June 2008, Vol 30, No. 2 |
Original Articles
|
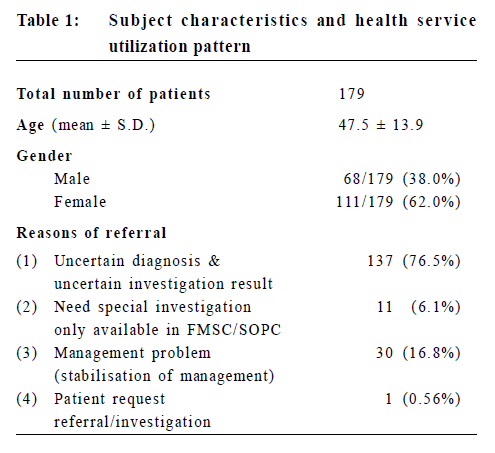
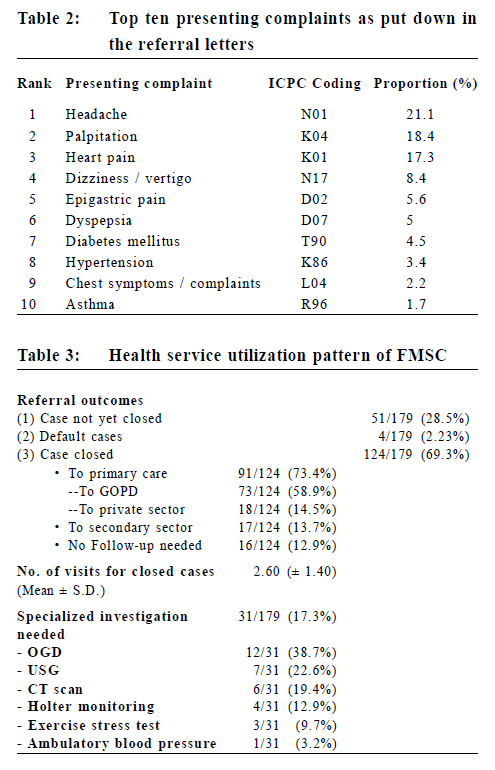
Collaboration between Family Medicine and Internal Medicine - a new model of care for effective primary care*Martin C S Wong 黃至生, Alvin C Y Chan 陳鍾煜, Wai-keung Kwan 關煒強, S W Mercer, S M Griffiths 葛菲雪, Yuk-kwan Yiu 姚玉筠 HK Pract 2008;30:60-69 Summary Objective: The Family Medicine Specialist Clinic (FMSC) of the Yan Chai Hospital (YCH) has been developed as a new model of health care delivery. The present study examined the efficiency of our FMSC model in managing referrals from the Accident and Emergency Department (AED) and studied the predictors of service utilization in this new FMSC model. Design: Retrospective descriptive study. Subjects: All cases referred from AED to FMSC of the Yan Chai Hospital were included from November, 2005 to February, 2007. Main outcome measures: Outcome variables include the average number of consultations, referrals for specialized investigation, case discharge to the primary care sector and case closing within the study period. These health services outcomes were examined according to age and gender. Results: There were 179 patients recruited from AED to FMSC. The most common reason for referral was uncertain diagnosis (76.5%). Only 17.3% of all referred cases had specialized investigations done. Of the 179 patients, 124 (69.3 %) cases were closed after a mean of 2.60 visits to FMSC. Among the cases which were closed, 91 (73.4%) were referred back to the primary care sector. Only 17 (13.7%) needed secondary care specialist referrals. Patients discharged back to the primary care sector were older (48.6 vs 42.7 year-old, p=0.049) as were those requiring specialized investigations (53.5 vs. 46.0 year-old, p=0.050). Conclusion: This new FMSC model of care has demonstrated that the majority of patients referred from AEDs can be managed in the primary care setting. These results imply an efficient means of enhancing integration of primary health care in Hong Kong. Further studies could be conducted to assess the cost-effectiveness of this FMSC model. Keywords: Family Medicine Specialist Clinic, Health Care Model, Efficiency (*This article represents a modification of a paper presented at the 30th Annual Scientific Meeting, The Hong Kong College of Family Physicians.) 摘要 目的:仁濟醫院的家庭醫學專科門診已發展為一種新的醫療服務模式。本研究檢視這種模式在診治由急症室轉介個案的成效,並研究使用這服務的可預測因素。 設計:回顧描述形式。 對象:由2005年11月至2007年2月所有由急症室轉介到仁濟醫院家庭醫學專科門診的病人。 主要測量內容:結果變數包括在研究時段內的平均求診次數,專科檢驗轉介,病人轉介到基層醫療部門以及無須再覆診個案。這些醫療服務結果是按照年齡及性別加以分析。 結果:共179位病人由急症室轉介到家庭醫學專科門診。其主要原因是未能確定診斷〔76.5%〕。只有17.3%的個案曾接受專科檢查。在179位病人中,124人〔69.3%〕於家庭醫學專科門診,經平均應診2.6次後無須再覆診。在無須覆診人士中,91人〔73.4%〕被轉介回基層醫療,只有17人〔13.7%〕需要公共醫療專科轉介。被轉介回基層醫療的病人為較年長的(48.6歲對比42.7歲,p=0.049)並和那些需要專科檢查病人相同(53.5歲對比46歲,p=0.050)。 結論:這種新的家庭醫學專科門診服務模式顯示大部份由急症室轉介的病人皆可以於基層醫療進行診治。這些結果示意一項有效加強基層醫療融合的方式,並可進一步為這模式的成本效益作研究。 主要詞彙:家庭醫學專科門診,醫療照顧模式,效率 Introduction The importance of a comprehensive primary health care system has been highlighted more than a decade ago when the work of Starfield1 provided substantial evidence for the concept of primary care as the foundation for a healthcare system. Her eleven-nation study showed the clear superiority of health systems with a primary care orientation - namely the achievement of better health levels, higher satisfaction with health services among their populations and overall lower costs of services. This is in line locally with a more recent Governmental proposal for a new health care delivery model by the Health and Medical Development Advisory Committee (HMDAC). It emphasizes the need for primary health care to take up more functions and responsibilities in health services2,3 including preventive, medical and rehabilitative care for the population. The implementation of a system involving more extensive primary care components must be matched by well-trained family doctors. Substantial evidence shows that public health burdens could be relieved by high quality Family Medicine (FM).4-6 It has been shown that family doctors are more selective in their investigations,7 manage problems at an earlier stage, resulting in a lesser use of hospital emergency services8 and admissions.9 Problems are managed at an earlier stage, reducing the need for expensive treatments for late complications.10 Also, there has been evidence showing that an increase in the family doctor to general population ratio may result in a decrease in mortality, health care costs, and an earlier diagnosis of cancers.5-8,11 Indeed, many studies revealed that family doctors can handle over 90% of all health problems in the community.9-10,12-13 No doubt an efficient gate-keeper role should be one important feature of a cost-effective primary care system. However, the public primary care sector in Hong Kong is not equipped with facilities and systems allowing efficient gate-keeping. Among the major reasons for referral are the absence of investigative tools in primary care and the lack of expertise. Currently, all patients who are referred to the public secondary care sector are likely to be reviewed by a secondary care specialist with loss of continuity of care from the primary care sector. This makes provision of comprehensive, holistic and continuing care difficult, and imposes a major barrier for implementation of high-quality primary care even in the presence of well trained and highly qualified family doctors. A new model of primary care has been developed in the Family Medicine Specialist Clinic (FMSC) of Yan Chai Hospital (YCH) since 2005. It represents a collaborative initiative between the Department of Family Medicine & Primary Health Care, Kowloon West Cluster (KWC) and the Department of Medicine, Yan Chai Hospital. A system has been in place targeting all routine patient referrals (third priority, or P3) to Medical Specialist Out-Patient Clinics (SOPCs). The distinguishing features of this FMSC model include (1) direct access to multiple specialized investigation tools supported by the Medical Unit; (2) joint triaging system by the medical and FM specialists; and (3) control of case selection to the FMSC by the FM specialists. The investigation tools operated and supported by the Medical Unit include Oesophago-Gastro-Duodenoscopy, treadmill, Holter, and ambulatory blood pressure monitoring. For the joint triaging system, all the referrals to the Medical Unit, from whatever sources, will be screened first by the medical physicians as usual, and then the P3 referrals will be further screened by the family physicians. The family physicians have the final discretion regarding whom would be seen and followed up by the FMSC. A recent study by Ng and Yiu14 analyzed the case load, disease profile and the outcomes of patients seen in four Family Medicine Specialist Clinics (FMSCs) and encouraging results were reported. The FMSCs managed a large variety of uncomplicated conditions in internal medicine with a significantly shorter waiting time, undoubtedly a brilliant first step towards creating an intact and effective primary health care system. The present study aims to substantiate the above study by further analyzing all those referrals from Accident and Emergency Department (AED), and the various predictors of health service utilization in this new model. The results will then act as useful information sources for policy-makers and physicians to address and identify rooms for improvement in this new model of primary care. Referrals from AED represent significant referrals to the YCH Medical Department and have been analysed in this study, and the YCH FMSC managed the triaged referrals. This represented successful collaboration between the two departments. Methods A consecutive cohort of all patients referred from AED to the YCH FMSC was recruited during the period November, 2005 to February, 2007. Patient demographics and information regarding health services were recorded and analyzed using the Statistical Package for Social Sciences (SPSS) version 11.0. The numbers of case closed, defaulted or still under health care were studied. Among the cases closed, the main outcome measurements included (1) the discharge rates back to the primary care sector including public (GOPCs) and private doctors; (2) the proportion of referrals requiring specialized investigations not available in GOPCs; (3) the proportion of referrals requiring public secondary care specialist management in clinics under the Hospital Authority; (4) the main reasons for referral; and (5) the mean number of visits to the FMSC before discharge. All these dependent variables for those cases closed were compared between the 2 different gender groups. The mean patient age of attaining (vs. not attending) these outcomes was also analyzed. Student's t-test was used for comparison between continuous variables and chi-square test of homogeneity for categorical variables. A p value <0.05 (two-sided) was regarded as statistically significant. Results Subject characteristics and overall health service utilization The AED referrals represented 22% of all P3 referrals to the YCH Medical Unit. During the study period, we collected 179 patient referrals from the AED to the YCH FMSC (Table 1), representing about 35% of all AED P3 referrals to the YCH Medical Unit. These 179 cases also represented 32.6% of all the YCH FMSC patients seen in the study period. The mean age was 47.5 year-old and the male gender consisted of 38%. The major reasons for referral were uncertain diagnosis (76.5%), followed by management problem (16.8%) and need for specialized investigation (6.1%). The top 10 presenting complaints as laid down in the referral letters are shown in Table 2. Majority of them were vague, undifferentiated symptoms.
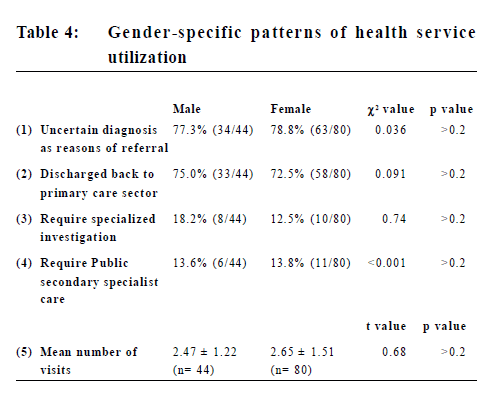
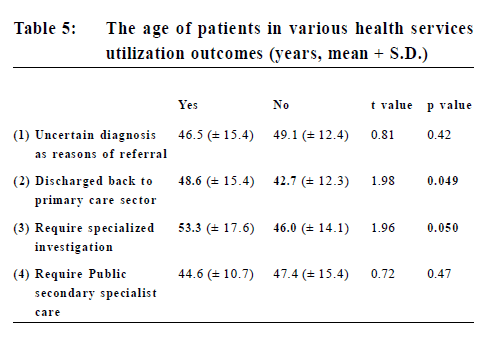
Of the 179 patients, 124 (69.3 %) cases were closed (Table 3) after a mean of 2.60 visits to FMSC. Among cases closed, 18 (14.5%) cases were referred back to private doctors, 73 (58.9%) to GOPCs, and 16 (12.9%) required no further follow up, i.e. 91 cases (73.4%) were discharged to the primary care sector. Only 17 patients (13.7%) needed public secondary care specialist referrals for further management. Only 17.3% of all referred cases had special investigations done. The main investigations were Oesophago-Gastro-Duodenoscopy (OGD) (38.7%), Ultrasound (22.6%), Computed Tomography (19.4%), Holter monitoring (12.9%), Treadmill (9.7%) and Ambulatory Blood Pressure Monitoring (ABPM) (3.2%). Gender-specific patterns of health service utilization Marginally more male patients were discharged back to the primary care sector (75.0% vs. 72.5%) and required specialized investigations (18.2% vs. 12.5%) than female patients (Table 4). The proportion of patients having ?ncertain diagnosis as reasons for referral" (77.3% vs. 78.8%) and those required public secondary specialist care (13.6% vs. 13.8%) were very similar for both genders. None of these comparisons reached statistical significance (p>0.2).
Female patients had a slightly greater number of visits than male patients (2.65 vs. 2.47 times), but again this difference was not statistically significant (p=0.50). Age of patients in health service utilization outcomes Patients discharged back to the primary care sector had a significantly higher mean age than those did not (48.6 vs. 42.7 year-old, p=0.049) (Table 5). In addition, those who required specialized investigation were older (53.3 vs. 46.0, p=0.05) than those who did not.
There were no significant age differences between patients referred for ?ncertain diagnosis" (p=0.42) and those ?eferrals to public secondary specialist care" (p=0.47). Discussion This study has demonstrated that the majority of patients referred from AEDs can be managed in the primary care setting by adopting this FMSC model of care. This new model achieved a low referral rate to the secondary care sector (13.7%), and an apparently low rate of utilization of specialized investigations (17.3%). The majority of referral cases could be referred back to the primary care sector (73.4%) thus allowing patients to be followed-up in the community, either public or private, after an average number of only 2.60 visits. As one of the key benefits of primary care consists of high accessibility and utilization for the majority of our population,15 these results potentially imply a very efficient means of handling referrals where the referring doctors identify cases requiring assessment by secondary care specialists. The effect of our model on cost, patient satisfaction, and long-term health outcomes needs to be further determined. While there was no gender difference found in the outcomes measured in this study, we have found that those discharged back to the primary care sector tended to be of an older age than those not discharged back, which was the same as for those who required specialized investigation. These interesting results could be explained by a number of doctor or patient-related factors. The lower discharge rate back to the primary care sector for the younger age patients could be due to the fact that they had conditions that needed further specialist assessment or management. The higher investigation rate in the older patients was potentially due to the presence of more conditions requiring further investigations. It may also represent different attitudes and perceptions of health care demand across different patient age groups,16-18 which would require further exploration in a larger-scale study. Our study has some limitations. These data were collected in a cross-sectional manner and we did not have a thorough prospective follow up. Only outcomes regarding health service utilization were collected and these should be better supplemented by clinical outcomes to allow assessment of the FMSC model more comprehensively. Besides, these outcomes could only act as a reference since there is lack of a control group i.e. a similar clinic not adopting this FMSC model within the same cluster (Kowloon West region) for direct comparison, or similar groups of patients receiving care from the medical specialist OPD. Furthermore, the fact that an average of only 2.60 visits was needed for FMSC to conclude one referral could have a number of reasons apart from the success of this new FMSC approach with the necessary back up of specialized investigation tools. Critics might argue that the presenting complaints in our patients could be relatively minor and hence resulted in early discharge or conclusion, or that our family physicians in this clinic were of exceptional standard and hence our result could not be generalized. Further studies may be needed to address these weaknesses. In summary, this study has demonstrated the efficiency of FMSC model in managing referrals from AED. The key components of running a high-quality and cost-effective primary care system to be evaluated, therefore, should also consist of the system of its operation, Public-Private Interface (PPI) and further development of a shared care concept among different sectors. This FMSC model may also be jointly run adopting a wider multi-disciplinary team of professionals in various specialties. These may involve inter-departmental collaborative approach and support from Government and various policy-making stakeholders. Conclusion These results suggest a new model as an efficient means of enhancing integration of primary health care in Hong Kong. Further studies could be conducted to assess the cost-effectiveness of this FMSC model, and a more vigorous process and outcome evaluation of the newer initiative. Key messages
Martin C S Wong, MBChB, MPH (CUHK), FRACGP, FHKCFP S W Mercer, MBChB, MSc, PhD (Cantab), FRCGP (UK) S M Griffiths, MB BChir, FFPHM (UK), FRCP (Lond, Edin), FHKCCM Alvin C Y Chan, MBChB, FRACGP, FHKCFP, FHKAM (Fam Med) Yuk-kwan Yiu, MBBS (HK), FRACGP, FHKCFP, FHKAM (Fam Med) Wai-keung Kwan, MBBS (HK), FHKAM (Med), FRCP (Edin), FRCP (Glasg) Correspondence to: Dr Martin C S Wong, 4/F School of Public Health, Prince of Wales Hospital, The Chinese University of Hong Kong, Shatin, NT, Hong Kong SAR. References
|
|