|
June 2016, Volume 38, No. 2
|
Update Article
|
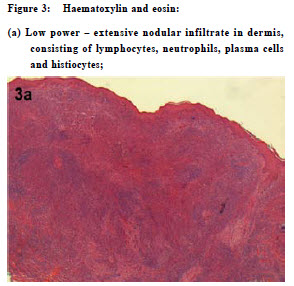
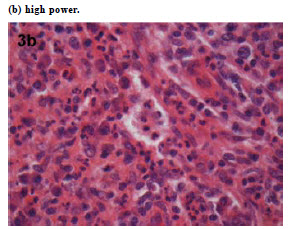
Hyperpigmented nodular plaques – a clinicopathological case studyMKA Basra, KS Chen, SM Andrew, AC Chu, AW Macfarlane HK Pract 2016;38:66-69 Summary Cutaneous Rosai-Dorfmann Disease or sinus histiocytosis is a rare, benign usually self resolving condition of unknown aetiology that in its typical form presents with massive lymphadenopathy with extra-nodal involvement. Skin is the most common extra-nodal site of involvement and pure cutaneous disease is exceptionally rare. Skin lesions usually present as dyspigmented nodules and plaques. 摘要 Rosai - Dorfman皮膚病,或稱竇道組織細胞增生症,是一種罕 見、病因不明而可自身緩解的良性疾病。其典型癥狀呈巨大 淋巴結腫脹和結外侵犯。皮膚是最常受到結外侵犯的組織, 但單純在皮膚出現病症則非常罕見。皮損表癥常為色素異常 的結節和斑塊。 Clinical findings A 63-year-old man presented with a 6-month history of hyperpigmented nodular plaques on his thighs, developing one month after returning to the United Kingdom from a holiday in Barbados. They stung but was not itchy. The patient was born in Mauritius, of Indian descent, but had lived in the United Kingdom for 40 years. He had a history of hypertension and Type 2 diabetes mellitus with retinopathy, but none of relevant medication, allergy or recent insect bites. On examination, there were rather firm hyperpigmented plaques with early nodular change on the lateral aspect of the left thigh and the posterior aspect of the right thigh (Figures 1 and 2). Systemic examination was normal. There was no evidence of lymphadenopathy or hepatosplenomegaly. Laboratory tests including inflammatory markers, immunoglobulins, immunoelectrophoresis, cholesterol and fasting lipids were all unremarkable. Subsequently, he developed similar hyperpigmented papules and nodules on the arms. A skin biopsy was taken from a plaque on the left thigh, and histological examination showed an extensive dermal infiltrate of mixed inflammatory cells including histiocytes, Touton giant cells, lymphocytes and plasma cells (Figure 3). Cutaneous Rosai-Dorfman disease without lymphadenopathy was diagnosed. Discussion Rosai-Dorfman disease (RDD) in its typical form is also known as sinus histiocytosis with massive lymphadenopathy (SHML). It is a rare , benign condition of unknown aetiology and unpredictable clinical course first described in 1969 by Juan Rosai and Ronald Dorfmann.1,2 Immune dysregulation or infection with viral or bacterial agents remain unproven aetiological hypotheses. The disease in its classic form is characterised by massive lymph node enlargement (particularly in the neck), high ESR, leucocytosis, neutrophilia and polyclonal hypergammaglobulinaemia.3 In around 43% of cases2 the disease may also involve extranodal sites such as the skin, genitourinary system, bones, lower respiratory tract, oral cavity, soft tissues and central nervous system.3 In general, the prognosis depends on the number of lymph node groups and extranodal sites affected. Although the skin is the commonest extra-nodal site to be involved in patients with classic RDD, purely cutaneous involvement without SHML, as in our case, is exceptionally rare. The differential diagnosis to consider with similar presentation of cutaneous lesions is cutaneous lymphoma, Langerhans' cell histiocytosis, reticulohistiocytomas, panniculitis and cutaneous lesions of leukemia. In comparison to typical RDD it seems commoner in an older age group, in Asian and Caucasian populations (cf. Africans), and in females.4 Brenn et al5 have reported probably the largest series of cutaneous RDD, with skin lesions presenting most commonly as papules or nodules with dyspigmentation, as in the case reported here. Other cases have presented with acneiform, pustular or clinically vasculitic lesions.6,7 It has been suggested that purely cutaneous RDD, although histopathologically indistinguishable from skin involvement in systemic RDD, is a distinct clinical entity in terms of its epidemiology and tendency to remain localised to the skin even on long term follow-up.5
Histopathologically, RDD is characterised by a mixed inflammator y cell infiltrate within which there are S100 - positive his tiocytes that exhibit emperipolesis.5 Emperipolesis occurs when a histiocyte (macrophage) engulfs another cell – usually a lymphocyte, plasma cell or neutrophil – by phagocytosis (Figure 4). It is not specific to RDD but may also be seen occasionally in other conditions including lymphoma and Langerhans’ cell histiocytosis. Immunohistochemical studies of RDD reveal that the phagocytic histiocytes are positive for S100 as well as macrophage markers such as CD68 and CD148, but negative for CD4 and CD1a. Although RDD is generally considered to be a benign, usually self-resolving condition, active treatment is often required , particularly in the presence of organ involvement, lymphadenopathy or disfigurement. Treatments such as ciclosporin, vinca alkaloids, interferon and etoposide have been used but with poor response rates. More successful therapies reported in the literature include radiotherapy, surgical debulking, systemic steroids and thalidomide. Our patient had no systemic involvement clinically and presented only with skin lesions. Initially he was treated with topical 0.05% betamethasone with 3% salicylic acid (Diprosalic ointment®), but without improvement. Sixteen months of azathioprine 75mg/ day (approximately 1 mg/kg/day) led to some flattening of the nodules but no further resolution, and higher doses were responsible for significant elevations in hepatic transaminases. He was then treated for three years with a combination of azathioprine 50 mg/day plus methotrexate 10 mg/week, increasing to 20 mg/ week in the last year. This produced virtually complete resolution of the skin changes, with complete flattening of all nodules, resolution of the plaque-like changes and significant improvement in the hyperpigmentation. Treatment was stopped at this point. Response to combination therapies incorporating methotrexate have been reported in the literature for classic RDD. These include regimens combining methotrexate with 6-mercaptopurine9, corticosteroids10 or other chemotherapeutic drugs.11 A recent report demonstrated a good response to azathioprine alone in a difficult case of RDD with central nervous system involvement.12 Conclusion In conclusion, to our knowledge, this is the only reported case of cutaneous RDD successfully treated with a combination of methotrexate and azathioprine. The patient is being followed up at six-monthly intervals and his skin has remained clear without any recurrence for six months.
References
|
|