Nocturnal hypertension among primary care
Chinese patients who underwent ambulatory
blood pressure monitoring: prevalence and
associated risk factors
Hing-han Chen 陳慶嫺, Ka-ming Ho 何家銘, Yim-chu Li 李艷珠, Catherine XR Chen 陳曉瑞
HK Pract 2023;45:21-31
Summary
Objective:
To study the prevalence and associated risk
factors of nocturnal hypertension among primary care
Chinese patients who had undergone ambulatory blood
pressure monitoring.
Nocturnal hypertension (NHT) increases the risks
of cardiovascular events. Isolated NHT was found to be
more prevalent among Chinese than among Westerners.
There has been no local data on the prevalence of
NHT and its associated risk factors among the Chinese
patients managed in Hong Kong’s primary care. To
address this knowledge gap, we conducted this study.
Method:
This study was a cross-sectional study. Chinese
patients who underwent ambulatory blood pressure
monitoring (ABPM) from 1/12/2017 to 30/11/2018 and
had annual assessment done were recruited. Their
demographic data, clinic blood pressure (BP) readings,
ABPM result and laboratory data were reviewed.
Student’s t-test and analysis of variance were used to
analyse continuous variables and the Chi square test
was used for categorical data. All statistical tests were
two-sided, and a P-value of <0.05 was considered
significant.
Results:
Among the 162 patients fulfilling the inclusion
criteria, 106 were found to have NHT with a period
prevalence of 65.4%. Among those with NHT, 17
(10.5%) patients had isolated NHT with normal daytime
blood pressure. NHT cases were found to have higher
readings of average daytime and night time BP and
more NHT cases were non-dippers. A higher proportion
of non-dippers were found to have ischaemic heart
disease (7.9% vs 0%, p=0.025) and NHT (78.2% vs
44.3%, p<0.001) than the dippers.
Conclusions:
Noctornal hypertension is commonly
encountered in primary care. Family physicians should
have enhanced awareness of the presence of NHT
and non-dippers during management of hypertension.
Concerted effort should be made to control both
daytime and night time BP to target levels and therefore
prevent the development of cardiovascular disease.
Keywords:
nocturnal hypertension, ambulatory blood
pressure monitoring, primary care, risk factor
摘要
目的:
研究接受動態血壓監測的中國基層醫療病人患有夜
間高血壓的患病率及相關危險因素。
簡介:
夜間高血壓(NHT) 會增加心血管疾病的風
險。發現單純的夜間高血壓在中方比在西方更普
遍。在接受基層醫療健康的中國病人中,沒有關於
夜間高血壓患病率及其相關危險因素的本地數據。
為了增加這一方面知識,我們進行了這項研究。
方法:
這是一項橫斷面研究。招募於2017年1月12日
至2018年11月30日接受動態血壓監測(ABPM)並進
行年度評估的中國患者。審閱了他們的人口統計數
據、臨床血壓(BP)讀數、動態血壓監測結果和實驗
室數據。學生t 測試和方差分析用於分析連續變數,Chi平方測試用於分類資料。所有統計測試都是雙面
的,P值<0.05被認為是有意義的。
結果:
在162名符合納入標準的患者中,106人被發
現患有夜間高血壓,患病率為65.4%。在夜間高血壓
患者中,有17名(10.5%)病人患有單純夜間高血壓,
白天血壓正常。夜間高血壓病例的平均白天和夜間
血壓讀數較高,並且更多夜間高血壓病例是沒有血
壓晝夜變動類型的患者。相比血壓俱有晝夜變動的
病人,發現沒有血壓晝夜變動的病人患有缺血性心
臟病(7.9%對0%,p=0.025)和夜間高血壓(78.2%對
44.3%,p<0.001)的比例更高。
結論:
夜間高血壓中基層醫療中很常見。家庭醫生在
高血壓治療過程中應提高對夜間高血壓和血壓沒有晝
夜變動的病人的認識。應共同努力將白天和夜間的血
壓控制在目標水平,從而防止心血管疾病的發展。
關鍵詞:
夜間高血壓,動態血壓監測,基層醫療,風險因素
Introduction
Hypertension (HT) is common in Hong Kong.
According to the Population Health Survey 2014/15
conducted by the Department of Health, the total
prevalence of HT was 27.7% (25.5% for females and
30.1% for males) among persons aged 15-84.1 HT
contributes substantially to cardiovascular morbidity and
mortality, and to all-cause mortality. Due to advances in
medical technology, we can evaluate blood pressure (BP)
not only during waking period, but also during sleeping
time periods. The abnormally high BP in sleeping time
is known as nocturnal hypertension (NHT).
Evidence from the literature has shown that the
presence of NHT increases the risk of cardiovascular
events, namely stroke and coronary events.2,3 In
addition, NHT is associated with poor physical
function and cognitive dysfunction in the elderly.4
One study among Chinese patients with nondialysis
chronic kidney disease (CKD)5 showed that nocturnal
BP was a significant risk factor for renal events and
cardiovascular events among these group of patients.
Renal events meant doubling of serum levels of
creatinine or end-stage renal disease, which ever
occurred first. Furthermore, studies also showed that
nocturnal BP was the most important determinant of all
the organ damages such as left ventricular hypertrophy,
microalbuminuria, carotid intima-media thickness.2,6-10
Therefore, nocturnal BP level is considered as a stronger predictor of cardiovascular morbidity and total
mortality than daytime BP.8,10-12
I sol a t ed NHT, whi ch i s de f ined a s dayt ime
normotension but with nocturnal elevated BP, is found
to be more prevalent in Chinese (10.9%) than in
Westerners (6.0%) and Eastern Europeans (7.9%).13,14
However, due to the difficulties to identify the
condition, the importance of isolated NHT is frequently
overlooked.2 Using the daytime clinic BP alone to guide
the antihypertensive treatment would therefore render
patients with isolated NHT at risk of poor BP control
and the subsequent development of cardiovascular
complications. Ambulatory blood pressure monitoring
(ABPM) has been reported to be a better predictor
for health outcomes than BP measured in clinic or at
home.15,16 Some studies showed that both daytime and
night time ambulatory systolic BP were better predictors
of all-cause and cardiovascular mortality than clinic BP
alone.15,17,18 In addition, it is the only method to offer
insights on patterns of nocturnal BP, therefore helps
identifying patients with NHT.19 Having said so, due to
limited resources, ABPM service could not be provided
for all patients. Usual indications for ABPM include
identifying white-coat HT, masked HT, abnormal 24-
hour BP patterns and assessment of treatment.20
Concerning the risk factors of NHT, studies
have shown that some conditions, such as older age,
diabetes, CKD, albuminuria, poor sleep quality such
as obstructive sleep apnoea (OSA), insomnia, nocturia,
depression, shift-working, etc. are associated with
the development of NHT.2,8,10,17,19,21,22 Once NHT is
identified, chronotherapy is suggested for these patients,
by taking hypertensive medication at night to restore
the normal circadian rhythm.10,23 This would be more
effective than morning administration, and could
improve the overall BP control. This is confirmed by a
local study showing that restoring the nocturnal BP dip
can improve left ventricular systolic ejection fraction
among Chinese patients.24
Up to now, there was no local data on the
prevalence of NHT and its associated risk factors
among Chinese patients managed in the primary care
setting. Locally, a significant proportion of hypertensive
patients are managed in primary care and followed up
at government General Out-patient Clinics (GOPCs) of
the Hospital Authority. In addition, the ABPM service
has been available to primary care clinics since 2012 to
improve the quality of care. To address this knowledge gap, we conducted this study and hopefully our findings
will provide important background information on the
prevalence of NHT in Chinese patients who undergo
ABPM and explore its associated risk factors.
Methods
Study Design:
Cross-sectional study carried out at public primary
care clinics
Subjects:
Inclusion criteria
All adult Chinese patients who underwent ABPM
in GOPCs of Kowloon Central Cluster from 1/12/2017
to 30/11/2018 and had annual blood and urine checkup
at least once during the study period were included.
Patients were referred to have ABPM due to the
following indications: suspected white coat HT, poorly
controlled or resistant HT or suspected masked HT. All
the devices for ABPM had been validated independently
by Biomedical Engineering Service Section (BESS)
yearly. In these clinics, hypertensive patients were
provided with blood and urine checkups at least
annually. This 1-year retrieval period was therefore
likely to cover all such patients regularly followed up in
these clinics. Annual blood checkup for all hypertensive
patients included renal function test with creatinine level,
fasting glucose and lipid profile. Routine urine checkup
included spot urine protein-creatinine ratio (PCR).
Urine albumin-creatinine ratio (ACR) would be done if
the patients were known to have diabetes mellitus (DM).
Inclusion criteria
-
Patients who were younger than 18-years-old.
-
Patients who were Non-Chinese in ethnicity.
-
Patients who worked night shift. Nurse would ask
whether patients had night shift duty before ABPM.
Such patients would be identified and excluded.
-
Patients who were intolerant to ABPM or the
ABPM data was invalid.
-
Patients who had no blood or urine checkup during
the study period.
ABPM and definition of nocturnal hypertension:
ABPM measures patients’ BP during a 24-hour
period. ‘ABPM daytime’ and ‘ABPM nighttime’
were defined according to patients’ schedules. ABPM provides a more accurate assessment with respect to
clinic BP. A valid ABPM result should have at least 70%
of expected measurements.20 The minimum of daytime
measurements should not be <20, with a minimum of
7 measurements at night. All patients who underwent
ABPM were asked about the sleep time and awake
time and these data were entered into ABPM software
(cardiovisions 1.16.6). They were advised not to do
vigorous exercise. Awake BP readings were measured in
30-minutes interval. Night time readings were measured
in 45-60-minutes interval, depending on total number of
sleeping hours so minimum of 7 measurements would
be achieved at night. Nocturnal dipping status and
whether patients got daytime HT were also retrieved
from the report. Dipper was defined as the difference
between daytime mean systolic pressure and nighttime
mean systolic pressure greater than or equal to 10%.25
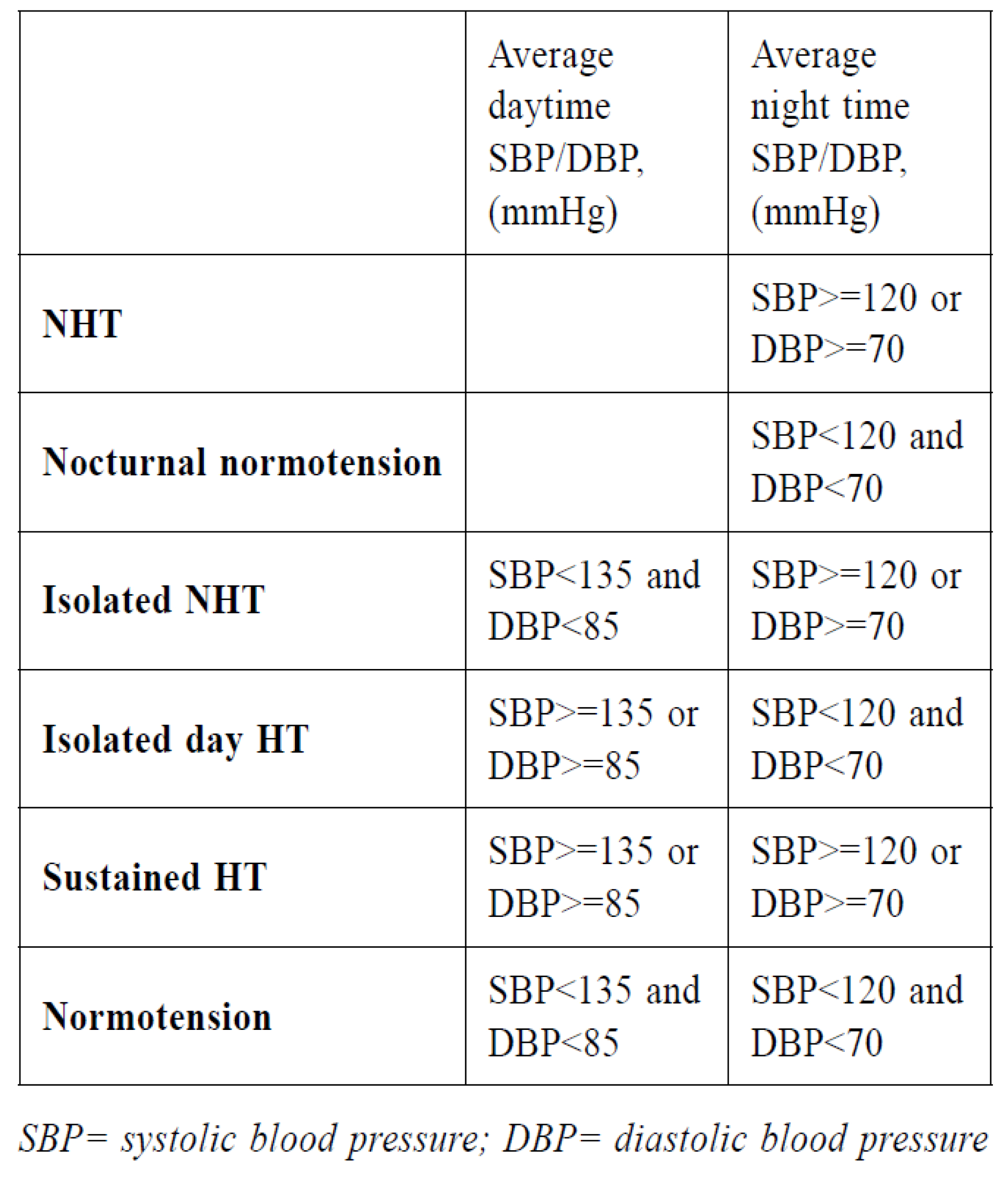
According to European Society of Hypertension26:
definition of NHT, nocturnal normotension, isolated
NHT, isolated day HT, sustained HT and normotension
were as followed:
Determination of variables:
All relevant clinical data were retrieved from the
Clinical Management System (CMS) of the Hospital
Authority. It included patient demographics such as age,
gender, body mass index (BMI), smoking and drinking
status; comorbidities such as DM, cardiovascular diseases (including stroke, ischemic heart disease,
or peripheral vascular disease), conditions which
may affect sleep such as mood problems (including
depression, anxiety disorder), benign prostate
hypertrophy (BPH) and OSA; laboratory data such as
serum creatinine levels, estimated glomerular filtration
rate (eGFR), urine ACR or spot urine PCR, serum
fasting glucose, lipid profile, clinic BP and current
treatment (receiving how many antihypertensive drugs,
any bedtime hypertensive drugs) etc. If more than
one test had been done, the blood and urine test done
closest to the date of ABPM was used for data analysis.
For clinic BP, patients were advised to measure BP
after at least 10-minutes of rest in the outpatient clinic.
The clinic BP reading on date of referring for ABPM
was used in data analysis. Obesity was defined as BMI
≥25kg/m2. Microalbuminuria was defined as urine ACR
being 2.5 to 30mg/mmol for males and 3.5 to 30mg/
mmol for females. Proteinuria was defined as urine
ACR being >30mg/mmol or urine PCR >50mg/mmol
for both genders.27 An elevated urine ACR and PCR
needed to be confirmed in the absence of urinary tract
infection with additional first-void specimens collected
during the next 3 to 6 months. CKD was defined as
having an eGFR of <60mL/min/1.73m2. Patient was
considered a smoker if currently smokes or was within
the first six months of quitting.
Sample Size Estimation:
According to the literature , the prevalence
of isolated NHT was around 10.9% in Chinese
population.13 Currently there are about 100,000 HT
cases in our cluster. Assuming a prevalence of 10.9%
patients who performed ABPM having NHT, with
5% margin of error and 95% confidence level, the
sample size required is 150 (calculated via the statistic
calculator).28 To allow the room for case exclusion
(around 30%), a sample size of 230 was decided for
this study. Each ABPM case done within this period
was assigned with a case number. Random Selection
Generator was used to randomly select the case number
and recruited into the study.29
Statistical Analysis:
All data were entered and analysed using computer
software (Windows version 21.0; SPSS Inc, Chicago
[IL], US). Student’s t-test and analysis of variance were
used for analysing continuous variables. Chi square test
was used for categorical data and if the sample size is small (<5), Fisher's Exact test was used. All statistical
tests were two sided, and a P-value of less than 0.05
was considered significant.
Results
A total of 348 cases had performed ABPM during
the study period in the GOPCs of the Kowloon Central
Cluster (KCC), among which 230 cases were randomly
selected for this study. Further review of the data
showed 68 cases (29.6%) did not fulfill the inclusion
criteria and were therefore excluded. These patients
included 1 case who was younger than 18 years old,
1 case that was not Chinese, 17 cases with invalid
ABPM result, and 49 cases (21.3%) did not have blood
and urine checked during the study period. Thus, the
remaining 162 patients (70.4%) fulfilling the inclusion
criteria were included into the data analysis.
Figure 1 summarised the flow chart of case
recruitment and the ABPM diagnosis of the patients
included in this study. From the data, we can see that,
among the 162 patients included, 106 cases were found
to have NHT, giving a period prevalence of 65.4%. In
addition, 17 cases were found to have isolated NHT,
with a period prevalence of 10.5%.
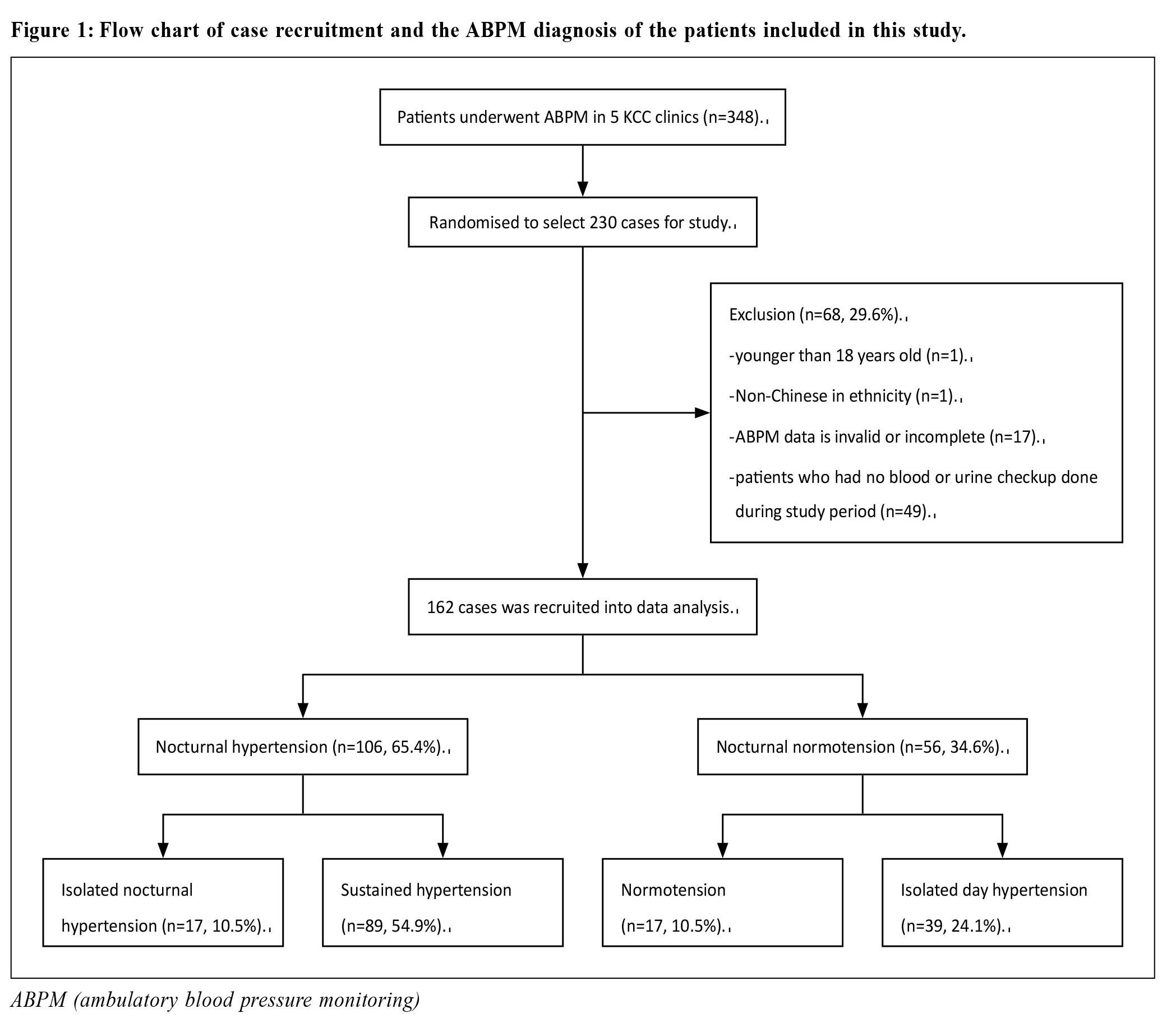
Table 1 summarised the demographic characteristics
of all patients categorised according to the four
ambulatory BP patterns. Basic demographic data revealed
that the mean age of these groups of patients was 64.8
+/- 13.4 years old, and 63 were male (38.9%). Patients
with sustained HT, isolated NHT and isolated day HT
were older than the normotension group, with their mean
age being 65.8 +/- 13.3 years, 61.1 +/- 14 years, 67.1
+/- 12.9 years respectively versus 57.5 +/- 12.4 years
(p=0.044). Their gender composition, BMI, proportion of
smoker and drinkers were comparable.
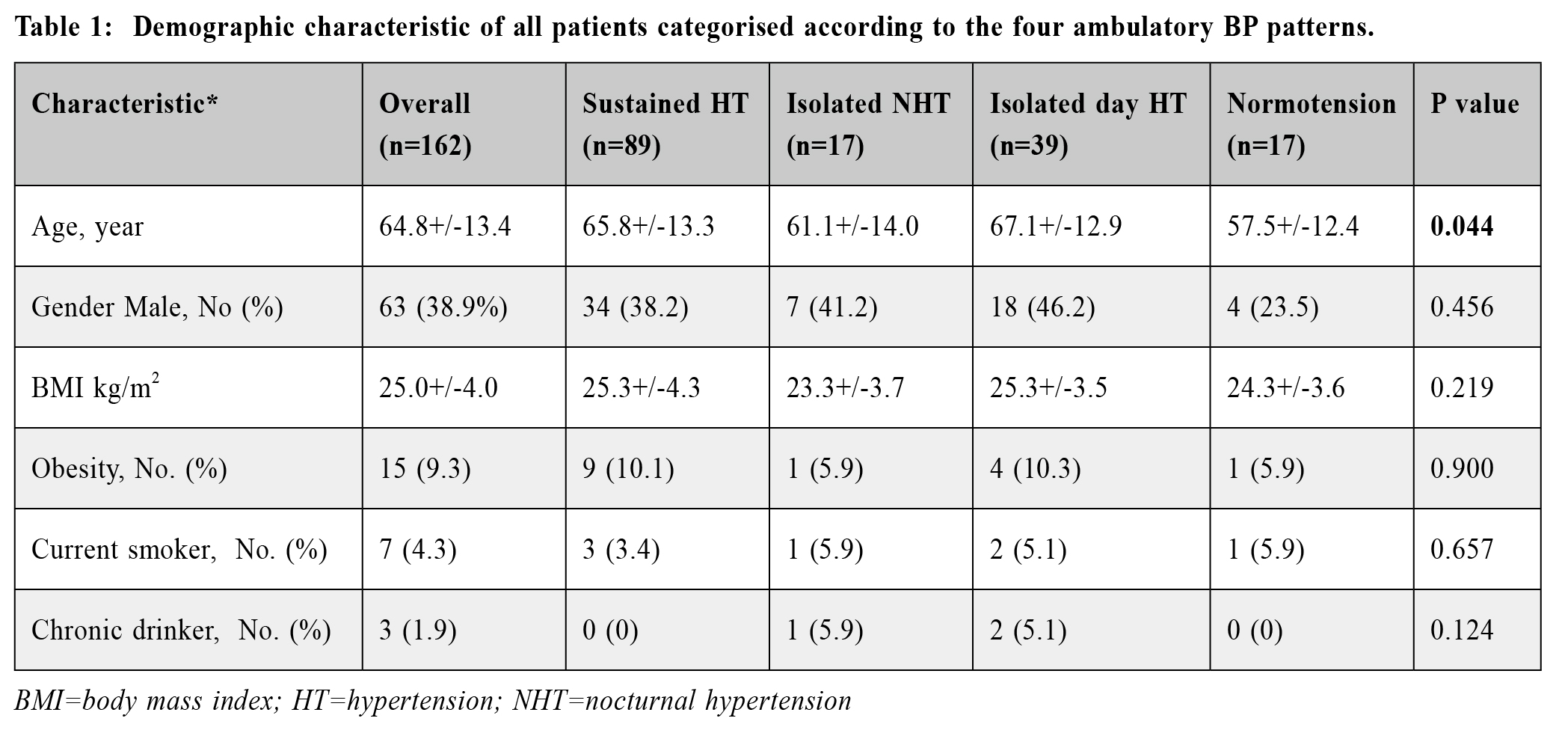
Table 2 summarised the demographic characteristics
of the patients with or without NHT. In summary, they
were comparable in terms of age, male-to-female ratio,
smoking status, and BMI (all p>0.05).
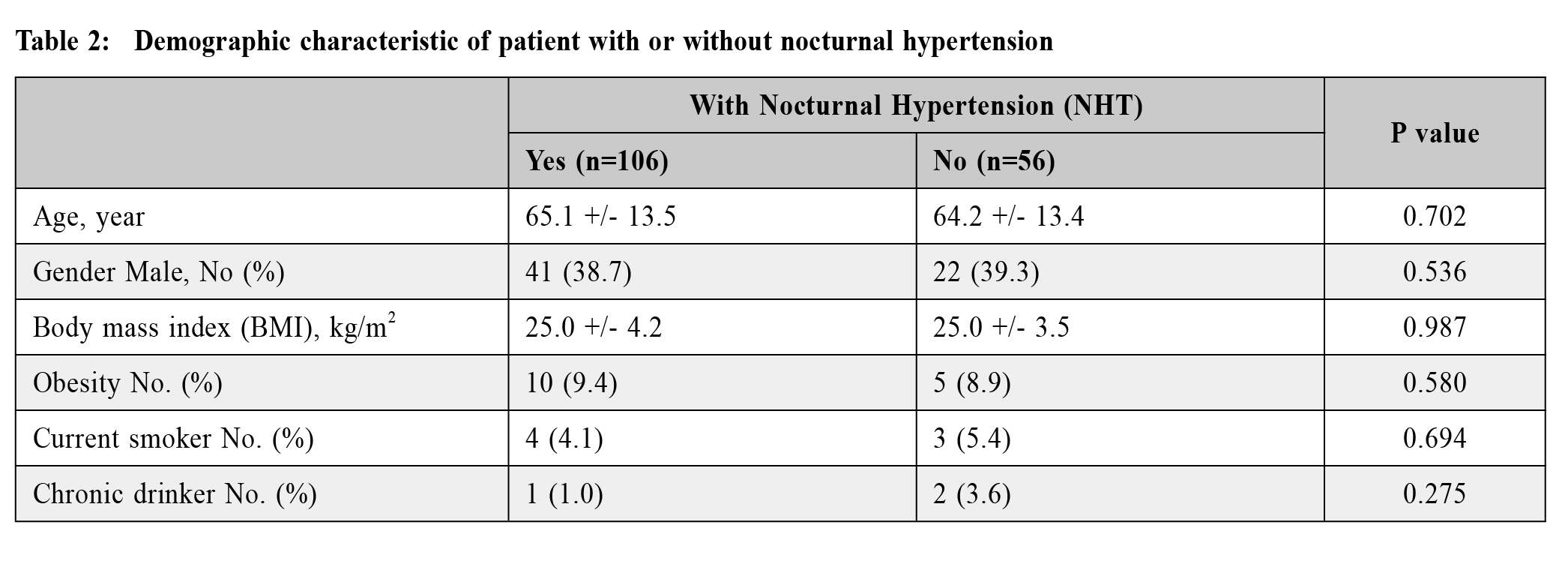
Table 3 summarised the comorbidities and ABPM
reading of patients with or without NHT. Compared
with nocturnal normotension group, NHT group was
found to have higher proportion with daytime HT (84%
vs 69.6%, p=0.043). Not surprisingly, the average
night time SBP and DBP were both much higher than
the nocturnal normotension group (both p<0.001). In addition, NHT group was found to have fewer dippers
(25.5%) than the nocturnal normotension group (60.7%),
with p<0.001. The comorbidity rates for stroke, ischemic
heart disease (IHD), DM, CKD, mood problem,
BPH, OSA were all similar (all p>0.05). Number
of antihypertensive medication used and whether
patient was on bedtime antihypertensive were not
statistically significantly different either (all p>0.05).
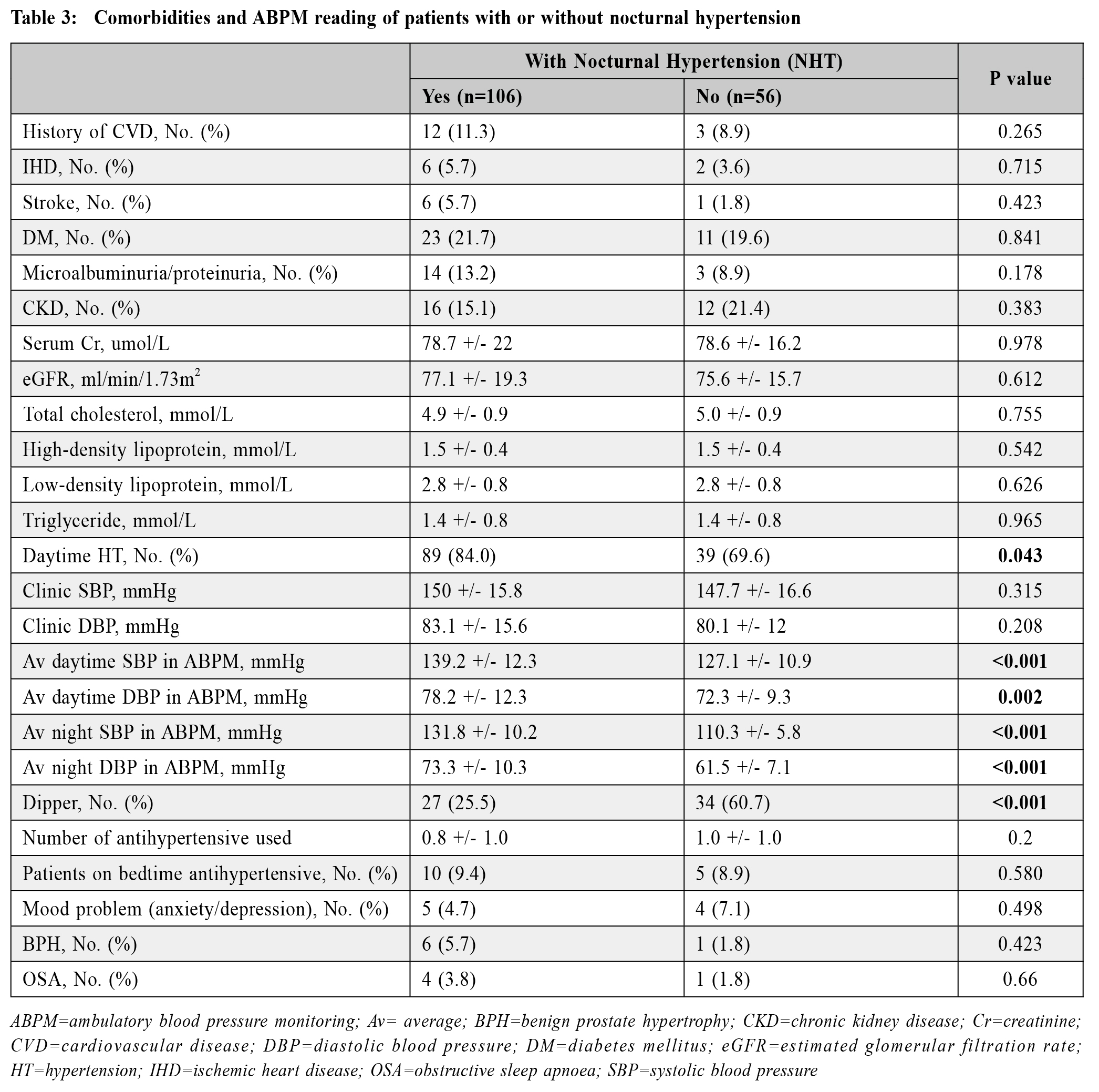
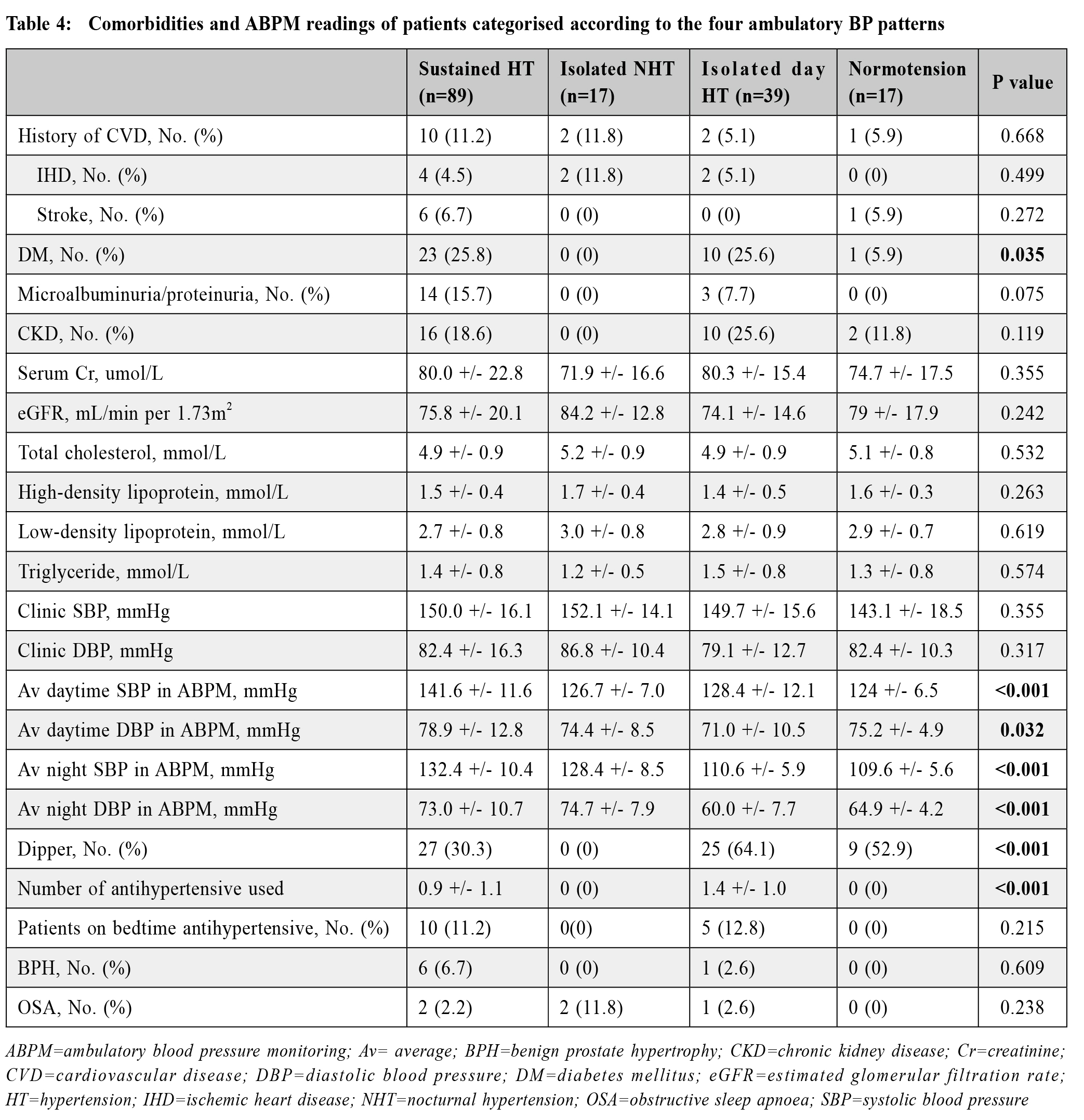
Table 4 summarised the comorbidities and ABPM
readings of patients categorised according to the four ambulatory BP patterns. The sustained HT group and
isolated day HT group were found to have higher
proportion with DM (25.8% and 25.6% respectively,
vs 0% for isolated NHT and 5.9% for normotension
group, p=0.035). Isolated day HT and normotension
group were found to have more with dipper (64.1%
and 52.9% respectively) whereas isolated NHT group
was found to have lowest dipper rate (0%, p<0.001).
The lipid profile and comorbidity rates for stroke, IHD,
microalbuminuria/proteinuria, CKD, mood problem,
BPH, OSA were all similar (all p>0.05).
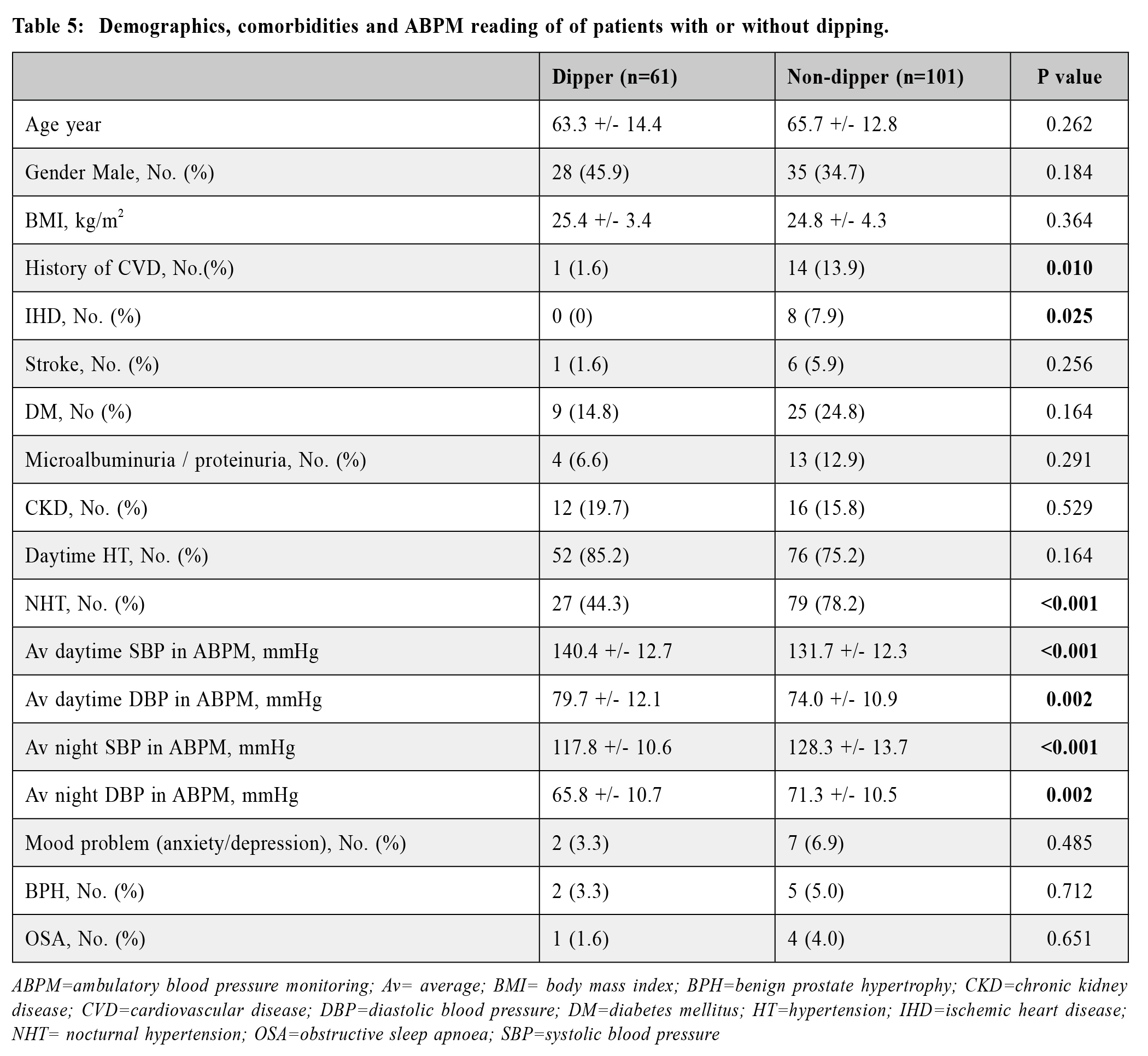
We further analysed the demo graphics,
comorbidities and ABPM reading of patients with or
without dipping (Table 5). In summary, they were
comparable in terms of age, male-to-female ratio, and
BMI (all p>0.05). Non-dippers were found to have
higher proportion with IHD (7.9% vs 0%, p=0.025) and
NHT (78.2% vs 44.3%, p<0.001) versus the dippers.
The comorbidity rates for stroke, DM, CKD, mood
problem, BPH, OSA were similar (all p>0.05).
Discussion
Our study revealed that the prevalence of NHT
among hypertensive patient undergone ABPM was
65.4%. In primary care, ABPM is usually indicated for suspected whitecoat hypertension or resistant
hypertension. The high prevalence of NHT in our
study subjects is likely contributed by the patients with
resistant hypertension. Among those with NHT, the
prevalence of isolated NHT was 10.5%. It was well
known that ethnic diversity exists in diurnal BP patterns,
possibly due to different genetic background, lifestyle,
or both.13 In addition, it was noted that patients with
isolated NHT were much younger than those with
isolated day HT or sustained HT, but was older than
those with normotension (Table 1). With regards to
the comorbidities, our data indicated that patients with
NHT had a higher chance of daytime HT and being
non-dippers too (Table 3). These findings should alert
physicians to the importance of both daytime and nocturnal BP control and pay particular attentions to
the non-dippers. During our daily practice, we usually
started once daily dose of antihypertensive to patients
and advised the patients to take the medication in the
morning. If patients were identified to have NHT, an
addition of night time dose of antihypertensive would
be advised so as to improve the overall BP control.
Similarly, for isolated NHT case, the patient should be
advised to take the antihypertensive before the sleep.
Indeed, studies had confirmed that taking hypertensive
medication at night time could improve the overall BP
control and reduce HT complication rate.23 Therefore,
all HT patients should be advised to have both day time
and nocturnal BP monitoring either by ABPM or home
BP monitoring so that doctors could advise them the
treatment as appropriate. In this regard, monitoring
clinic BP or daytime home BP alone was considered
inadequate. All doctors should also pay special attention
to the diurnal patterns of different HT and make all
efforts to make sure that both the daytime and night
time HT are under control.
Isolated NHT is a very easily missed clinical
condition when only daytime BP or clinic BP is
monitored. Our study revealed that the prevalence
of isolated NHT was 10.5%, which was not low. In
addition, all isolated NHT group was found to be non-dipper
(Table 4) and the non-dipper cases were found
to have higher proportion with IHD (Table 5). As non-dipper
had been shown to be associated with higher
mortality and cardiovascular events12, all doctors should
pay special attention to the presence of isolated NHT
and make every effort to identify them early by using
either the ABPM or regular home BP monitoring before
sleep. In a recent study comparing self-measured home
BP (HBP) and ABPM, the evening BP before sleep was
similar between measured by home BP and ABPM. The
BP before sleep was on average 10 mmHg lower than
daytime BP and close to nocturnal BP.30 Since ABPM
might not readily available in some clinic setting, home
BP before sleep may be considered as a surrogate of
nocturnal BP and suboptimal home BP before sleep
could be an indication for ABPM.
ABPM request repeated measures of BP. It is reasonable to concern about the possible sleep
disturbance secondary to the frequent blood pressure
measurement and the sleep disturbance might affect the
interpretation of nocturnal BP. In our study, enrolled
patients did not particularly complain sleep disturbance caus ed by ABPM. A recent study compared the
nocturnal BP between sleep and awake state, showing
no significant difference regardless patient was asleep
or not.30
As to the aetiology of NHT, it was multifactorial.
Some studies had shown that it was commonly
encountered with a number of clinical backgrounds,
such as autonomic dysfunction, volume overload
secondary to salt sensitivity and CKD, poor quality
of sleep, disruption of biological circadian rhythms
and other factors.14 However, risk factors proved to be
associated with the presence of NHT in other studies,
including older age, the presence of diabetes, CKD,
albuminuria, or with poor sleep quality2,8,10,17,19,21,22
were not significantly different in the dipper versus
non-dipper group in our study. The reasons for this
discrepancy could be explained by the difference in their
racial or ethnic compositions. In addition, the clinic
setting was also different, with many of such studies
were carried out in secondary care settings whereas our
study was carried out in the primary setting. We had to
admit that the sample size of our study was relatively
small (n=162), which may limit the power to detect
the significant difference between the groups. In our
recruited patients, only 15 patients were found to have
cardiovascular disease (CVD) including IHD and stroke,
and even fewer number of patients got OSA, BPH, or
mood problem. Indeed, most patients managed in the
primary care were relatively more stable with fewer
complications and therefore had a lower prevalence of
CVD compared with those managed in secondary or
tertiary settings. Furthermore, some patients had already
received treatment for different comorbidities such
as antihypertensive for HT, lipid lowering agent for
hyperlipidaemia or continuous positive airway pressure
for OSA. Improvement of these conditions might also
affect the prevalence of NHT or isolated NHT.
Nocturia due to lower urinary tract symptoms
(LUTS) might affect sleep quality than thus affect
the nocturnal BP. In our study, only 7 out of 63
male subjects have BPH, which might not affect the
interpretation of data. The prevalence of BPH in our
study was 11%, this was similar to literature. In a study
about LUTS in Chinese male patients, the prevalence
of LUTS among men aged beyond age 50 years was
10.66%. Prevalence in age group 50-59 was 8.39%, and
10.61%in age group 60-69, 14.7% in age group >=70.31
Strength and limitations of the study
This was the first local study on the prevalence of
NHT and its associated risk factors in the primary care
setting. In addition, the ABPM readings, the clinical
data and the biochemical data were all retrieved from
the CMS system of the Hospital Authority, therefore not
much human error or recall bias.
However, several limitations existed in this study.
First, this was a single cluster study and only patients
who had performed ABPM were recruited, therefore
selection bias existed. Also, the sample size was small,
this might affect the significance of data. In this study,
most patients were referred to have ABPM due to the
following indications: suspected white coat HT, poorly
controlled or resistant HT or suspected masked HT.
Therefore, our study findings may not be generalised
to other settings or to the general population. Second,
49 case (21.3%) who did not have blood or urine
assessments done were excluded, which may affect the
genuine prevalence rate of NHT in the study. It is well
observed in our daily practice that those patients who
do not attend routine blood or urine tests tend to have
poor compliance to regular follow up and taking regular medications. Therefore, the exclusion of these groups
of patient would likely result in under-estimation of the
prevalence rate of NHT. Third, because of the crosssectional
nature of our study, we were unable to adjust
for other potential unmeasured confounders e.g. quality
of sleep during ABPM, frequency of nocturia. Therefore
no temporal or causal relationship could be established.
Implications for primary care
Family physicians are at the forefront in the
management of HT, and aim to achieve optimal BP
control to prevent cardiovascular complications. This
study has provided important background information
on the high prevalence of NHT among Chinese patients.
Physicians should stay alert on it and promote the use
of ABPM to identify this group of patients. If patients
are identified to have NHT, adding a night time dose of
antihypertensive would be advised so as to improve the
overall BP control and reduce its complication rate.
Future studies using a prospective randomised
clinical trials would help to address some of the
limitations of this study. Also, considerations should be
given to future studies identifying the role of NHT in
mortality and its prognostic value.
Conclusion
In summary, our study suggested that NHT was a
common condition, with a period prevalence of 65.4%.
NHT cases were found to have a higher reading of
average daytime and night time BP and more NHT cases
were non-dippers. In addition, non-dipper patients were
found to have higher proportion with IHD and NHT
than the dippers. Family physicians should enhance the
awareness on the presence of NHT and non-dippers
during management of HT in daily practice. Concerted
effort should be made to bring both the daytime and
night time BP down to target level and therefore prevent
the development of CVD.
Acknowledgement
I sincerely thank my supervisors Dr. Catherine Chen
and Dr. Ken Ho for their continuous encouragement,
inspiration, and support during this study. I would
also like to thank Mr. Steven Lau, statistical officer of
Kwong Wah Hospital, Kowloon Central Cluster for his
expert statistical support.
References
-
Centre for Health Protection, Department of Health, Hong Kong SAR
Government. Report of Population Health Survey 2014/15. Available from:http://www.chp.gov.hk/en/static/51256.html.
-
Kario K. Essential manual of 24 hour blood pressure management: from
morning to nocturnal hypertension. p. p.
-
Li Y, Wang JG. Isolated nocturnal hypertension: a disease masked in the
dark. Hypertension. 2013;61(2):278-283.
-
Yano Y, Inokuchi T, Hoshide S, et al. Association of poor physical function
and cognitive dysfunction with high nocturnal blood pressure level in
treated elderly hypertensive patients. American journal of hypertension.
2011;24(3):285-291.
-
Wang C, Li Y, Zhang J, et al. Prognostic Effect of Isolated Nocturnal
Hypertension in Chinese Patients With Nondialysis Chronic Kidney Disease.
Journal of the American Heart Association. 2016;5(10).
-
Cuspidi C, Facchetti R, Bombelli M, et al. Nighttime blood pressure and
new-onset left ventricular hypertrophy: findings from the Pamela population.
Hypertension. 2013;62(1):78-84.
-
Cuspidi C, Sala C, Valerio C, et al. Nocturnal hypertension and organ
damage in dippers and nondippers. American journal of hypertension.
2012;25(1)(8):869-875.
-
de la Sierra A, Gorostidi M, Banegas JR, et al. Nocturnal hypertension or
nondipping: which is better associated with the cardiovascular risk profile?
American journal of hypertension. 2014;27(5):680-687.
-
Tadic M, Cuspidi C, Pencic-Popovic B, et al. The influence of nighttime
hypertension on left ventricular mechanics. International journal of
cardiology. 2017;243:443-448.
-
Yano Y, Hayakawa M, Kuroki K, et al. Nighttime blood pressure, nighttime
glucose values, and target-organ damages in treated type 2 diabetes patients.
Atherosclerosis. 2013;227(1):135-139.
-
Ben-Dov IZ, Kark JD, Ben-Ishay D, et al. Predictors of all-cause mortality
in clinical ambulatory monitoring: unique aspects of blood pressure during
sleep. Hypertension. 2007;49(6):1235-1241.
-
Hansen TW, Li Y, Boggia J, et al. Predictive role of the nighttime blood
pressure. Hypertension. 2011;57(1):3-10.
-
Li Y, Staessen JA, Lu L, et al. Is isolated nocturnal hypertension a novel
clinical entity? Findings from a Chinese population study. Hypertension.
2007;50(2):333-339.
-
Yano Y, Kario K. Nocturnal blood pressure and cardiovascular disease: a
review of recent advances. Hypertension research: official journal of the
Japanese Society of Hypertension. 2012;35(7):695-701.
-
Banegas JR, Ruilope LM, de la Sierra A, et al. Relationship between Clinic
and Ambulatory Blood-Pressure Measurements and Mortality. The New
England journal of medicine. 2018;378(16):1509-1520.
-
Stergiou GS, Asayama K, Thijs L, et al. Prognosis of white-coat and masked
hypertension: International Database of Home blood pressure in relation to
Cardiovascular Outcome. Hypertension. 2014;63(4):675-682.
-
Boggia J, Li Y, Thijs L, et al. Prognostic accuracy of day versus night
ambulatory blood pressure: a cohort study. Lancet. 2007;370(9594):1219-1229.
-
Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of
ambulatory blood-pressure recordings in patients with treated hypertension.
The New England journal of medicine. 2003;348(24):2407-2415.
-
O'Brien E, Dolan E. Ambulatory Blood Pressure Monitoring for the Effective
Management of Antihypertensive Drug Treatment. Clinical therapeutics.
2016;38(10):2142-2151.
-
Parati G, Stergiou G, O'Brien E, et al. European Society of Hypertension
practice guidelines for ambulatory blood pressure monitoring. Journal of
hypertension. 2014;32(7):1359-1366.
-
Iannucci G, Petramala L, La Torre G, et al. Evaluation of tolerance to
ambulatory blood pressure monitoring: Analysis of dipping profile in a large
cohort of hypertensive patients. Medicine. 2017;96(50):e9162.
-
Wang C, Deng WJ, Gong WY, et al. Nocturnal Hypertension Correlates Better
With Target Organ Damage in Patients With Chronic Kidney Disease than a
Nondipping Pattern. Journal of clinical hypertension. 2015;17(10):792-801.
-
Kristanto A, Adiwinata R, Suminto S, et al. Nocturnal Hypertension:
Neglected Issue in Comprehensive Hypertension Management. Acta medica
Indonesiana. 2016;48(1):76-82.
-
Ko GT, Chan HC. Restoration of nocturnal dip in blood pressure is associated
with improvement in left ventricular ejection fraction. A 1-year clinical study
comparing the effects of amlodipine and nifedipine retard on ambulatory blood
pressure and left ventricular systolic function in Chinese hypertensive type 2
diabetic patients. International journal of cardiology. 2003;89(2-3):159-166.
-
Bloomfield D, Park A. Night time blood pressure dip. World journal of
cardiology. 2015;7(7):373-376.
-
Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines
for the management of arterial hypertension. European heart journal.
2018;39(33):3021-3104.
-
Management of diabetes. Scottish Intercollegiate Guidelines Network.
Edinburgh: SIGN; 2010.
-
Select statistical services. 2022. Retrieved from https://select-statistics.co.uk/calculators/sample-size-calculator-population-proportion/
-
Random Integer Generator. 1998-2022. Retrieved from https://www.random.org/integers/
-
Hosohata K, Kikuya M, Asayama K, et al. Comparison of nocturnal blood
pressure based on home versus ambulatory blood pressure measurement: The
Ohasama Study. Clin Exp Hypertens. 2020;42(8):685-691.
-
Zhang W, Zhang X, Li H, et al. Prevalence of lower urinary tract symptoms
suggestive of benign prostatic hyperplasia (LUTS/BPH) in China: results
from the China Health and Retirement Longitudinal Study. BMJ Open.
2019;9(6):e022792.
Hing-han Chen,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Resident Specialist,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority Hong Kong
Ka-ming Ho,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Consultant,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority Hong Kong
Yim-chu Li,
MBBS, FHKCFP, FRACGP, FHKAM (Family Medicine)
Chief of Service and Consultant,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority Hong Kong
Catherine XR Chen,
MRCP(UK), PhD(Med, HKU), FRACGP, FHKAM (Family Medicine)
Consultant,
Department of Family Medicine & General Outpatient Clinic, Kowloon Central Cluster,
Hospital Authority, Hong Kong.
Correspondence to:
Dr. Hing-han Chen, Room 807, Block S, Queen Elizabeth Hospital,
30 Gascoigne Road, Kowloon, Hong Kong SAR.
E-mail: chh729@ha.org.hk
|
