Kong: Government
Printer, 2013.
-
Moraschini V, Barboza ES, Peixoto GA. The impact of diabetes on dental
implant failure: a systematic review and meta-analysis. International journal
of oral and maxillofacial surgery. 2016;45(10):1237-1245.
-
Rupel K, Ottaviani G, Gobbo M, et al. A systematic review of therapeutical
approaches in bisphosphonates-related osteonecrosis of the jaw (BRONJ).
Oral Oncol. 2014;50(11):1049-1057.
Katherine CM Leung,
BDS, MDS (with distinction), PhD (HK), FHKAM (Dental Surgery)
Clinical Associate Professor;
Associate Dean (Taught Postgraduate Education);
Clinical Manager of the IAD-MSC.
Faculty of Dentistry, The University of Hong Kong
Correspondence to:Dr. Katherine CM Leung, Faculty of Dentistry, The University of
Hong Kong, Prince Philip Dental Hospital, 34 Hospital Road, Sai Ying Pun, Hong Kong SAR.
E-mail:kcmleung@hku.hk
|