Research & Publications > The Hong Kong Practitioner > Clinical Quiz

Clinical Quiz (Please login 'Member Area' for online submission of latest issue)
Clinical Quiz December 2024
A 59-year-old lady complained of a painful lesion over the base of her right index finger
Dr. Adrian KC Cheng
|
Readers are invited to participate in the Clinical Quiz*. Simply answer the question, fill in the reply slip and return it to the College by 24 Feb 2025. Each reader is allowed to submit one entry only.
*Note: There would be no prize award for this issue while sponsorship for Clinical Quiz has been ended in September 2020 issue. The answer of the Clinical Quiz for this issue will be announced in the next issue. Thank you for your support.
|
Clinical history:
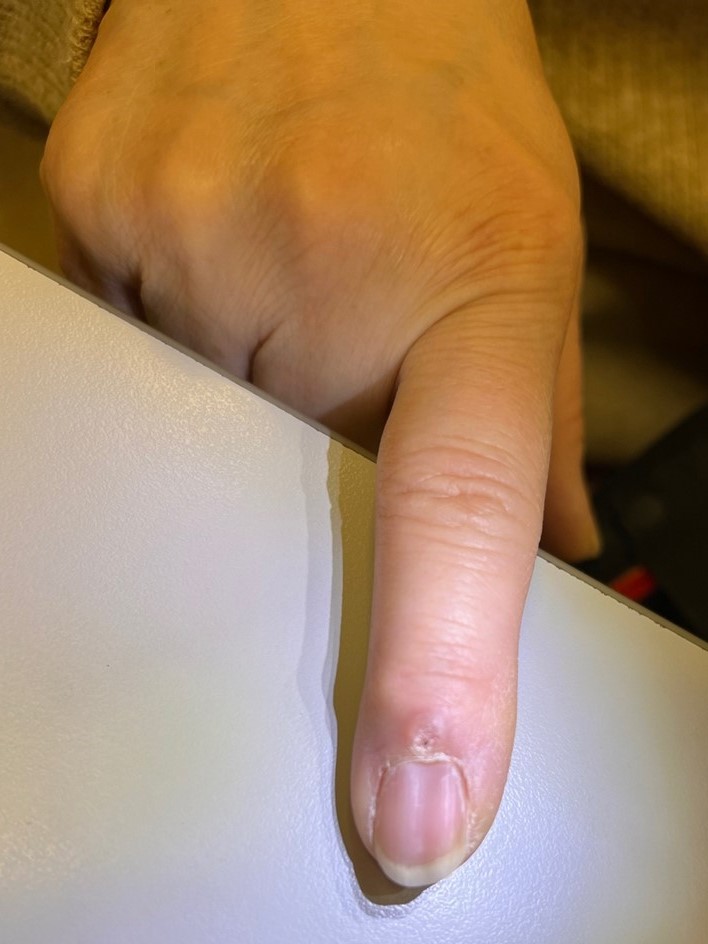
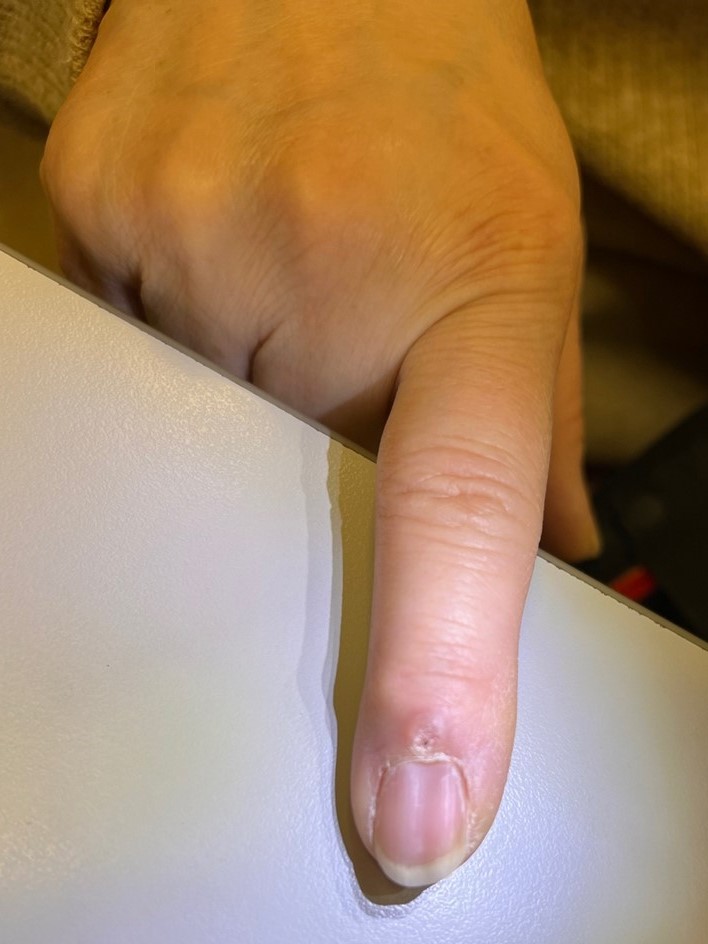
A 59-year-old lady complained of a painful lesion over the base of her right index finger. The lesion ruptured multiple times, expressing a sticky fluid that subsequently reaccumulated. On examination, a 3mm shiny papule was observed over the base of the right index finger nail, with a longitudinal groove extending along the nail plate distal to the papule.
What is the diagnosis?

| A. | Digital myxoid cyst |
| B. | Periungual viral wart |
| C. | Onychomatricoma |
| D. | Periungual fibroma |
Answer:
A. Digital myxoid cyst
A digital myxoid cyst (DMC), or myxoid pseudocyst, presents as a translucent nodule on the dorsal digit between the distal interphalangeal joint and the proximal nail fold, most commonly on the radial fingers.
DMCs result from mucoid degeneration of connective tissue and/or joint fluid leakage from an osteoarthritic distal interphalangeal joint via a communicating canal. Despite being termed a "cyst", histological analysis reveals mucinous fluid accumulation without an epithelial lining, making "myxoid pseudocyst" a more accurate designation.
DMCs near the proximal nail fold may exert pressure on the nail matrix, causing a longitudinal groove in the nail plate. Mucinous discharge may intermittently relieve pressure on the nail matrix, leading to irregular nail depression.
Diagnosis is typically clinical, with high-resolution ultrasonography or MRI aiding in ambiguous cases. MRI reveals a communicating canal with the distal interphalangeal joint in over 80% of cases.
Management options include digital compression, cryotherapy, sclerosant injection, or surgical excision. Spontaneous discharge increases the risk of septic osteoarthritis, warranting intervention.
The slide and the question were prepared by:
Dr. Adrian KC Cheng, MBBS(HK), MRCP(UK), MSc GEOR (CUHK), FHKCP, FHKAM (Medicine)
Specialist in Dermatology & Venereology;
Associate Consultant,
Division of Dermatology, Department of Medicine, Queen Mary Hospital, Hong Kong SAR
Back